PATIENT: M, Age: 62, ASA II (pharmacological management of hypertension and high cholesterol).
CHIEF COMPLAINT: Patient presented for the fabrication of a mandibular implant supported fixed prosthesis, with implants having been placed 6 months ago.
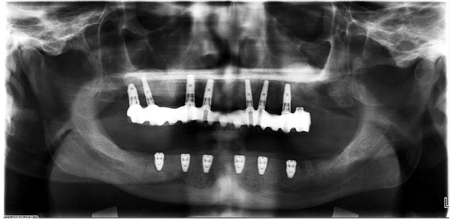
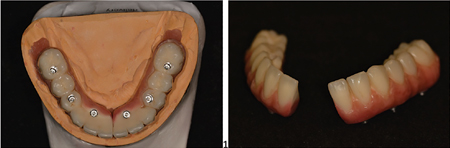
CLINICAL FINDINGS: Maxillary arch had a fixed implant supported prosthesis with implants in the 17, 16, 14, 13, 22, 23, 25 positions. The prosthesis was a titanium substructure with layered composite (Gradia) material. The mandibular arch consisted of an interim complete denture removable prosthesis relined with soft reline material, and 6 uncovered Straumann bone level implants (positions 36, 34, 32, 42, 44, 46) after 6 months of integration. (Fig. 1A) (Fig. 1B)
SOFT TISSUE: 2mm of attached tissue was present around each implant in the mandible. There was noted bone loss and recession around implants in the maxillary arch with thread exposure of 13 and 22, and moderate plaque accumulation was observed. Thin gingival tissue had grey discoloration show-through on the buccal of 13 and 22.
HARD TISSUE: Peri-implantitis was present at implants 17, 16, 13, and 22, with a prior history of implant failure at 26 site.
RADIOGRAPHIC FINDINGS: Localized peri-implantitis with bone loss on implant 16, 13, 22 and 24 was detected. Six Straumann BLT 4.8 x 8mm implants were present in the mandibular arch, evenly spread out with a flat platform. (Fig. 1C)
DIAGNOSIS: Peri-implantitis of 17, 16, 13 and 22. Moderate wear to the maxillary arch prosthesis, with a canted occlusal plane. Edentulism of the mandibular arch.
Fig. 1A

Fig. 1B

Fig. 1C
TREATMENT
The treatment plan consisted of refurbishment of the maxillary prosthesis and fabrication of a mandibular fixed prosthesis. Monolithic zirconia or a traditional metal-acrylic hybrid was considered, but it was decided to fabricate the prosthesis with a similar material as the maxillary to minimize potential wear issues. A final impression was taken of the mandibular arch with splinted open-tray impression copings for accuracy. Orthodontic wire and light-cured bis-acryl composite material was used to splint the impression copings prior to final impression with PVS and custom trays. A verification jig was fabricated on the master model using non-engaging temporary abutments and pattern resin, which was sectioned and luted back together after 24 hours to account for dimensional shrinkage. The verification jig was tried in the mouth and passive seating was confirmed with Sheffield test (one-screw test), intraoral evaluation confirming no rocking of the jig, and digital evaluation of abutment screws tightening in the last half turn. Radiographs were taken to confirm seating of the abutments. (Fig. 2) A mandibular occlusal rim was adjusted and pink wax was added to the maxillary arch to achieve an idealized occlusal plane, record the VDO, and determine positions of mandibular teeth for a trial setup. (Fig. 3) After successful tooth try-in, (Fig. 4) the mandibular setup was sent for fabrication of a milled titanium substructure. (Fig. 5). The mandibular titanium framework was inserted and checked for passive seating with no issues. Articulator mounting of the casts was confirmed intraorally with pattern resin, and then the maxillary arch prosthesis was removed for refurbishment along with adding the composite material to the prosthesis. (Fig. 6) Delivery of the maxillary prosthesis and the new mandibular implant supported fixed prosthesis was completed with no issues. (Fig. 7) Abutment screws were torqued to 35Ncm as per manufacturer recommendation, and retorqued after 15 minutes before being sealed with PTFE tape and composite plugs. Patient was asked to return after 2 weeks for post-delivery evaluation.
Fig. 2
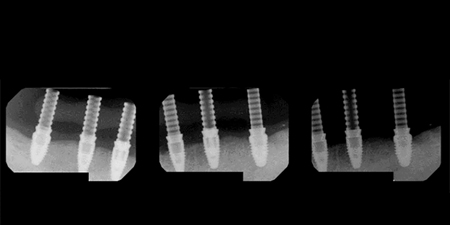
Fig. 3

arch for idealization of occlusal plane, incisal length, vertical dimension, and tooth positions.
Fig. 4

