ABSTRACT:
Implant rehabilitation of the severely atrophic maxilla presents a surgical and prosthetic challenge to even the most experienced clinician. The “graft-less” approach with the use of zygomatic implants is gaining acceptance. The purpose of this case series is to present the successful protocols employed in our Toronto clinic for the management of severe maxillary atrophy using a graft-less approach.
INTRODUCTION
Implant restoration of missing teeth has become common place in North America and the developed world. Standard (alveolar) implant placement and restoration are now a part of most dental specialties and some general dental training programs. Treatment of the majority of implant cases is now considered routine. However, the presence of atrophy of the alveolar ridge often requires hard and/or soft tissue augmentation, which can reduce case acceptance and complicate management. Rehabilitation of the severely atrophic fully edentulous maxilla can present a significant challenge to even the most experienced clinician. The purpose of this case series is to present the successful protocols employed in our Toronto clinic for the management of severe maxillary atrophy using a “graft-less” approach.
There is no denying the need for sound protocols in managing this patient population. While the incidence of complete edentulism is on the decline [Slade et al., 2014], this medical burden remains significant. In 2010, the prevalence of U.S. edentulism was projected at 12.2 million and future projected prevalence of edentulism for the U.S. population by 2050 is 8.6 million adults [Slade et al., 2014].
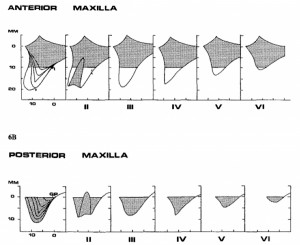
Those with edentulism are and should be considered amputees. The dental amputee possesses a unique problem: ongoing and progressive loss of anatomy due to the process of residual ridge resorption (RRR). This catabolic change in the alveolus that occurs subsequent to tooth loss has been well described and classified (Nakamato, 1968; Atwood, 1971; Lekholm & Zarb, 1985; Cawood and Howell, 1988; Farina et al., 2011). Bone changes associated with RRR are most significant within the first three to six months, (Atwood, 1963; Schropp et al., 2003; Farina and Trombelli, 2011). Unfortunately, RRR continues indefinitely. These dimensional changes seem to be dependent on number of extrinsic (smoking, number of teeth removed) and intrinsic (location in the mouth, individual) factors (Saldanha et al., 2006; Farina and Trombelli, 2011; Pramstraller et al., 2011; Pietrokovski, 1975; Schropp et. al., 2003). The most widely used classifications systems for alveolar atrophy are those of Lekholm & Zarb (1985) and Cawood & Howell (1988). In our clinic, we classify individuals using clinical and radiographic evaluation and stratify patients based on the latter (Fig. 1) along with the “zones of the maxilla” classification system (Bedrossian, 2011; Fig. 2).

Fixed implant-supported rehabilitation of the maxillary arch must take into account prosthetic and surgical considerations. In this type of solution, the support, stability, and retention of the prosthetic is provided solely by the implant fixtures. When implants are placed soon after dental extraction and early in the resorptive phase, the need for grafting can be reduced, if not eliminated. Classically, longstanding edentulism of the maxilla was associated with the need for staged rehabilitation involving extensive autogenous grafting and placement of eight or more implants. More recently long-term predictability has been shown with a minimum of four implant fixtures when rehabilitating the completely edentulous maxilla with a fixed prosthetic (Maló et al., 2011). When planning implant placement, it is of particular importance to ensure fixture placement allows for control and management (reduction but not necessarily elimination) of the prosthetic cantilever forces (Krekmanov et al., 2000). Posterior alveolar atrophy with pneumatisation of the maxillary sinus often limits the ability to spread implant placement posteriorly. Proposed options for implant placement in the presence of maxillary alveolar atrophy include the use of short and/or narrow implants (Maló et al., 2015), reconstruction (Clayman, 2006; Chiapasco et al., 2007; De Santis et al., 2012; Pieri et al., 2012) or a graft-less approach utilizing tilted alveolar implants or specialized / basilar bone implant placement such as zygomatic (Brånemark et al, 2004; Malo et al., 2014; Maló et al., 2015) or pterygoid (Graves, 1994; Balshi et al., 2013; Curi et al., 2015) implants. Rather than reconstruct resorbed alveolar bone, zygomatic and pterygoid implants anchor into local craniofacial bone. This graft-less approach proceeds to anaplastically replace the composite (dental, hard and soft tissue) defect. To date, there is no direct randomized trial to evaluate the options available. However, when assessing the literature individually, zygomatic implants have a level of predictability in the short- and long-term comparable with that of staged reconstruction with delayed standard (alveolar) implant placement. When taking into account the benefits of immediate function and return to esthetics, comfort, reduced morbidity, and reduced cost, zygomatic implant placement is the preferred approach for these authors when faced with inadequate bone volumes for alveolar implant placement in the completely edentulous individual.
