EXTRACT
Fractured teeth are the mist common encountered dental emergency. This manuscript presents an anterior trauma case from initial presentation to final treatment through use of an interdisciplinary approach to diagnosis, planning, and treatment.
Introduction
A 22-year-old male patient presented to Scripps Center for Dental Care on emergency reporting having been hit in the face by a baseball. The patient reported that his front teeth and lower lip were in pain, but manageable. The lower lip was swollen and bleeding and the patient reported his upper front left tooth was broken. The patient informed us he was playing shortstop for the UCSD Baseball team and a ground ball had taken a bad bounce and hit him in the face (Figs. 1 & 2). The patient’s chief complaint was the discomfort from the trauma in the lower lip and the upper front left tooth.
FIGURE 1.Patient presentation day of trauma.

FIGURE 2. Figure 2: Lower lip laceration.

Case Report
A complete intra and extra oral examination was completed with evaluation of hard/soft tissues, TMJ, caries risk, periodontal health, occlusion, attrition, orthodontic class, crowding, and condition of existing dental restorations. Radiographs were obtained to evaluate supporting structures, existing dental restorations, and caries assessment. A photo series was acquired for records of pre-operative conditions and evaluation.
Periodontal health was good, all periodontal pocketing was 1-3 mm without any attachment loss. Mild attrition was present; patient was in Class I molar and canine relation and presented with slight post orthodontic relapse crowding of lower anterior teeth.
Upon examination, #9 presented with sulcular bleeding on the palate and a horizontal fracture in the gingival third of the facial and Class III mobility of the clinical crown, which displaced during oral examination (Fig. 3). Radiographically, #9 presented with a fracture (Fig. 4). No other mobility or fractures were observed. Lower lip presented with bleeding and swelling.
FIGURE 3. Fractured clinical crown.

FIGURE 4. Periapical radiograph showing fractured #9.
Abstract
Fractured teeth are the most common encountered dental emergency. This manuscript presents an anterior trauma case from initial presentation to final treatment through use of an interdisciplinary approach to diagnosis, planning, and treatment.
Diagnosis
Upon completion of examination, the patient was informed of all the clinical findings. #9 was diagnosed with a coronal fracture with pulpal exposure. Clinical crown fractures are the most common injuries reported in the permanent dentition, 26 to 76 percent, while crown root fractures comprise only 0.3-5 percent of the fractures.1, 2, 3
Due to the patients discomfort and pulpal exposure, a pulpectomy was diagnosed and completed at the time of presentation. After completion of the pulpectomy, a cone beam computed tomography (CBCT) scan was acquired to determine the extent of the fracture. The scan revealed a coronal fracture extending apical to the crest of the alveolar bone
on the palate without any obvious signs of alveolus fracture (Fig. 5).
FIGURE 5. CBCT showing coronal fracture extending to alveolus.

