Introduction: Old Job, New Tool
Since the 1950s, when x-ray photography came into widespread use in dentistry, the radiograph has been a dentist’s primary diagnostic tool.1 It is easy to see why: Only a tiny fraction of what a radiograph shows can be seen by the unaided eye.
In other branches of medicine, radiology is its own specialty; in dentistry, it is a sideline of the clinician, a brief stop on the way to prophylaxis and repair.
Accurate interpretation of dental radiographs is difficult. Images vary in quality and can be full of ambiguities. Not surprisingly, several studies have shown that different dentists, looking at the same radiograph, interpret features in different ways and arrive at different diagnoses and different estimates of the depth and severity of lesions.2 Forty percent of estimates of cavity depth are wrong. We miss between a quarter and half of periapical radiolucencies. In one study involving thousands of radiographs, three dentists were in full agreement about a given radiograph only four percent of the time.3 Patients sense this, and approach dentistry with a certain wariness.
About 15 years ago, radiologists working with cancer oncologists began using a new technology to assist them in interpreting radiographs of lungs and other internal organs.4 This new technology was what is broadly known as “artificial intelligence,” or AI for short. AI, in the form of digital image analysis, has now become an accepted tool in oncology, and has shown an ability to detect abnormalities that is equal, and sometimes superior, to that of human radiologists.5,6
It was only a matter of time before that same type of AI would be implemented in the world of dentistry, where interpretation of radiographs is so fundamental to clinical practice. The dental field turns out to be a fertile one for AI, which requires intensive “training” using vast amounts of data tagged by expert analysts. If ever there was a health discipline with vast amounts of data in existence, it is in the form of radiographs in dentistry. The proof has been in the practical performance of dental AI. As it does in oncology, digital image analysis matches or exceeds the performance of dental experts in detecting and identifying both normal and abnormal features.7
The Business Case for AI in Dentistry
A frequently cited Reader’s Digest article originally published in 1997 reported the experience of a writer who visited 50 dentists in 50 states and got almost that many diagnoses and treatment plans.8 As you would suspect, they diverged widely in complexity and cost. There is no way to know whether that article moved the needle on dental reputations, but it certainly resonated with the widespread perception that dentistry can be a very subjective business.
Scientifically conducted studies have yielded the same result; dental diagnosis is highly inconsistent – you might even say unreliable.
While some unscrupulous practitioners could profit from the ambiguity of radiographic evidence to foist unnecessary treatments on patients, most of us strive to bring as much accuracy and consistency of diagnosis into our work as we can. Digital image analysis can only help. It presents its results to both dentist and patient, chairside, as an image of the radiograph with areas of concern highlighted and tagged. As an aid to the dentist, it ensures that nothing will be overlooked while allowing him or her to make the necessary professional judgments about the importance of different criteria and how to proceed with treatment. As a service to the patient, it clarifies ambiguous imagery and conveys a reassuring impression of precision and objectivity. The AI-analyzed radiograph feels like a second opinion delivered in real time.
AI also has several advantages over human radiographers. One is sensitivity, a function of its ability to make extremely fine grayscale discriminations. Another is that it is never tired, inattentive, distracted, forgetful or rushed. In other words, it never makes careless mistakes. But perhaps the most important is that it is a tide that lifts all boats. It never stops learning. AI has the potential to incorporate the collective knowledge and experience of a vast number of practitioners and patients, and to make its power available to all.
Digital image analysis is not the only kind of AI that can be useful to dentists. To a greater degree than most other medical professionals, dentists are entrepreneurs. In private practice, they juggle the dual roles of business owners and care providers. AI and AI-related software can take on many of the routine tasks involved in running an office, simplifying the managerial side at the same time as it improves performance on the clinical side. Conveniently, as business owners dentists are not only in a position to benefit from AI, but also to make the decision to acquire it.
For DSOs, AI not only increases consistency in diagnosis, but also makes it possible to identify clinicians who tend to over- or under-diagnose certain conditions. In the context of access to a large array of patient records in different localities, it opens up the future option of longitudinal analyses of patients’ dental health over time, and of detecting potential relationships between dental health, general health, geography, nutrition and other environmental factors.