The patient workup includes a complete medical history, clinical evaluation (intra- and extra-oral), and radiographic evaluation. The radiograph of choice is the orthopantomogram (OPG), which serves as a screening image. When the degree of horizontal atrophy is in question, or when zygomatic implant placement is planned, a cone-beam CT (CBCT) is considered mandatory. For individuals that will require zygomatic implant placement, the evaluation and screening of the sinuses for pathology is critical. Any indication of sinus pathology (on history, clinically, or radiographically) must initiate a referral to an Otolaryngology – Head & Neck Surgeon and management of the osteomeatal complex must be completed prior to proceeding with zygomatic implant placement.
Proper management of severe maxillary atrophy requires a highly skilled team with open communication and a close working relationship. Our team is comprised of an oral and maxillofacial surgeon, otolaryngologist, restorative dental practitioner and laboratory technician. When compared to alveolar implants, the surgical skill involved in the placement of zygomatic implants requires a high level of understanding of the local anatomy and specialized surgical training. While risks with zygomatic implant placement are uncommon, should one develop it can carry significant consequence for the patient. Risks described can occur intraoperatively (surgical misadventure into the orbit or infratemporal fossa, bleeding, labial laceration, poor primary stability, zygomatic fracture), and postoperatively (hematoma, paresthesia, pain and tenderness to palpation, sinusitis, dehiscence/thread exposure, oral-antral fistula, implant failure, zygomatic-cutaneous fistula, zygomatic implant fracture (Aparicio et al., 2012).
In our clinic, individuals with inadequate bone volume for standard implant placement are managed using one of three graft-less techniques: 1) the angled (“All-on-4”®) implant technique; 2) a combination of two to four anterior alveolar implants with a single zygomatic and/or pterygoid implant placement in the posterior region; or 3) four zygomatic implants alone (“Quad Zygoma”). Below we outline the treatment of three patients that have undergone zygomatic implant placement in our clinic.
