Many dental patients lead active lifestyles and their participation in athletic activities of all types continues to rise. The driving factor seems to be a societal focus on wellness, nutrition, and health. One study found considerable consistency across both sport and age levels when examining the relative importance of the different enjoyment factors related to sports participation. Factors that were interpreted as being intrinsic, or giving personal satisfaction to the sport activity (excitement of the sport, personal accomplishment, improving one’s skills, competing against others, and playing the sport itself), were consistently rated as being most important, whereas more extrinsic or outcome-related factors (pleasing others, winning rewards, winning the game), were consistently rated least important. The social aspects of “being on a team” and “being with friends” were deemed of intermediate importance.1
Participation in sports is not without inherent risk for injury, however, and includes trauma to the orofacial region. Proper sport-specific protective equipment can be helpful in preventing or decreasing the severity of dental and/or facial trauma. Studies on the use of athletic mouthguards to diminish or prevent dental injuries are voluminous, and the wear of such appliances is highly recommended, even when not mandatory, for those active in sport.2-14 Some sports may pose a higher risk of trauma. Fos, Pinkham and Ranalli formulated a sports classification matrix characterized by two dimensions: (1) the velocity and (2) the intensity of the sport.15 Based on the matrix parameters, the degree of risk can be assessed and estimated relative to the intensity and velocity levels of the sport. (Box 1).
Box 1

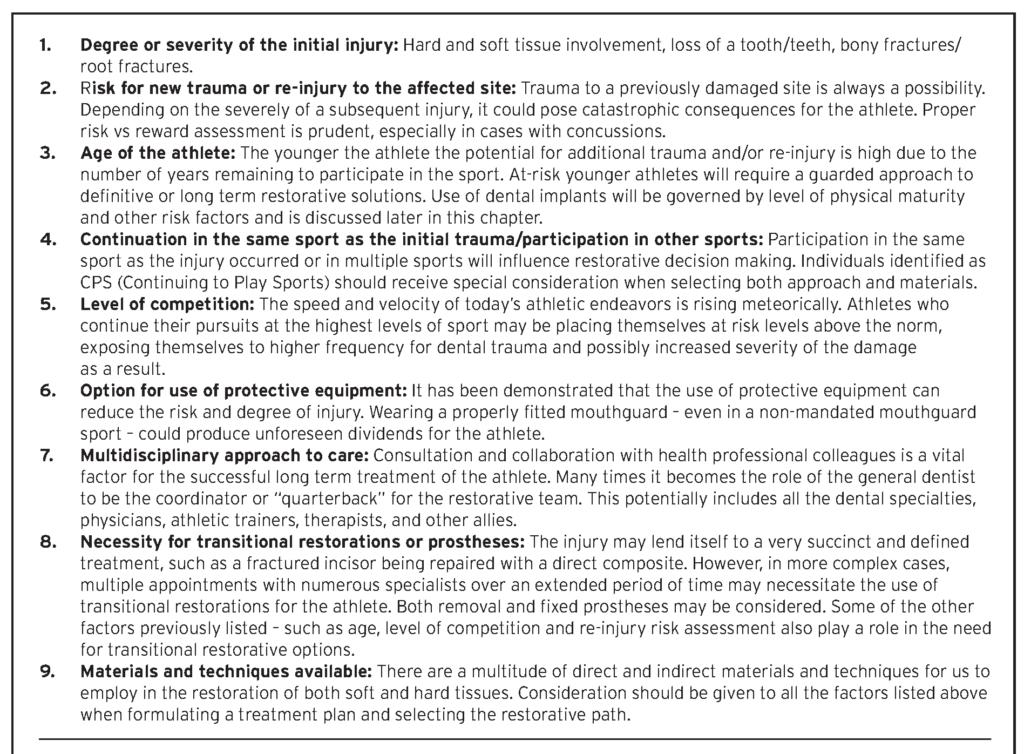
In the event of a sports-related dental injury, risk variables are considered, and a treatment plan is formulated. The use of a decision-tree model is helpful in determining a practical and logical course of action. This provides a systematic approach for evaluation and treatment for the dentist, the athlete, and their families, delineating a restorative path based on science and a best-outcomes scenario.16 (Box 2).
Box 2
Once post-trauma stabilization is achieved, and risk assessment completed, the next step is to develop a restorative treatment plan. The course of treatment may be classified as:
- Simple – completed in one or two appointments
- Complex – requiring multiple appointments over a period of time
- Multidisciplinary – utilizing the expertise of specialist colleagues to complete the restoration
Advances in dental materials offer multiple restorative options. Ceramics, resins, and dental implants may all play a role in the decision-making process. Collaborating with dental specialists, as well as other healthcare providers (athletic trainers, physicians, and physical therapists), in both the planning and treatment phases, paves a path to success. Any treatment plan should be formulated using the latest scientific data and sound clinical judgement, as applied to the specific presenting circumstances.
A conservative approach should be considered in formulating the treatment plan when the athlete will continue to play sports (CPS), particularly at a high level. Consequently, some approaches which may not be appropriate for the mainstream patient population can be considered. Contemporary dental materials and techniques, such as direct composite resins and adhesive bonding, are ideal for restoring many sports-related injuries. Composite resins are key because they are additive; they restore only what is missing or damaged. They are also readily available, repairable, and are the least costly of all tooth colored restorative materials.
CASE REPORT:
A 31-year-old male athlete fractured his maxillary right central incisor (#11) while playing in an adult hockey league. The fractured tooth fragment was not found, necessitating a restorative procedure. The fracture was diagnosed as an Ellis Class III (no pulpal exposure). During the patient examination, variously angled digital periapical radiographs assessed for root fracture. The patient reported minor sensitivity to temperatures (2 on a scale of 10), and the tooth displayed no mobility but was slightly responsive to percussion. The injury was classified as a concussive luxation. Treatment options discussed with the patient included: (1) full and partial coverage with an indirect approach, (2) direct restorative materials, and (3) application of a trauma splint. The patient decided on a composite resin for reasons of tooth structure conservation and cost-effectiveness. He declined a post-operative trauma splint. (Figs. 1 & 2)
Fig. 1