A multidisciplinary evaluation was completed with restoring cosmetic dentist, endodontist, periodontist, oral surgeon, and orthodontist. The factors considered were the length of the fracture, biologic width invasion on the palate, the pulpal exposure, periodontal trauma, occlusion, and aesthetics.2, 3, 4
Treatment options were discussed with the patient and all questions answered. The treatment options included:
– Root canal therapy of #9 with periodontal crown lengthening with porcelain crown
– Root canal therapy of #9 with orthodontic extrusion and porcelain crown
– Extraction of #9 and fabrication of a fixed partial denture
– Extraction of #9 with dental implant placement and custom abutment and porcelain crown5, 6, 7, 8
Treatment Plan
The patient elected to proceed with extraction of the fractured tooth and immediate placement of a dental implant if possible. For the immediate need of treating the patient’s discomfort, a pulpectomy was completed. This treatment would provide the patient with immediate comfort and the implant would allow for replacing the fractured tooth without removal of otherwise healthy tissue and provide a very nice aesthetic result.
Discussion
Pre-operative photos and radiographs were initially acquired. 1.0cc 4% Septocaine with 1:100k epinephrine (Septodont, Lancaster, PA) was administered to ensure patient comfort during the pulpectomy. An anterior rubber dam clamp (Hu-Friedy Mfg. Co., Chicago, IL) was placed with rubber dam (Patterson Dental, St. Paul, MN) to isolate maxillary anterior teeth. The pulpal tissue was removed with a barbed broach (NTI-Kahia GmbH, Kahla, Germany) and canal was irrigated with sodium hypochlorite 5.25% (Patterson Dental, St. Paul, MN) then rinsed and dried with paper points (Patterson Dental, St. Paul, MN).9 Calcium hydroxide (Pulpdent Corporation, Watertown, MA) was placed in canal space and sealed with cavit-g (3M ESPE, St. Paul, MN).9 The clinical crown and the retained root were then etched with Scotchbond Etchant (3M ESPE, St. Paul, MN) 35% phosphoric acid for 15 seconds and rinsed and blotted to remove excess moisture. The displaced clinical crown was then bonded back on the retained root with 5th generation bonding, Adper Single Bond Plus Adhesive (3M ESPE, St. Paul, MN) and light cured for 20 seconds with an Elipar S10 (3M ESPE, St. Paul, MN).10, 11, 12 #9 was then adjusted to remain out of occlusion in all movements. Impressions (Algitec Alginate, Patterson Dental, St. Paul, MN) were then acquired for records and fabrication of a temporary to be worn after the extraction of the fracture tooth.
The patient returned one week later for extraction of the fractured tooth with the oral surgeon. 3.0cc 2% Lidocaine with 1:100k epinephrine (Septodont, Lancaster, PA) was administered and #9 was removed atraumatically with periotomes (Hu-Friedy Mfg. Co., Chicago, IL) preserving the bone and soft tissue (Figs. 6 & 7).13, 14 After curettage of the socket, the buccal plate was determined to be completely intact with adequate bone for immediate placement. The patient’s biotype was thick with minimal scalloping making the site more predictable for immediate placement.15, 16 A Nobel Active implant (Nobel Biocare, Zurich, Switzerland) 4.3 mm x 13mm was then placed toward the palatal aspect (Figure 8) with implant connection 1mm below the buccal bone achieving a torque of 35Ncm.17, 18, 19, 20, 21
FIGURE 6. Atraumatic extraction site.

FIGURE 8. Implant in palatal position (Nobel Biocare, Zurich, Switzerland).

Though adequate primary stability was achieved, the surgeon requested not to immediately load the implant, so a custom-healing abutment was fabricated along with an Essex (Dentsply Raintree Essix, York, PA) style temporary. The custom-healing abutment was then created with an engaging temporary abutment sleeve (Nobel Biocare, Zurich, Switzerland) along with composite (Filtek Supreme Ultra, 3M ESPE, St. Paul, MN) to reproduce the natural emergency profile from the implant collar to the marginal tissue.15, 17, 18 The custom abutment was seated and torqued to 15Ncm. Teflon was placed over the screw and composite was placed over the access. The clinical crown from the extracted tooth was then contoured with composite (Filtek Supreme Ultra, 3M ESPE, St. Paul, MN) and fit into an Essex retainer, which was fabricated from the initial maxillary model, and delivered to the patient to be worn as a temporary until the implant was ready for restoration.
The patient returned for follow up one and two weeks later without any complaints of discomfort. The tissue was pink and firm and the custom-healing abutment was clean and stable to gentle palpation (Fig. 9). The Essex temporary was verified and the fit was great.
FIGURE 9. Custom healing abutment in immediate implant 1 week post op.

The patient returned 10 weeks later for a tissue check and modification of the custom-healing abutment. The custom-healing abutment was removed gently and modified to guide the soft tissue as it healed. Modification was made every two weeks until the tissue reached the desired position (Figs. 10 & 11).
FIGURE 10. Custom healing abutment with healed soft tissue.

FIGURE 11. Implant site with developed soft tissue.