Fig. 5

Fig. 6

Fig. 7

COMPLICATIONS
The patient had the opportunity to test form and function for 2 weeks before re-evaluation. The patient approved of the occlusion, masticatory function, and esthetics of the prosthetics. However, he noted that there was an unusual pain in the mandibular arch when yawning. The pain was consistent whenever the patient yawned or intentionally opened to maximum opening, but was not present during standard masticatory function or speech. Patient reported that he felt a dull ache in the left posterior mandible with an intensity of 2 out of 10, and he was unable to specify if it was located by the 34 or 36 implant location. Extraoral examination demonstrated no tenderness to palpation in the muscles of the head and neck region. Intraoral examination was within normal limits, and both the 34 and 36 implants had no symptoms when attempting a reverse torque test at 35Ncm. It was also noted that the pain could be elicited when asking the patient to protrude the mandible as far as possible. The patient was noted to have an above average range of motion when opening (>65mm).
The possibility of mandibular flexure from having a splinted implant prosthetic from 36 to 46 was considered. A new verification jig was fabricated to test this hypothesis. Although pattern resin is commonly used for verification jigs, a long span will have slight flexibility iii that can bend with the mandible during movement. Instead, a verification jig was fabricated from plaster and temporary abutment cylinders. (Fig. 8A-D) The mandibular fixed prosthesis was removed, and then the plaster verification jig was inserted with the patient only opening 50% of his maximum range. Passive seating was confirmed with all abutments torqued into place, and no fracture of the plaster jig was noted. (Fig. 9) However, upon maximum jaw opening, the plaster jig fractured at the 32 abutment position and a space opened between the two pieces. The gap between the fractured plaster pieces decreased (Fig. 10) when returning to rest position. Re-opening of the gap was observed as well when comparing the rest position to the patient’s maximum protrusive position. (Fig. 11)
Fig. 8A

Fig. 8B
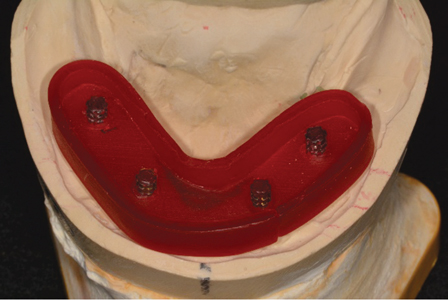
Fig. 8C

Fig. 8D

Fig. 9

Fig. 10
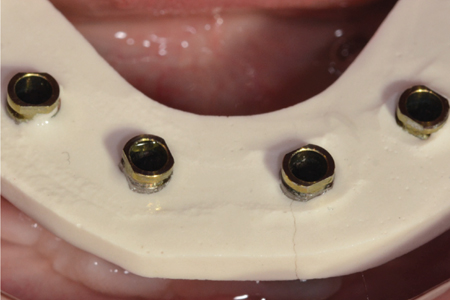
Fig. 11

fracture gap widens.
Based on these findings, it was concluded that the mandibular prosthesis would need to be sectioned. Sectioning the prosthesis would have minimal complications because of the presence of 6 implants with even anterior-posterior spread, along with the composite-layered titanium framework being easier to manipulate. If the prosthesis was monolithic zirconia or contained porcelain crowns, the cost of replacement would have been significantly higher. The prosthesis was sectioned between 31 and 41 (Fig. 12 A,B) to maintain cantilever forces in the least destructive area. An alternative would have been to section the prosthesis distal to the 33 or 43 if esthetics were a greater concern.
Fig. 12A, B
A. and from the front B.
The mandibular prosthesis was re-inserted and minor occlusal adjustments were completed at delivery. During the 2 week post-delivery evaluation, the patient reported to be asymptomatic with no pain when yawning or during protrusive movements. The mandibular prosthesis abutment screws were then re-torqued and screw channels obturated with composite plugs. (Fig. 13) The patient was placed on a regular 4 month recall schedule with a periodontist to maintain maxillary implants.
Fig. 13