How it Works
It may seem hard to understand how a computer can be taught to recognize caries by showing it a lot of pictures of caries, but it is not that different from how we ourselves do it. Newborn babies, too, must learn to organize visual data into objects; they do not come into the world with built-in recognition of dogs, cats, and automobiles. The programming technology used in computer vision is called a “neural network”, because its structure and operation are broadly analogous to those of an animal or human nervous system.
Like the human retina with its rods and cones, the computer takes in a raw image in the form of a large collection of pixels. It finds relationships among them – edges, gradients, amounts and locations of color, light and dark, and so on – and compares those relationships with an internal catalog of object-related relationship sets, looking for a close match.
The hard part is creating that internal catalog in the first place. The process is called “deep learning”, a somewhat dramatic sounding term for finding mathematical commonalities in a large variety of visual records of the same class of thing. Having learned from 10,000 pictures of different cats, the computer can recognize any new cat, and will not be fooled by a catlike dog or other feline. The results are astonishingly precise. The computer will recognize not just any cat, but a particular cat; not just any face, but your face, even turned sideways, or in a crowd, or partly covered by your N95.
To train a machine learning system for use in dentistry, dental radiologists annotated thousands of radiographs. From studying those annotated radiographs, the AI learned to identify the visual signatures of a wide range of both normal and abnormal conditions. Of course, the annotators did not always agree on every point. When they differed, the AI recorded the uncertainty as a probability. The result is a machine that embodies the collective skill of a large team of expert radiograph readers and is capable of learning and refining its abilities by continuous feedback.
AI in Action
From a dentist’s standpoint, using AI technology to annotate x-rays can improve multiple areas of current frustration. For instance, a recent study conducted by the corporate consultancy L.E.K. ranked alleviating administrative burden and desire for better work/life balance as the primary drivers for job selection. AI can impact both. From the dental claims administrative side, annotated radiographs help to remove the subjective elements of claims review. More precisely, there are now objective measurements attached to a tooth, which removes the need for a reviewer to decide if a tooth is missing 40% or 50% tooth structure in order to adjudicate the claim. Inconsistency of claims review has traditionally been an area of contention for dentists, and AI allows for a streamlined, unbiased review to occur.
Additionally, feedback from clinicians working in practices supported by the US-based DSO, Sage Dental, which ran a pilot deployment of clinical AI software, unanimously reported that they felt less exhausted and experienced lower levels of job-related stress when using the software. Several reasons account for this. Dentists view well over 300 radiographs per day, on average. Statistical variability of diagnosis will occur based on everything from the time of day to how rushed the clinician is at the time of the exam. We live in a litigious climate, so the clinician’s worries about “missing things” is certainly a stressor. Add eye fatigue and other operative stresses, and the perfect recipe for burnout exists. Incorporating AI technology helps improve both work/life balance by eliminating stressors and relieves the administrative burden by creating a single version of the data upon which a claim is reviewed.
Innovative clinically assistive AI technologies deliver improved, consistent patient diagnosis and increased revenue on a per-patient basis. And while revenue is never the primary goal, it certainly helps mitigate the costs associated with implementing adjunctive technologies. To test this thesis, we sampled pilot patient cases to evaluate performance measures, patient treatment acceptance, and overall patient satisfaction. The case studies below are illustrative of the overall pilot group and indicate enhanced disease detection, patients’ understanding of their disease state, and trust in diagnosis.
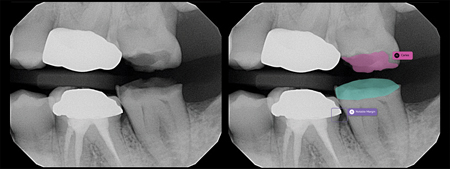
Case Study 1: Pull My Tooth
AI Persuaded the Patient to Save #36 and Address #35
This patient presented to the office in severe pain and just wanted “his tooth pulled.” The doctor was able to use Second Opinion, a real-time AI pathology detection aid, to help the patient see both the source of the pain (i.e. decay in proximity to the nerve on #36) and the fact that most of the structure of the tooth could be saved. The AI software also showed a very small cavity on #35-d that was not visible to the naked eye when performing the visual exam. The office was able to address both of these concerns on the same day, and to treat this patient’s pain without extraction. Two things occurred that would not have occurred without the assistance of AI. One, the patient was able to address the incipient decay on #35 with a less invasive, lower-cost treatment than would have been required to address decay that had progressed over the six months or more leading up to their next visit. Second, the patient made a healthier more conservative choice for treatment on #36. In essence, the objective ability to see the decay, versus merely trusting the dentist, allowed the patient to make a better decision by saving the tooth.