When the patient presented for final impressions, a pre-prosthetic cosmetic photo series was acquired along with shade photos of the hydrated teeth for the ceramist using VITA Classical Shade Guide (Vident, Brea, CA) (Fig. 12). The custom-healing abutment was removed and a closed tray impression coping was seated (Nobel Biocare, Zurich, Switzerland) and hand torqued.22 A radiograph was acquired to verify complete seat of impression coping.
FIGURE 12. Pre prosthetic photo series

Light body vinyl polysiloxane, Imprint 4 (3M ESPE, St. Paul, MN), was injected around the implant site and adjacent teeth and a full arch metal tray loaded with heavy body Imprint 4 was seated and held in place for four minutes. The impression was removed and verified. The impression coping was removed and replaced with the custom-healing abutment. A full lower arch impression was also acquired with Imprint 4 light and heavy body vinyl polysiloxane. A full arch bite registration was acquired with thixotropic vinyl polysiloxane, Blu-Mousse super-fast bite registration material (Parkell, Edgewood, NY). A Kois Dento Facial Analyzer (Panadent, Colton, CA) record was additionally acquired.
Zirconia was chosen for the custom abutment (Nobel Procera, Zurich, Switzerland) for its strength and lithium discilicate (Ivoclar Vivadent, Amherst, NY) was chosen for its strength and aesthetics for the final crown.23
The patient returned four weeks later for delivery of the custom abutment and crown. The healing abutment was removed and the implant was irrigated with 0.12% Chlorohexidine Gluconate (3M ESPE, St. Paul, MN). The custom abutment was delivered and hand torqued. A radiograph was acquired to verify complete seat. The final abutment was torqued to 35Ncm and teflon was placed over the screw access in the abutment.24 The crown was then tried in. The margins and contacts were verified and the occlusion was verified to ensure hypo occlusion in MIP and to ensure interferences were not introduced.25 The aesthetics of the crown were additionally evaluated for the hue, value, chroma, translucency, contours, line angles, and surface texture. The crown was delivered with a self adhesive resin, Unicem2 (3M ESPE, St. Paul, MN), with a one second flash light cure to aid in excess cement removal followed by a final cure of 20 seconds.
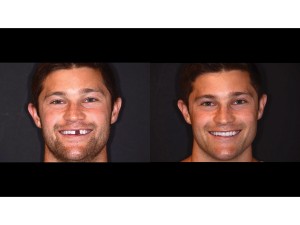
The patient returned two weeks later for post-prosthetic photos and follow up (Fig. 13).
FIGURE 13. Post Prosthetic photo series.