Fig. 2

Composite resins can restore teeth to replace lost tooth structures in a variety of ways. Contemporary direct resins offer the practitioner a multitude of options in recreating nature: (1) single shade (monochromatic), (2) two layers with a body/dentin and enamel (gradient) or (3) multiple layers (stratified) which can incorporate special effects (halo, mamelon definition, translucency, maverick lines, flecks or fluorosis). Melding the material and the technique allows dentists to replicate natural structures.
A local anesthetic (1.8cc 2% mepivacaine hydrochloride with levonordefrin 1:20,000) was administered using labial infiltration. A two-tier bevel technique prepared for the Class IV composite. The primary 2 mm bevel at a 300 angle both labially and lingually was prepared with a 100u diamond. This significant “heavy” bevel allowed the dentin replacement portion of the resin to have adequate bulk and to overlap the Class IV fracture, thus blocking light transmission which could otherwise reveal a visible line in the final restoration. Use of the newly developed, single shade composite OMNICHROMA (Tokuyama Dental, Encinitas CA) facilitates shade matching as it is the restorative material itself which adapts to the surrounding coloration of the natural dentition. For Class IVs, the OMNICHROMA Blocker prevents dark tooth coloration or lingual show through.
The second “feather” 2 mm bevel was placed at a shallow angle in an irregular pattern prepared with a 60u diamond (Premier Dental, Plymouth Meeting PA). Human eyes tend to notice straight lines; the irregular pattern allows for light reflection and refraction to be scattered, creating an indiscernible margin once the enamel layer is placed and finished. (Fig. 3)
Fig. 3

Isolation of the preparation was achieved with a specialized clear matrix, Margin Perfect Matrix Ultra (Margin Perfect Matrix, www.marginperfectmatrix.com), and secured into place with Heliobond, an unfilled light cured resin (Ivoclar/Vivadent, Schaan, Liechtenstein). This created a sealed system to place the composite, an anatomically favorable shape, and an emergence angle for the restoration. A total-etch technique on both enamel and dentin was followed by a universal bonding agent, applied according to the manufacturer’s instructions. An initial light-blocking dentin replacement layer of composite was placed and shaped to replace the missing dentin portions of the tooth. Care was taken to wrap this layer over the incisal edge both facially and lingually and to carry it just beyond the initial “heavy” bevel margins. After shaping with composite hand instruments and brushes, the dentin-replacement layer was polymerized from both the labial and lingual for 20 seconds using an LED light source.
Subsequently, the second or enamel-replacement layer was added and shaped to extend the material slightly beyond the “feather” bevel, over-building the restoration by 10% to allow for finishing, and then cured for an additional 20 seconds. The matrix was removed from the tooth. Post-cure shaping and texturing were achieved with various 12-fluted, spiral-bladed carbide burs (Brasseler USA, Savannah GA). Final polish of the Class IV composite was completed with Astropol abrasive cups and points (Ivoclar/Vivadent). (Fig. 4).
Fig. 4