AI-INFLUENCED PRODUCTION IMPACT
36 Endo
36 Porcelain/Ceramic Crown
35 DO Resin
Comprehensive Exam
Fig. 1

Case Study #2 My “Free” Cleaning
An elderly patient presented to the office simply wanting her “free cleaning” and no other work. She was adamant about this. The office team again used Second Opinion to provide her with an AI-driven visual walkthrough of all conditions detected in her x-rays, including precise attachment loss measurements and localized annotations of impaction-influenced decay, an open margin on an existing restoration, as well as a missing crown. She proceeded to accept periodontal scaling and root planing (SRP) treatment and is scheduled to start treatment on #17, #27 and #37, as well as extract #18. This patient indicated that she had been told about the attachment loss on a prior visit but did not accept treatment because she was not certain that it was a valid concern. The colour-coded measurement annotations influenced her decision to accept treatment on this visit.
AI-INFLUENCED PRODUCTION IMPACT
SRP
27 Buildup
27 Porcelain/Ceramic Crown
37 Porcelain/Ceramic Crown
17 Porcelain/Ceramic Crown
18 Removal of Impacted Tooth
Fig. 2A
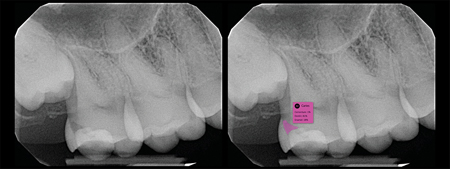
Fig. 2B
Fig. 2C
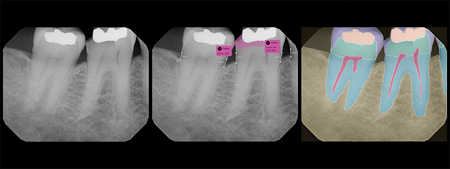
Case Study #3 Fix My Cracked Tooth
This patient presented to our office as an emergency patient with a broken #46. The office team utilized the AI software to show the patient that they had both a fractured #46 and mesial decay on previously filled #47. The patient clearly understood from the annotated images why something that did not yet hurt should be addressed. The office was able to address the patient’s chief concern on #46 as well as #47 on the same day, saving the patient both time and money in the future. The patient noted that she was impressed with the technology, adding that it helped her better understand her disease state.
AI-INFLUENCED PRODUCTION IMPACT
46 Indirect Pulp Cap
46 Buildup
46 Porcelain/Ceramic Crown
47 Buildup
47 Porcelain/Ceramic Crown
Fig. 3A

Fig. 3B
Comprehensive Exam
From a patient’s perspective, these annotated images clearly went a long way in terms of helping them see, understand, and take action to treat their respective disease states. With AI technology gaining in popularity, studies confirm that patients are now extremely receptive to the concept of AI-enabled assessments in dentistry. A recent L.E.K. Consulting study showed that 61% of all patients are very or extremely receptive to annotated x-rays and 59% are willing to switch providers in order to receive exam annotations and treatment supported by artificial intelligence. Similar findings were made in a patient trust and technology survey where 71% of the 600 U.S. dental patient respondents reported that they would be more likely to trust a diagnosis from a dentist who was using AI to assist in disease detection.9 The time to leverage this technology across the dental field has arrived.
Conclusion
Some dentists may have concerns about being replaced by robots, but we expect those fears to dissipate when the convenience and productivity of the AI assistant become well known. AI technologies do not provide care, and so AI will not replace dentists; it will assist them. In the next few years, we anticipate widespread adoption of dental AI; in fact, it will become an expected adjunct to the x-ray camera. We expect treatment costs to become less unpredictable and variable, and patients to feel increased confidence in the objectivity of their dentists.
