Introduction: The Digital Revolution in Dentistry
Whether or not a clinician is working under the model of an in-house chairside milling solution or a more traditional lab-based relationship, digital scanner capture for crown and bridge restorations offers significant advantages over impression based capture – especially when prescribing digitally manufactured restorations.
Many esthetic restorative materials are available for use with CAD/CAM based models. For basic esthetic C&B, clinicians need not start with more than a few standard digital materials in their ‘bag of tricks’, but they should become comfortable prescribing these products with a high degree of specificity. As clinicians become more comfortable prescribing these products, additional digital materials can be added.
This article will explore the use of some more common digital C&B materials currently in use (Zirconia and Lithium Disilicate glass ceramic) highlighting restoration indications based on patient requirements from the authors point of view.
The Digital Workflow Differs from Practice to Practice
Any digital workflow for C&B starts with an intraoral scan. For some practice models, it will make sense to hold on to the restoration design, milling, sintering, and characterization, skipping the commercial lab entirely. For others, this complete model can make ‘going digital’ seem daunting.
There is a common misconception that in order to offer digital CAD/CAM dentistry, a practitioner must offer chairside milling and on-site processing. This is not the case. Digital capture can now be easily delivered via the cloud to your off-site digital based laboratory for processing and manufacture.
It is already the case that some practices employ a combination of these models. Perhaps on-site or chairside milling for singles and simpler cases, cases that require faster turnaround, and off-site commercial processing and manufacture for more complex multiples, implants or less time sensitive cases.
Digital Restorations – The Inevitable Solution
Over the past decade or so, there has been a shift in designing lab-based restorations from the traditional model of stone dies, and wax added toward the Computer Animated Design (CAD) model. This shift toward computer-based design is not unique to the dental industry.
CAD design software have become increasingly sophisticated, allowing for more detailed restoration design control. Furthermore, these systems help address the issue of variability between lab technicians. With the advent of CAD, we will rely less on the “hands and eyes” of any one individual technician.
Why Intraoral Digital Scanning?
It has been established that current generation intraoral scanners are appropriately accurate for digital capture in conventional crown and bridge. 1,2 The advantages to direct intraoral digital scanning are only evident once a clinician understands the laboratory steps used to manufacture their prescribed restorations.
For example, if a clinician is making a traditional rubber base wet (analog) impression and prescribing a zirconia (digital) crown, the laboratory is using a digital process to manufacture that restoration. That means that they are digitizing the impression, or more likely scanning a stone model of the case in order to work in a CAD platform, and ultimately will manufacture (mill) the final product. The same can be true for lithium disilicate cases if a CAD workflow is employed by the laboratory.
Unfortunately, in this example, many of the inherent potential inaccuracies associated with an analog workflow are being realized unnecessarily (impression material handling, length of time from impression to pour, shipping and handling issues, powder water ratios of stone, model preparation, etc.). If the ‘impression’ were captured digitally with an intraoral scanner, then the case is scanned into the CAD platform directly – without the potential problems associated with the analog workflow. If a clinician’s lab is manufacturing their restorations digitally, it would be wise to consider a transition to intraoral digital scanning.
Fig. 1
CAD digital workflow is less physically demanding on the technician.

Fig. 2
Intraoral scanning allows a direct path to working in CAD, skipping the potential inaccuracies of wet impressioning, shipping, and stone model fabrication.
Fig. 3
PFZ–feldspathic ceramic being applied to a zirconia framework.