Conclusion
Implants are an excellent tooth replacement option. Having adequate hard and soft tissue remains to be one of the biggest challenges with implants, especially in the aesthetic zone. Immediate implants, when applicable, can be a great service to patients to reduce healing time and provide and excellent long-term restorative option. Interdisciplinary approach in diagnosis, treatment planning, and clinical treatment is very important and was a big part of the success of this case. OH
Dr. Marongiu is an Accredited Member of the American Academy of Cosmetic Dentsitry. He received his dental degree from Loma Linda University School of Dentistry and completed a GPR at West LA VA/UCLA. He is on medical staff at Scripps Memorial Hospital and is adjunct faculty at University of California, San Diego, School of Medicine, all while maintaining a full time multispecialty private practice in La Jolla, CA – Scripps Center for Dental.
In addition to the AACD, Dr. Marongiu is a member of the San Diego County Dental Society, the California Dental Association, the American Dental Association, and the Academy of General Dentistry.
Dr. Marongiu currently serves on the AACD Board of Directors and the CDA Board of Managers. He is also a delegate from the San Diego County Dental Society to the CDA House of Delegates and a delegate from the 13th District to the ADA House of Delegates. marongiu@gmail.com.
Oral Health welcomes this original article.
References
1. Andreasen JO, Andreasen FM, Andersson L. Textbook and color atlas of traumatic injuries to the teeth. 4th ed. Oxford: Blackwell; 2007.
2. Olsburgh S, Jacoby T, Krejci I. Crown fractures in the permanent dentition: pulpal and restorative considerations. Dent Traumatol. 2002 Jun;18(3):103-15.
3. Elias H, Baur DA. Management of trauma to supporting dental structures. Dent Clin North Am. 2009 Oct;53(4):675-89.
4. de Castro JC, Poi WR, Manfrin TM, Zina LG. Analysis of the crown fractures and crown-root fractures due to dental trauma assisted by the Integrated Clinic from 1992 to 2002. Dent Traumatol. 2005 Jun;21(3):121-6.
5. de Castro MA, Poi WR, de Castro JC, Panzarini SR, Sonoda CK, et al. Crown and crown-root fractures: an evaluation of the treatment plans for management proposed by 154 specialists in restorative dentistry. Dent Traumatol. 2010 Jun;26(3):236-42.
6. Subramanian K, Chogle SM. Medical and orofacial considerations in traumatic dental injuries. Dent Clin North Am. 2009 Oct;53(4):617- 26.
7. Poi WR, Cardoso L de C, de Castro JC, Cintra LT, Gulinelli JL, et al. Multidisciplinary treatment approach for crown fracture and crown-root fracture–a case report. Dent Traumatol. 2007 Feb;23(1):51-5.
8. Baratieri LN, Monteiro Júnior S, Cardoso AC, de Melo Filho JC. Coronal fracture with invasion of the biologic width: a case report. Quintessence Int. 1993 Feb;24(2):85-91.
9. John M Coulter, O Lee Wilson, Murray K Marks. Management of traumatic tooth injuries in the dental office. J Tenn Dent Assoc. 2014 Fall-Winter; 94)2): 31-37.
10. Hamouda IM, Samra NR, Badawi MF. Microtensile bond strength of etch and rinse versus self-etch adhesive systems. J Mech Behav Biomed Mater. 2011 Apr;4(3):461-6.
11. Castelnuovo J, Tjan AH, Liu P. Microleakage of multi-step and single-step bonding systems. Am J Dent. 1996 Dec;9(6):245-8.
12. Gallo JR, Comeaux R, Haines B, Xu X, Burgess JO. Shear bond strength of four filled dentin bonding systems. Oper Dent. 2001 Jan-Feb;26(1):44-7.
13. Sharma SD, Vidya B, Alexander M, Deshmukh S. Periotome aid to atraumatic extraction: a comparative double blind randomized controlled trial. J Maxillofac Oral Surg. 2015 Sep; 14(3):611-5.
14. Thomson PJ. Minimizing trauma in dental extractions: the use of the periotome. Br Dent J. 1992 Mar 7;172(5):179.
15. Park JB. Immediate placement of dental implants into fresh extraction socket in the maxillary anterior region: a case report. J Oral Implantol. 2010;36(2):153-7.
16. Gelb DA. Immediate implant surgery: three-year retrospective evaluation of 50 consecutive cases. The International J of Oral & Maxillofacial Implants. 1993, 8(4):388-399.
17. Stephen Chen, Ivan Darby, Eric Reynolds, John Clement. Immediate implant placement postextraction without flap elevation. Journal of Periodontology. Jan 2009, 80(1): 163-172.
18. Kan JY, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. The International J of Oral & Maxillofacial Implants. 2003, 18(2): 31-39.
19. Gintaras Juodzbalys, Hom-Lay Wang. Soft and hard tissue assessment of immediate implant placement: a case series. Clinical Oral Implants Research. April 2007 (18)2:237-243.
20. Devorah Schwartz-Arad, Gavriel Chaushu. Immediate Implant Placement: A procedure without Incisions. Journal of Periodontology. July 1998 (69)7:743-750.
21. Norton. The linfluence of insertion torque on the survival of immediately placed and restored single-tooth implants. Int J Oral Maxillofac Implants. 2011 Nov-Dec;26(6):1333-43.
22. Papaspyridakos P, Chen CJ, Gallucci GO, Doukoudakis A, Weber HP, Chronopoulos V. Accuracy of implant impressions for partially and completely edentulous patients: a systematic review. Int J Oral Maxillofac Implants. 2014 Jul-Aug;29(4):836-45.
23. Christensen GJ. Implant Abutment Material Choices. Clinicians Report. Kan 2013;6(1).
24. Moraguez OD, Belser UC. The use of polytetrafluoroethylene tape for the management of screw access channels in implant-supported prostheses. J Prosth Dent. 2010 Mar;103(3):189-91.
25. Gross MD. Occlusion in implant dentistry. A review of the literature of prosthetic determinants and current concepts. Aust Dent J. 2008 Jun;53 Suppl 1:S60-8.
RELATED ARTICLE: A Multidisciplinary Approach For The Esthetic Treatment Of Anterior Crown Fracture