Case #1:
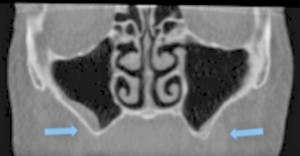
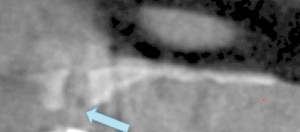
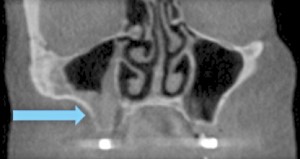
Placement of a unilateral zygomatic implant in addition to alveolar and pterygoid implants to replace a terminal dentition
A 67-year-old non-smoking female presented seeking options to restore her maxillary and mandibular arches. The medical history was significant for hypothyroidism, rheumatoid arthritis and depression. Daily medications included Synthroid, Wellbutrin as well as vitamin supplements (vitamin D, calcium and magnesium). Clinical and radiographic examination confirmed a terminal dentition with moderate to severe generalized horizontal bone loss (Figs. 3 and 4). The remaining maxillary alveolus displayed advanced horizontal and vertical atrophy. More detailed radiographic imaging with CBCT (Figs. 5 and 6) confirmed advanced atrophy with Cawood & Howell class VI at the posterior and Cawood & Howell class III at the anterior maxilla. The maxillary sinus displayed bilateral pneumatisation and significant anterior extension. There was inadequate zone 2 and 3 bone for standard implant placement. The osteomeatal complex appeared unobstructed (Fig. 7) and, with the exception of mucosal thickening (Fig. 5), no other significant sinus pathology was noted. The patient was presented with the treatment options and elected to proceed with an implant supported maxillary and mandibular fixed prosthesis. The patient was given a preoperative prescription for Amoxicillin 500mg (q8h for 8 days, beginning 1 day prior to surgery), Chlorhexidine oral rinse (0.12%, BID, rinse for 60 sec., NPO for ½ hour after) and Naproxen (250mg q12h for five days, beginning two hours prior to surgery). Under IV sedation and local anaesthetic, all remaining maxillary and mandibular teeth were extracted. Four standard implants (Nobel Biocare®, NobelSpeedy™, Regular Platform) were placed in the mandible following the angled (All-on-4®) implant technique. In the maxilla two standard implants were immediately positioned in the anterior region (Nobel Biocare®, NobelSpeedy™, Regular Platform) and the left pterygoid plate (Nobel Biocare®, NobelActive™, Regular Platform). In the right maxilla a zygomatic implant (Nobel Biocare®, Brånemark System® Zygoma, TiUnite™ surface) was placed. All implants achieved an initial insertion torque of more than 35 Ncm. Multi-unit abutments (Nobel Biocare®) were selected and positioned and torqued to manufacturer recommendations. An all-acrylic transitional full arch prosthesis consisting of 12 teeth was immediately secured onto the abutments and the implants were immediate loaded with a fixed prosthesis. The transitional prosthesis was maintained for the duration of the healing phase (six months). A modified soft diet was recommended during this period. ISQ (Osstell) measurements were taken at time of placement and at follow-up. After six months, integration was confirmed clinically, radiographically, and with ISQ. The final titanium-reinforced acrylic profile prosthetic was fabricated and inserted (Figs. 8 and 9). Continued follow-up occurs at six-month intervals.





Case #2:
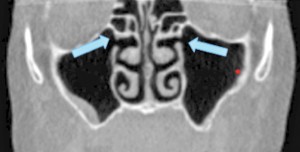
Placement of 4 Zygomatic Implants (“Quad-Zygoma”) in a patient with complete maxillary edentulism
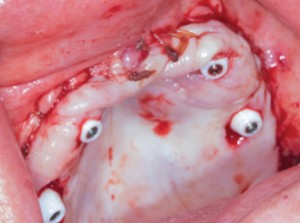
A 64-year-old non-smoking female presented seeking treatment for her edentulous maxillary arch with the expectation for a fixed prosthesis. The mandibular arch was previously restored with a removable partial denture. Her medical history was significant for controlled diabetes (type II), hypertension, irritable bowel syndrome, osteoarthritis, chronic pain and depression. Daily medications include Pantoprazole, Decetel, Domperidone, Oxycodone, Ramipril, Ezetrol, Metformin, Trazadone, Celebrex, Lactulose and Cymbalta. Clinical and radiographic (OPG and CBCT) evaluation revealed advanced acquired maxillary atrophy with bilateral maxillary sinus pneumatisation (Figs. 10, 11 and 12). Classification for this patient was (Cawood & Howell VI) in the anterior and (Cawood & Howell V) in the posterior maxilla with inadequate zone 1, 2, or 3 bone (Bedrossian, 2011) for alveolar implant placement. The anterior maxillary residual ridge had developed idiopathic hyperplasia due to combination syndrome. The osteomeatal complex was patent and no other sig sinus pathology was noted. The patient was given a preoperative prescription for Amoxicillin 500mg (q8h for eight days, beginning one-day prior to surgery) and Chlorhexidine oral rinse (0.12%, BID, rinse for 60 sec., NPO for ½ hour after). Surgical treatment took place under deep intravenous sedation with administration of local anaesthesia. Due to the lack of anterior maxillary bone volume, four zygomatic implants (Nobel Biocare®, Brånemark System® Zygoma, TiUnite™ surface) were placed. Implant placement followed the ZAGA (Aparicio, 2011) technique (Fig. 13). In this particular case, platelet-rich fibrin (PRF) was placed on the exposed threads (Boora et al., 2015) (Fig. 14). The incision location allowed for a flap design that maintains a labial cuff of keratinized mucosa (Figs. 13 and 15). Primary tissue closure was achieved with 3-0 chromic gut suture. All implants obtained an initial insertion torque of more than 45 Ncm. Fixtures were fitted with zygomatic multi-unit abutments (Nobel Biocare®). An OPG was taken once the patient was stable (Fig. 16) to ensure full seating of the zygomatic multi-unit abutments. An all-acrylic transitional full arch prosthesis consisting of 12 teeth was immediately secured onto the abutments (Figs. 17 and 18) and the implants were placed in immediate load with a fixed prosthesis. A soft diet was recommended during the healing period. At two weeks, the patient returned for follow-up where tissues and the prosthesis were evaluated and a T-scan (Tekscan, Inc.) was used for occlusal equilibration (Fig. 19). A soft tissue complication of dehiscence of the suture line was noted at the two-week re-evaluation. This was resolved with the suture re-approximation. No further complications have occurred to date.








Case #3:
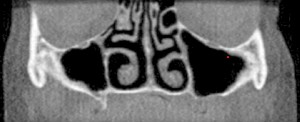
Placement of four zygomatic implants to replace failing implant-supported maxillary full arch prosthesis
A 63-year-old non-smoking female presented with a late failure of a full arch prosthesis using the angled (All-on-4®) implant technique. The medical history was significant for Hypothyroid, Lymphedema, and ADHD. Medications included Thyroxin and Adderall. Clinical Evaluation revealed three failed maxillary implants. Radiographic analysis (OPG and CBCT) confirmed a severely atrophic maxillary anterior and posterior ridge (Cawood & Howell class IV anterior and class VI posterior) with inadequate bone in zones 1, 2 and 3 (Bedrossian, 2011) for alveolar implant placement (Figs. 20 and 21). The failed implants had caused significant destruction of the remaining alveolus in the premaxilla (Fig. 21). Possible pathology was noted in the right maxillary sinus (Fig. 22). The osteomeatal complex appeared unobstructed. Consultation with an Otolaryngologist was arranged preoperatively and no preparatory treatment was indicated. The patient was given a preoperative prescription for Clavulin 500mg (q8h for 8 days, beginning one-day prior to surgery) and Chlorhexidine oral rinse (0.12%, BID, rinse for 60 sec., NPO for half-hour after). Surgical treatment took place under deep intravenous sedation with administration of local anaesthesia. The three existing maxillary implants were removed and four zygomatic implants (Nobel Biocare®, Brånemark System® Zygoma, TiUnite™ surface) were placed following the ZAGA (Aparicio, 2011) technique (Figure 23). Flap design and suturing were done at the labial aspect to preserve keratinized mucosa. All implants achieved an initial insertion torque of more than 35 Ncm and were fitted with zygomatic multi-unit abutments (Nobel Biocare®). An all-acrylic transitional full arch prosthesis consisting of 12 teeth was immediately secured onto these implants for the patient to wear during the healing phase. A modified soft diet was recommended during the six-month healing period. Evaluation at three months shows excellent soft tissue adaptation (Fig. 23).



CONCLUSION:
To date, we have managed 42 patients with a total of 80 zygomatic implants. Our experiences have been favorable. More importantly our patients report a high level of satisfaction. Prosthetic success rates are 100 percent. Complications encountered include: dehiscence (4%), oral antral fistula (2.5%), sinusitis (2.5%) and implant failure (1.3%).