Digital Restorations – The Workhorses
Zirconia Restorations:
Commercial Laboratory produced zirconia restorations are typically designed using CAD and manufactured by dry milling discs of raw zirconia. The raw zirconia is then infiltrated with color and heat sintered. The resulting restoration can be completed with stain and glaze or can be veneered with feldspathic ceramic – porcelain fused to zirconia(PFZ). This layering process is often necessary in esthetic areas to impart character to the restoration. As with traditional PFM, chipping of the veneering ceramic can occur. Careful framework design principles are required to minimize feldspathic veneering ceramic from chipping. 3 Furthermore, with PFZ care must also be taken to properly manage the thickness of the framework and veneering layers 4, and to properly control the thermal residual stresses generated when heating and cooling a restoration. 5 It is noteworthy that when properly processed, PFZ restorations have similar survival rate to traditional PFM. 6,7
The advantages of zirconia as a restorative material are primarily realized when used in the monolithic form.
Monolithic zirconia restorations can be stained, glazed, and/or highly polished. When highly polished, zirconia provides an extremely strong 8 and non-abrasive restorative solution 9,12 – much stronger and less abrasive as compared to PFM. 10,11 Recently, zirconia products with increased translucency and pre-shaded gradients have been introduced to the marketplace. The result is an Esthetic tooth colored restoration with the following characteristics:
- Esthetic Tooth Colored with no unsightly framework
- Moderately Translucent Differing translucenciesavailable
- Strong Traditional Zirconia–Over 1200 MPa (Higher Translucency products are closer to 750 MPa)
- Tough 4 to 5 MPa.m
- Non-abrasive Similar characteristics to Enamel (must be highly polished)
Fig. 4
Multiple crowns milled form raw zirconia disc.

Fig. 5
Milled raw zirconia (larger) beside color infiltrated, sintered zirconia (shrunken).

Fig. 6
Completed monolithic zirconia restoration after stain, glaze and high polish.

Lithium Disilicate Restorations:
Commercial laboratory produced Lithium disilicate restorations can be designed using CAD or by employing a traditional wax-added technique. Those designed in CAD are typically wet milled in a ‘blue block’ form then crystallized. CAD designed restorations may also be printed in wax. Wax patterns (analog or digital) are typically invested and hot-pressed. Feldspathic ceramic can be fused to Lithium Disilicate to impart character to the restoration but as with PFZ, many variables must be properly controlled to avoid chipping of the veneering ceramic. Lithium Disilicate restorations are typically stained and glazed, and/or highly polished. The result is a highly esthetic tooth colored restoration with the following characteristics:
- Highly Esthetic Tooth Colored with no unsightly framework
- Highly Translucent13 Differing translucencies available
- Moderate Strength when bonded 360MPa CAD- 450 MPa Pressed
- Moderately Tough8 2.8 MPa.m
- Low-abrasiveness Similar characteristics to Enamel (must be highly polished)
Fig. 7
Lithium disilicate (eMax) CAD is purchased in ‘blocks’ and wet milled.

Fig. 8
Milled lithium disilicate CAD pre crystalization.

Fig. 9
Lithium disilicate post crystalization–stained, glazed & highly polished.

Fig. 10
Four crowns for the same case – all with slightly different characteristics.
Left to Right: monolithic, highly polished zirconia/monolithic, highly polished zirconia, stained and glazed/monolithic highly polished translucent zirconia, stained and glazed/monolithic lithium disilicate CAD stained and glazed.