Over the longer term, we hope to see increased use of population-wide “big data”, including dental data, to provide new insights into general health and its connections with dental health. When privacy concerns have been addressed, AI should go hand in hand with the digitization of health records to improve patient care both within and outside of the field of dentistry.
Oral Health welcomes this original article.
References
- Molteni R. (2021). The way we were (and how we got here): fifty years of technology changes in dental and maxillofacial radiology. Dento maxillo facial radiology, 50(1), 20200133. https://doi.org/10.1259/dmfr.20200133
- Inconsistency in Radiographic Dental Diagnostics & Treatment Planning. Dental AI Council. (2020, December). Retrieved September 21, 2022, from https://www.dentalaicouncil.org/research
- Carter, C., Sant, N., Annigeri, R., Puttashamachar, N., & Stanley, K. (2020). (rep.). Can a Computer Identify Carious Lesions in Dental X-Rays As Accurately As Humans? Pearl. Retrieved September 21, 2022, from https://pages.ada.org/can-a-computer-identify-carious-lesions-as-accurately-as-humans.
- Kaul, V., Enslin, S., & Gross, S. A. (2020). History of artificial intelligence in medicine. Gastrointestinal endoscopy, 92(4), 807–812. https://doi.org/10.1016/j.gie.2020.06.040
- Luchini, C., Pea, A. & Scarpa, A. (2022). Artificial intelligence in oncology: current applications and future perspectives. Br J Cancer 126, 4–9. https://doi.org/10.1038/s41416-021-01633-1
- Killock, D. (2020). AI outperforms radiologists in mammographic screening. Nat Rev Clin Oncol 17, 134. https://doi.org/10.1038/s41571-020-0329-7
- Ossowska, A., Kusiak, A., & S’ wietlik, D. (2022). Artificial Intelligence in Dentistry-Narrative Review. International journal of environmental research and public health, 19(6), 3449. https://doi.org/10.3390/ijerph19063449
- Ecenbarger, W. (2022, April 1). I Went to 50 Different Dentists and Almost All of Them Gave Me a Different Diagnosis. Reader’s Digest. Retrieved September 21, 2022, from https://www.rd.com/article/how-honest-are-dentists/.
- Pearl. (2022). (rep.). Dental Patient Trust & Technology Survey. Retrieved September 21, 2022, from https://www.hellopearl.com/guides/patient-trust?utm_campaign=Patient%20Trust%20%26%20Technology%20Survey&utm_medium=email&_hsmi=222290340&_hsenc=p2ANqtz–gbE5UvSw2XD1i8wlqncFxSS62_EAFTaKcnFrEtz0C5mDZ96ISP1xWmb8mG28qStrJRZhtcwundZ3Fo6Lqu3z3Z55_YQ&utm_content=222290340&utm_source=hs_email.
About the Authors
 Cindy Roark is the Senior Vice President and Chief Clinical Officer at Sage Dental Management and a member of the Harvard School of Dental Medicine Board of Fellows. Dr. Roark received a MS in Health Care Management degree from Harvard University and earned her dental degree Magna Cum Laude at the Henry M. Goldman School of Dental Medicine at Boston University.
Cindy Roark is the Senior Vice President and Chief Clinical Officer at Sage Dental Management and a member of the Harvard School of Dental Medicine Board of Fellows. Dr. Roark received a MS in Health Care Management degree from Harvard University and earned her dental degree Magna Cum Laude at the Henry M. Goldman School of Dental Medicine at Boston University.
 Kyle Stanley is chief clinical officer at Pearl, an AI company specializing in diagnostic and business analytics solutions for the dental industry. A graduate and former faculty member of USC’s Herman Ostrow School of Dentistry, Dr. Stanley’s research has been published in international dental journals. His private practice is in Beverly Hills, CA.
Kyle Stanley is chief clinical officer at Pearl, an AI company specializing in diagnostic and business analytics solutions for the dental industry. A graduate and former faculty member of USC’s Herman Ostrow School of Dentistry, Dr. Stanley’s research has been published in international dental journals. His private practice is in Beverly Hills, CA.