Fig. 5

CONCLUSION:
Preventive measures, such as protective equipment and custom-fitted mouthguards, can be implemented to decrease the potential risk or severity of sports-related dental trauma. However, damage and injury to the oral cavity during participation in sports, especially the anterior dentition, is a reality. In situations such as the above, where the fractured tooth fragment is not reclaimed, the dentist is challenged to rebuild lost dental structures with artificial materials. Composite resins offer the dentist the best overall solution to this esthetic and functional dilemma. Modern composite resins and adhesives offer unlimited options for additive solutions to dental trauma cases involving one or more fractured teeth. Although the severity of the fracture plays a key role in the decision-making process of selecting a restorative modality, direct resins are eminently suitable as transitional or permanent solutions after athletic traumas at all ages.
Oral Health welcomes this original article.
References
- Wankel LM, Kreisel PS. Factors underlying enjoyment of youth sports: Sport and age group comparisons. Jour Sport and Exercise Psych 1985;7(1):51-64.
- Heintz WD. Mouth protectors: a progress report. Bureau of Dental Health Education. J Am Dent Assoc. 1986;77:632-636.
- Luyk NH, Larsen PE. The diagnosis and treatment of the dislocated mandible. Am J Emerg Med. 1989;7:329-335.
- Kvittem B, Hardie N, Roettger M et al. Incidence of orofacial injuries in high school sports. J Public Health Dent 58(4):288-93, 1998.
- Woodmansey KF. Athletic mouth guards prevent orofacial injuries: a review. Gen Dent. 1999;47:64-69.
- Labella CR, Smith BW, Sigurdsson A. Effect of mouth guards on dental injuries and concussions in college basketball. Med Sci Sports Exerc. 2002;34:41-44.
- Labella CR, Smith BW, Sigurdsson A. Effect of mouth guards on dental injuries and concussions in college basketball. Med Sci Sports Exerc. 2002;34:41-44.
- Muhtarogullari M, Demiralp B, Ertan A. Non-surgical treatment of sports-related temporomandibular joint disorders in basketball players. Dent Traumatol. 2004;20:338-343.
- ADA Council on Access, Prevention and Interprofessional Relations; ADA Council on Scientific Affairs. Using mouth guards to reduce the incidence and severity of sports-related oral injuries. JADA. 2006;137:1712-1720.
- Cohenca N, Roges RA, Roges R. The incidence and severity of dental trauma in intercollegiate athletes.J Am Dent Assoc. 2007;138:1121-1126.
- Knapik JJ, Marshall SW, Lee RB, et al. Mouthguards in sport activities: history, physical properties and injury prevention effectiveness. Sports Med. 2007;37:117-144.
- Emerich K, Kaczmarek J. First aid for dental trauma caused by sporting activities. Sports Med. 2010;40:361-366.
- Tiryaki M, Saygi G, Yildiz S et al. Prevalence of dental injuries and awareness regarding mouthguards among basketball players and coaches. J Sports Med Phys Fitness. 2017 Nov;57(11):1541-1547.
- Fernandes LM, Neto JCL, Lima TFR et al. The use of mouthguards and prevalence of dento-alveolar trauma among athletes: A systematic review and meta-analysis. Dent Traumatol. 2019 Feb;35(1):54-72.
- Fos PJ, Pinkham JR, Ranalli, DN: Prediction of sports-related dental traumatic injuries. Dental Clinics of North America 44(1): 19-33, January, 2000.
- Lambert DL, McNew D, Shaker Z. (2018). ‘Restorative considerations after athletic dental trauma’ in Roettger, M. (ed) Modern Sports Dentistry. Springer International, pp. 93-110.
About the Author
 Douglas L. Lambert graduated from the University of Minnesota Carlson School of Management and the University of Minnesota School of Dentistry. He is a Fellow in the American College of Dentists, International College of Dentists, Pierre Fauchard Academy, Academy for Sports Dentistry, American Society for Dental Aesthetics, and a Diplomat of the American Board of Aesthetic Dentistry. He serves as an independent researcher for many dental manufacturers, and as the team dentist for the Minnesota Lynx of the WNBA. Dr. Lambert’s practice in Edina, Minnesota emphasizes cosmetic, comprehensive, and sports dentistry.
Douglas L. Lambert graduated from the University of Minnesota Carlson School of Management and the University of Minnesota School of Dentistry. He is a Fellow in the American College of Dentists, International College of Dentists, Pierre Fauchard Academy, Academy for Sports Dentistry, American Society for Dental Aesthetics, and a Diplomat of the American Board of Aesthetic Dentistry. He serves as an independent researcher for many dental manufacturers, and as the team dentist for the Minnesota Lynx of the WNBA. Dr. Lambert’s practice in Edina, