Introduction
Dental implants remain the gold standard for the replacement of one or more missing teeth.1,2 In an edentulous arch, all the teeth are missing and rehabilitation with implants provides the patient a significant improvement in function, aesthetics and quality of life.3 Implant bars, where a bone-affixed bar supports and retains the denture instead of it resting on the patient’s soft tissues,4 are predictable and cost-effective options. Implant bars are fabricated through subtractive manufacturing or milling5 and delivered to patients through a complex clinical workflow.6 The milling process has numerous disadvantages in terms of cost, efficiency and environmental footprint.7,8
As metal additive manufacturing (AM) matures, it presents a novel opportunity for the fabrication of implant bars, offering a process that promises to reduce both the time and cost9,10, ultimately improving treatment accessibility. Moreover, AM provides a more sustainable approach, specifically through a more conservative lattice-structured design, reducing dentistry’s environmental footprint11,12. This report explains the workflow developed for the fabrication of additive manufactured solid & lattice-structured titanium alloy dental implant overdenture bars.
Methods & Materials
Milled Bar
A dental implant metal bar was sourced from Panthera Dental (Quebec QC). This bar was part of a patient education model, consisting of the implant bar, model of the patient’s lower jaw (mandible) and the simulated soft tissue. (Fig. 1) The implant bar was milled from medical grade titanium alloy (Ti6Al4V) on a fully robotic CNC machine at a 4.0 manufacturing facility. The bar was monobloc, with no welded areas and no porosity, and had a very accurate and passive fit with the dental implants on the model. The STL file of the bar was provided by Panthera Dental.
Fig. 1

Design
The implant bar design file (STL) was reviewed by ADEISS (Additive Design in Surgical Solutions Centre, London ON) to evaluate the design for additive manufacturing. Review for AM determined that the STL design required modifications to incorporate through-holes of 2 mm in diameter for implant placement, and the overall implant bar structure needed to be thickened to account for AM post-processing where surface finishing was required.
Two implant bar designs were generated for AM; the first design was a solid structure to replicate a standard implant bar, and the second design incorporated an internal latticed pattern within the bar component. The lattice design was created using standard computer aided design (CAD) software functions, with circular cross-sectional geometry (Ansys Spaceclaim 3D Modeling Software, Concord MA). (Figs. 2 & 3) Additionally, for the lattice-designed bars, drainage holes of 0.75 mm diameter were incorporated into the anterior walls, such that non-consolidated powder from the AM process could be cleaned from the samples in post-processing. (Fig. 3) The final STL designs for AM were confirmed to match the dimensions of a comparative milled bar sample.
Fig. 2
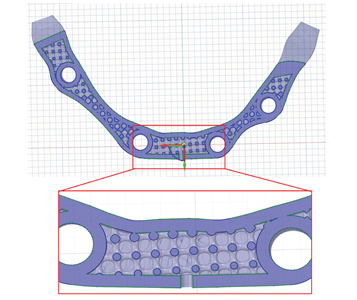
Fig. 3

Selective Laser Melting (3D Printing) and Post-Processing
STL designs for AM were prepared for printing in medical-grade titanium alloy (Ti6Al4V). Printing was done using selective laser melting technology with the Renishaw AM 400 system (Renishaw PLS, Gloucestershire, United Kingdom). The 3D printer utilizes alloy powder within the range of 30-50µm in diameter, with a 400W laser of 70µm diameter, to consolidate the final implant bars within a 250 mm x 250 mm x 250 mm build volume. A total of 18 implant bars (12 solid, 6 internal lattices) were fabricated with machine print time of 7 hours and 6 mins.
Following the printing process, the implant bars on the build plate were cleaned using compressed air. Air was cycled across the build plate and through drainage holes until loose powder could not be further expelled. Following powder clearance, the implant bars were exposed to standard heat treatment in a vacuum furnace, removed from the build plate, and surfaces finished. All implant bars were processed to a polished mirror finish (<1µm Ra) using hand tooling. (Fig. 4) The final processing step included cleaning of all implant bars using ADEISS ultrasonic cleaning methods to remove any remaining alloy powder and polishing agents.
Fig. 4

Discussion
The AM workflow fabricated dental implant bars that were all evaluated to be clinically acceptable, based on the fit with the original patient model and subsequently with the fit of a denture. (Fig. 5) Based on the number of implant bars that can be fabricated from the single build plate, and the total time of fabrication and cost, the AM fabrication workflow suggests meaningful advantages over conventional milling of implant bars. Further research is being conducted through 4-point testing and will be released shortly.
Fig. 5