The use of zygomatic implants for the rehabilitation of complete and partial maxillary edentulism is a predictable treatment modality with minimal morbidity. The execution, however, requires a multi-disciplined team and a high level of surgical and prosthetic expertise.OH
Dr. Peter Gioulos is a board certified Oral & Maxillofacial Surgeon practicing in two private practice clinics: Crescent Oral Surgery (Richmond Hill, Aurora & Toronto; www.crescentoralsurgery.com) and Chrysalis Dental Centre (Toronto; www.ChrysalisCanada.com). He maintains a hospital appointment at Rouge Valley Health System–Centenary Site. While he practices the full scope of his specialty, his clinical focus is immediate implant placement and restoration and zygomatic implant placement.
Dr. Allan Vescan is a board certified Otolaryngology — Head and Neck Surgeon with subspecialty expertise in Rhinology and Skull Base Surgery. He practices at Mount Sinai Hospital, University Health Network — Toronto Western Site and Centric Health — Don Mills Surgical Center. He received his Medical Doctorate (MD) in 2001 from the University of Western Ontario, followed by the completion of his Otolaryngology residency program in 2006 from the University of Toronto. He received his Oncologic Skull Base Fellowship from the University of Pittsburgh in 2007. He also holds a Master’s of Science from the Institute of Medical Science, University of Toronto.
Dr. Steven Bongard obtained his DDS degree from The University of Toronto Faculty of Dentistry in 1986. He is the founder and clinical head of Chrysalis Dental Centres in Toronto Canada (www.ChrysalisCanada.com) and United Smiles Centres in London UK (www.unitedsmilecentres.co.uk) both of which are implant only facilities focused on “same day” dental implant solutions. Dr. Bongard has extensive experience in implant placement, bone grafting procedures, as well as the prosthetic component of implant restoration. He has published and lectured both nationally and internationally on implant placement, All-on-4®, “Guided” implant surgery, single tooth, and alternative implant solutions. Clinically, his recent focus has been on developing innovative implant solutions for predictable same-day treatment of the severely atrophic edentulous patient.
Oral Health welcomes this original article.
REFERENCES:
1. Aparicio C. A proposed classification for zygomatic implant patient based on the zygoma anatomy guided approach (ZAGA): a cross-sectional survey.Eur J Oral Implantol. 2011;4(3):269-75.
2. Aparicio C, González-Martín O, Manresa C, Ouazzani.Complications. In: Aparicio C, editor. Zygomatic Implants: The Anatomy-Guided Approach. United Kingdom: Quintessence; 2012. p.244-250.
3. Balshi TJ, Wolfinger GJ, Slauch RW, Balshi SF. Brånemarksystem implant lengths in the pterygomaxillary region: a retrospective comparison. Implant Dent. 2013;22(6):610-2.
4. Bedrossian E. Systematic Pretreatment Evaluation of the Edentulous Maxilla. In: Bedrossian E, editor. Implant Treatment Planning For the Edentulous Patient: A Graftless Approach to Immediate Loading. Missouri: Mosby Elsevier; 2011. p.37-40.
5. Brånemark PI, Gröndahl K, Öhrnell LO, Nilsson P, Petruson B, Svensson B, et al. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J of Plast Recon Surg. 2004; 38(2):70–85.
6. Boora P, Rathee M, Bhoria M. Effect of Platelet Rich Fibrin (PRF) on Peri-implant Soft Tissue and Crestal Bone in One-Stage Implant Placement: A Randomized Controlled Trial. J ClinDiagn Res. 2015; 9(4):ZC18-21
7. Cawood JL, Howell RA. A classification of the edentulous jaws.Int J Oral Maxillfac Surg. 1988; 17: 232-6.
8. Chiapasco M, Brusati R, Ronchi P. Le Fort I osteotomy with interpositional bone grafts and delayed oral implants for the rehabilitation of extremely atrophied maxillae: a 1-9-year clinical follow-up study on humans. Clin Oral Implants Res. 2007; 18(1):74-85.