CONCLUSION & DISCUSSION
Mandibular prosthetics that splint implants from molar to molar across the entire arch may be subject to forces of mandibular flexure. The 4 major types of mandibular deformation are described by Hylander as:
- Parasymphyseal bending: medial convergence related to the lateral pterygoids during jaw opening movements5,6
- Dorsoventral shear: shear forces related to the vertical component of the lateral pterygoid5,6
- Corporal rotation: torsion of the body about the long axis during the power stroke of mastication5,6
- Antero-posterior shear: shear forces related to the contraction of the masseter and temporalis muscles5,6
Often times, patients will report no issues when splinting a mandibular prosthesis across the arch. However, in the case of the reported patient, symptoms uniquely associated with yawning (mandibular opening >90% of maximum) led us to suspect mandibular flexure as a factor. This was confirmed through the use of a verification jig fabricated with a rigid and brittle material. Auditory and visual confirmation was obtained by the jig distortion that appeared when the mandible was within the last 20% of maximum opening or maximum protrusion. The elastic modulus of the commonly used pattern resin jig was not able to demonstrate this phenomenon. The long-term effects of mandibular deformation on periodontal bone levels and implant survival are unclear and there are few long term studies documenting it. This concern is not an issue in the tilted-implant treatment (“All-on-4”) commonly used in the mandibular arch because the implants have reduced anterior-posterior spread with cantilevered teeth distally.
In terms of material selection, the author would like to note one major disadvantage of the designed Gradia-composite layered titanium framework seen when comparing Fig. 7 (initial delivery) and Fig. 13 (re-delivery). During the span of approximately 6 weeks, the maxillary prosthesis was not removed and the composite material accumulated a moderate amount of staining and plaque in the short period of time. This design is not commonly used but was made in order to match the maxillary prosthesis that was fabricated 12 years prior.
The author would like to extend gratitude to Jesse and Frichtel Dental Labs (Pittsburgh, PA, USA) for their collaboration on the case.
Oral Health welcomes this original article.
References
- Assif D, Marshak B, Schmidt A. Accuracy of implant impression techniques. Int J Oral Maxillofac Implants. 1996;11:216–22.
- Papaspyridakos P, Kim YJ, Finkelman M, El-rafie K, Weber HP. Digital Evaluation of Three Splinting Materials Used to Fabricate Verification Jigs for Full-Arch Implant Prostheses: A Comparative Study. J Esthet Restor Dent. 2017;29(2):102-109.
- Sakaguchi, R. L., Ferracane, J. L., & Powers, J. M. (2019). Craigs restorative dental materials. St. Louis, MO: Elsevier.
- White GE. The Sheffield fitting test. Osseointegrated Dental Technology 1993:61. Quintessence Publishing Co Ltd, London.
- Hochstedler JL, Allen JD, Follmar MA. Temporomandibular joint range of motion: a ratio of interincisal opening to excursive movement in a healthy population. Cranio. 1996;14(4):296-300.
- Van eijden TM. Biomechanics of the mandible. Crit Rev Oral Biol Med. 2000;11(1):123-36.
- Law C, Bennani V, Lyons K, Swain M. Mandibular flexure and its significance on implant fixed prostheses: a review. J Prosthodont. 2012;21(3):219-24.
About the Author
 Jonathan C Wong is a fellow of the RCDC in Prosthodontics. He completed his undergraduate degree at Schulich School of Medicine and Dentistry, and then his Certificate in Advanced Prosthodontics at University of Pittsburgh School of Dental Medicine. Dr. Wong maintains associateships in private practice in Toronto and Kitchener-Waterloo.
Jonathan C Wong is a fellow of the RCDC in Prosthodontics. He completed his undergraduate degree at Schulich School of Medicine and Dentistry, and then his Certificate in Advanced Prosthodontics at University of Pittsburgh School of Dental Medicine. Dr. Wong maintains associateships in private practice in Toronto and Kitchener-Waterloo.