Conclusions
The AM workflow for both solid and latticed-structured dental implant bars indicated that AM is a suitable, and perhaps a superior, fabrication workflow for implant bars. Further research and metrics are needed. Workflows that provide improved cost savings, efficiency and sustainability should be explored, not only to improve the patient experience, but also to enhance the sustainability of the profession.
Oral Health welcomes this original article.
Acknowledgements: Panthera Dental provided the milled implants bars and models. All design, manufacturing, and post-processing for AM were completed by the Additive Design in Surgical Solutions Centre (ADEISS Inc.). Alien Milling Technologies provided the Ivotion denture. This research was funded by an International Congress of Oral Implantologists (ICOI) IDREF grant. Special thanks to Dr. Yara Hosein for above and beyond assistance.
References
- Alaqeely, R., Babay, N., & AlQutub, M. (2020). Dental implant primary stability in different regions of the Jawbone: CBCT-based 3D finite element analysis. The Saudi dental journal, 32(2), 101-107.
- Kämmerer, Palarie, V., Schiegnitz, E., Hagmann, S., Alshihri, A., & Al-Nawas, B. (2014). Vertical osteoconductivity and early bone formation of titanium-zirconium and titanium implants in a subperiosteal rabbit animal model. Clinical Oral Implants Research, 25(7), 774–780. https://doi.org/10.1111/clr.12175
- Bramanti, E., Matacena, G., Cecchetti, F., Arcuri, C., & Cicciù, M. (2013). Oral health-related quality of life in partially edentulous patients before and after implant therapy: A 2-year longitudinal study. ORAL & implantology, 6(2), 37.
- Scrascia, R. Tissue support and Implant retention Overdenture in mandible: a simply, smart and predictable treatment.
- Lin, Chou, J.-C., Metz, M. J., Harris, B. T., & Morton, D. (2015). Use of intraoral digital scanning for a CAD/CAM-fabricated milled bar and superstructure framework for an implant-supported, removable complete dental prosthesis. The Journal of Prosthetic Dentistry, 113(6), 509–515. https://doi.org/10.1016/j.prosdent.2015.01.014
- Ortensi, L., Stefani, R., Lavorgna, L., Caviggioli, I., & Vitali, T. (2018). A Digital Workflow for an Implant Retained Overdenture: A New Approach. Biomed. J. Sci. Tech. Res, 6.
- Anadioti, Musharbash, L., Blatz, M. B., Papavasiliou, G., & Kamposiora, P. (2020). 3D printed complete removable dental prostheses: a narrative review. BMC Oral Health, 20(1), 343–343. https://doi.org/10.1186/s12903-020-01328-8
- Baba. (2016). Materials and Processes for CAD/CAM Complete Denture Fabrication. Current Oral Health Reports, 3(3), 203–208. https://doi.org/10.1007/s40496-016-0101-3
- Revilla-León, M., Meyer, M. J., & Özcan, M. (2019). Metal additive manufacturing technologies: literature review of current status and prosthodontic applications. Int. J. Comput. Dent, 22, 55-67.
- Yakout, M., Elbestawi, M. A., & Veldhuis, S. C. (2018). A review of metal additive manufacturing technologies. In Solid State Phenomena (Vol. 278, pp. 1-14). Trans Tech Publications Ltd.
- Tang, Mak, K., & Zhao, Y. F. (2016). A framework to reduce product environmental impact through design optimization for additive manufacturing. Journal of Cleaner Production, 137, 1560–1572. https://doi.org/10.1016/j.jclepro.2016.06.037
- Tang, Dong, G., Zhou, Q., & Zhao, Y. F. (2018). Lattice Structure Design and Optimization With Additive Manufacturing Constraints. IEEE Transactions on Automation Science and Engineering, 15(4), 1546–1562. https://doi.org/10.1109/TASE.2017.2685643
About the Author
 Les Kalman is an educator & medical device researcher focusing on additive manufacturing and software. He remains active with externally-funded research and has published and presented internationally. He has been recognized as a Fellow with the AO, ACD, IADFE; Diplomate (ICOI); Schulich Alumni of Distinction & a CES Innovation Award Honoree.
Les Kalman is an educator & medical device researcher focusing on additive manufacturing and software. He remains active with externally-funded research and has published and presented internationally. He has been recognized as a Fellow with the AO, ACD, IADFE; Diplomate (ICOI); Schulich Alumni of Distinction & a CES Innovation Award Honoree.