9. Clayman L. Implant reconstruction of the bone-grafted maxilla: review of the literature and presentation of 8 cases. J Oral Maxillofac Surg. 2006; 64(4):674-82.
10. Curi MM, Cardoso CL, Ribeiro Kde C. Retrospective study of pterygoid implants in the atrophic posterior maxilla: implant and prosthesis survival rates up to 3 years. Int J Oral Maxillofac Implants. 2015; 30(2):378-83.
11. Davó R, Pons O. Prostheses supported by four immediately loaded zygomatic implants: a 3-year prospective study. Eur J Oral Implantol. 2013; 6(3):263-9.
12. De Santis D, Trevisiol L, D’Agostino A, Cucchi A, De Gemmis A, Nocini PF. Guided bone regeneration with autogenous block grafts applied to Le Fort I osteotomy for treatment of severely resorbed maxillae: a 4- to 6-year prospective study. Clin Oral Implants Res. 2012; 23(1):60-9.
13. Farina R, Trombelli L. Wound healing of extraction sockets. Endo Topics. 2011; 25(1):16–43.
14. Farina R, Pramstraller M, Franceschetti G, Pramstraller C, Trombelli L. Alveolar ridge dimensions in maxillary posterior sextants: a retrospective comparative study of dentate and edentulous sites using computerized tomography data.Clin Oral Implants Res. 2011; 22(10):1138-44.
15. Graves SL. The pterygoid plate implant: a solution for restoring the posterior maxilla. Int J Periodontics Restorative Dent.1994; 14(6):512-23.
16. Krekmanov L, Kahn M, Rangert B, Lindström H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000; 15(3):405-14.
17. Lekholm U, Zarb GA. Patient selection and preparation. In: Branemark PI, Zarb GA, Albrektsson T editors. Tissue integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintessence; 1985. p.199–209.
18. Maló P, de AraújoNobre M, Lopes A, Ferro A, Moss S. Extramaxillary surgical technique: clinical outcome of 352 patients rehabilitated with 747 zygomatic implants with a follow-up between 6 months and 7 years. Clin Implant Dent Relat Res. 2015; 17Suppl 1:e153-62.
19. Maló P, de AraújoNobre MA, Lopes AV, Rodrigues R. Immediate loading short implants inserted on low bone quantity for the rehabilitation of the edentulous maxilla using an All-on-4 design. J Oral Rehabil. 2015; 42(8):615-23.
20. Maló P, Nobre Md, Lopes A. The rehabilitation of completely edentulous maxillae with different degrees of resorption with four or more immediately loaded implants: a 5-year retrospective study and a new classification. Eur J Oral Implantol. 2011; 4(3):227-43.
21. Maló P, Nobre Mde A, Lopes A, Ferro A, Moss S. Five-year outcome of a retrospective cohort study on the rehabilitation of completely edentulous atrophic maxillae with immediately loaded zygomatic implants placed extra-maxillary. Eur J Oral Implantol. 2014; 7(3):267-81.
22. Pieri F, Lizio G, Bianchi A, Corinaldesi G, Marchetti C. Immediate loading of dental implants placed in severely resorbed edentulous maxillae reconstructed with Le Fort I osteotomy and interpositional bone grafting. J Periodontol. 2012; 83(8):963-72.
23. Saldanha JB, Casati MZ, Neto FH, Sallum EA, Nociti FH Jr. Smoking may affect the alveolar process dimensions and radiographic bone density in maxillary extraction sites: a prospective study in humans.J Oral Maxillofac Surg. 2006; 64(9):1359-65.
24. Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23(4):313-23.
25. Slade GD, Akinkugbe AA, Sanders AE. Projections of U.S Edentulism prevalence following 5 decades of decline.J Dent Res 2014; 93(10):959-65.