What to use Where?
In order to simplify the transition toward the use of digital restorations for basic C&B, a clinician should consider focusing on the two main products highlighted above. Although there are many other appropriate products in the marketplace, the availability, versatility and ease of use of Zirconia and Lithium Disilicate provide an excellent starting point. Considering a patients’ esthetic requirement and overall force factors will then assist in deciding which of these digital products to prescribe. Speaking in general terms, the more beautiful a restoration is, the weaker it is. For this reason, clinicians should prescribe their restorations with a high degree of specificity while maintaining a realistic expectation of the final esthetic outcome. Listed below are appropriate digital product options based on location followed by cases demonstrating clinical application of each.
Digital Product Options – Crowns
- Second Molar
- Monolithic Zirconia highly Polished, Stain and Glaze(S&G) optional
- First Molar
- Monolithic zirconia Highly polished, selective S&G
- Monolithic translucent Zirconia Highly polished, selective S&G
- PFZ vestibular veneering only, Highly polished, selective S&G
- Monolithic Lithium Disilicate, selective S&G
- Premolar
- Monolithic Translucent Zirconia highly polished, selective S&G
- Optionally monolithic lithium Disilicate, selective S&G
- Anterior
- Lithium Disilicate with Vestibular Veneering, S&G
- Optionally Translucent PFZ with Vestibular veneering, S&G
- Optionally monolithic lithium Disilicate, S&G
Digital Product Options – Bridges
- Posterior
- Monolithic Zirconia highly Polished, selective Stain and Glaze (S&G)
- Optionally PFZ with vestibular
- Veneering, highly polished, selective S&G
- Anterior 3 Units
- PFZ with Vestibular Veneering, S&G
- Optionally Monolithic translucent Zirconia Highly polished, S&G
- Anterior over 3 units
- PFZ with Vestibular Veneering, S&G
- Optionally Monolithic Zirconia, S&G
Clinical Cases
CASE 1
Fig. 11
Pre-operative condition #16.

Fig. 12
Core and preparation #16, DO resin #15.

Fig. 13
Virtual model ready for CAD design. CAD designed restoration.

Fig. 14
Milled translucent zirconia and printed die.

Fig. 15
Highly polished occlusal surface.

Fig. 16
Stained and glazed vestibular surface. Monolithic translucent zirconia – strong esthetic result.

Monolithic translucent zirconia crown #16
- 61-year-old female.
- Cc: Cracked tooth #16
- Patient with high esthetic demand
- Moderate force factors
Case 2
Fig. 17
Pre-operative condition #46 and #47.

Fig. 18
Virtual model ready for CAD design. CAD designed restorations.

Fig. 19
Highly polished monolithic zirconia #46 and #47.

Fig. 20
Very strong, moderately esthetic result.

Monolithic Zirconia Crowns
- 62-year-old male
- Cc: “My back teeth are crumbling. I want this repair to last forever!”
- Low Esthetic demand, high expectation
- High force factors
Case 3
Fig. 21
Pre-operative – incisal breakdown.

Fig. 22
Pre-operative – excessive lingual erosion.

Fig. 23
Virtual model ready for CAD design.

Fig. 24
#12 #11 #21 #22 restored to full contour.

Fig. 25
Lithium Disilicate crowns veneered with feldspathic ceramic, bonded – moderate strength, highly esthetic.

Lithium Disilicate Crowns Veneered with Feldspathic Ceramic
- 25-year-old female
- Cc: My front teeth are chipping
- Previous history of eating disorder
- High esthetic expectation
- Low force Factors
Case 4
Fig. 26
Pre-operative condition – severe thinning observed.

Fig. 27
Pre-operative condition–#11 #21 lingual wear.

Fig. 28
Restorations designed in CAD.

Fig. 29
Monolithic Lithium Disilicate crowns bonded. #11 #21 Restored to full form and function.

Monolithic Lithium Disilicate Crowns
- 53-year-old male
- Cc: “My front teeth are thinning chipping – attrition”
- High esthetic expectation
- Moderate Force Factors
Case 5
Fig. 30
Pre-operative condition–high force factors.

Fig. 31
Foundation restorations prepared for intraoral scan.

Fig. 32
Virtual model for CAD design and monolithic zirconia ready for milling.

Fig. 33
Zirconia milled and processed with printed dies.

Fig. 34
Monolithic zirconia bridge cemented. high strength. Moderate esthetics.

Monolithic Zirconia Bridge
- 53-year-old male
- Cc: Back Bridge fell out. Implant is not an option financially
- Low esthetic expectation
- Extremely High Force Factors
Case 6
Fig. 35
Pre-operative condition, endodontically treated, highly discolored.

Fig. 36
Preparation and preparation shade.

Fig. 37
Low translucency Lithium Disilicate framework. Feldspathic ceramic to be added for character and shade development.

Fig. 38
Cementation day–final result.

Porcelain Fused to Low Translucency Lithium Disilcate Crown
- 88-year-old female
- Cc: front tooth keeps breaking
- Complex tooth shade and characterization
- Endodontically treated tooth, dark preparation shade
- Moderate force factors
Case 7
Fig. 39
Pre-operative condition. #12 deemed unrestorable.

Fig. 40
Extraction #12 and preparation, after healing and ovate pontic development.

Fig. 41
Digital model showing virtual die spacer.
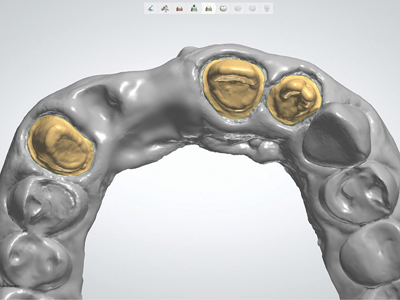
Fig. 42
CAD designed. PFZ framework–veneering ceramic limited primarily to non-functional surfaces.

Fig. 43
PFZ with feldspathic ceramic applied, stained, glazed and highly polished.

Fig. 44
Final PFZ bridge result – cementation day.

Porcelain Fused to Zirconia Bridge
- 56-year-old male
- Cc: existing front bridge loose
- esthetic zone
- Deep bite, parafunctional, High Force Factors
Case 8
Fig. 45
Pre-operative failing maxillary arch.

Fig. 46
Pre-operative loss of VDO–need to open VD and restore.

Fig. 47
Preparations and zirconia custom implant abutments.

Fig. 48
Intraoral digital scan.

Fig. 49
Final result: visible difference between Lithium Disilicate (anterior)and monolithic zirconia(posterior). All restorations highly polished on functional surfaces.

Fig. 50
Strong and adequately esthetic–anterior monolithic lithium disilicate. Posterior monolithic zirconia.

Mixed Case: Anterior Monolithic Lithium Disilicate Posterior Monolithic Zirconia
- 58-year-old male
- Cc: “My teeth are worn down”
- Moderate esthetic expectation
- High Force Factors
- Staged approach planned. Maxillary rehabilitation first
Conclusion
Digital scanner capture for crown and bridge restorations offers significant advantages over impression-based capture – especially when prescribing digitally manufactured restorations. Although there are many appropriate materials options available in the marketplace, a clinician can successfully transition to a digital material-based practice using a combination of zirconia and Lithium Disilicate. It is important, however, that the materials’ properties and indications be well-understood and be prescribed with a high degree of specificity. OH
Oral Health welcomes this original article.
Acknowledgement
Laboratory services for the above cases were provided by eNamel dental laboratory in Winnipeg, MB under the direction of Mr. Vlad Shpunt, RDT.
References
- Yang X1, Lv P2, Liu Y3, Si W4, Feng H5. Accuracy of Digital Impressions and Fitness of Single Crowns Based on Digital Impressions. Materials (Basel). 2015 Jun 29;8(7):3945-3957. doi: 10.3390/ma8073945.
- Muallah J, Wesemann C, Nowak R, Robben J, Mah J, Pospiech P, Bumann A. Accuracy of full-arch scans using intraoral and extraoral scanners: an in vitro study using a new method of evaluation. Int J Comput Dent. 2017;20(2):151-164.
- Guess PC1, Bonfante EA, Silva NR, Coelho PG, Thompson VP. Effect of core design and veneering technique on damage and reliability of Y-TZP-supported crowns. Dent Mater. 2013 Mar;29(3):307-16. doi: 10.1016/j.dental.2012.11.012. Epub 2012 Dec 8.
- White SN1, Miklus VG, McLaren EA, Lang LA, Caputo AA. Flexural strength of a layered zirconia and porcelain dental all-ceramic system. J Prosthet Dent. 2005 Aug;94(2):125-31.
- Al-Amleh B1, Neil Waddell J2, Lyons K2, Swain MV2.Influence of veneering porcelain thickness and cooling rate on residual stresses in zirconia molar crowns. Dent Mater. 2014 Mar;30(3):271-80. doi: 10.1016/j.dental.2013.11.011. Epub 2013 Dec 19.
- Sailer I, Fehér A, Filser F, Gauckler LJ, Lüthy H, Hämmerle CH. Five year clinical results of zirconia frameworks for posterior FPD. Int. J Prosthodont. 2007;20(4): 383-8.
- Pelaez J1, Cogolludo PG, Serrano B, Serrano JF, Suarez MJ. A four-year prospective clinical evaluation of zirconia and metal-ceramic posterior fixed dental prostheses. Int J Prosthodont. 2012 Sep-Oct;25(5):451-8.
- Silva LHD1, Lima E2, Miranda RBP2, Favero SS2, Lohbauer U3, Cesar PF2. Dental ceramics: a review of new materials and processing methods. Braz Oral Res. 2017 Aug 28;31(suppl 1):e58. doi: 10.1590/1807-3107BOR-2017.vol31.0058.
- Passos SP1, Torrealba Y, Major P, Linke B, Flores-Mir C, Nychka JA. In vitro wear behavior of zirconia opposing enamel: a systematic review. J Prosthodont. 2014 Dec;23(8):593-601. doi: 10.1111/jopr.12167. Epub 2014 Jun 24.
- Park JH1, Park S2, Lee K3, Yun KD4, Lim HP5. Antagonist wear of three CAD/CAM anatomic contour zirconia ceramics. J Prosthet Dent. 2014 Jan;111(1):20-9. doi: 10.1016/j.prosdent.2013.06.002. Epub 2013 Nov 5.
- Stober T1, Bermejo JL, Rammelsberg P, Schmitter M. Enamel wear caused by monolithic zirconia crowns after 6 months of clinical use. J Oral Rehabil. 2014 Apr;41(4):314-22. doi: 10.1111/joor.12139. Epub 2014 Jan 22.
- Janyavula S1, Lawson N, Cakir D, Beck P, Ramp LC, Burgess JO. The wear of polished and glazed zirconia against enamel. J Prosthet Dent. 2013 Jan;109(1):22-9. doi: 10.1016/S0022-3913(13)60005-0.
- Harada K1, Raigrodski AJ2, Chung KH2, Flinn BD3, Dogan S4, Mancl LA5. A comparative evaluation of the translucency of zirconias and lithium disilicate for monolithic restorations. J Prosthet Dent. 2016 Aug;116(2):257-63. doi: 10.1016/j.prosdent.2015.11.019. Epub 2016 Mar 17.
About the Author
 After completing a Bachelor of Science, Dr. Mollot obtained his D.M.D. degree from the University of Manitoba in 1997. He is a Fellow of the International Congress of Oral Implantologists and the Pierre Fauchard Academy. Dr. Mollot is an Evaluator for the National Dental Examining Board and is a member of the Seattle Study Club. Dr. Mollot practises general dentistry in a progressive group practise in Winnipeg, Manitoba. He has a special interest in digital restorative dentistry and dental implants.
After completing a Bachelor of Science, Dr. Mollot obtained his D.M.D. degree from the University of Manitoba in 1997. He is a Fellow of the International Congress of Oral Implantologists and the Pierre Fauchard Academy. Dr. Mollot is an Evaluator for the National Dental Examining Board and is a member of the Seattle Study Club. Dr. Mollot practises general dentistry in a progressive group practise in Winnipeg, Manitoba. He has a special interest in digital restorative dentistry and dental implants.
RELATED ARTICLE: One Appointment Crowns and Bridges
Follow the Oral Health Group on Facebook, Instagram, Twitter and LinkedIn for the latest updates on news, clinical articles, practice management and more!












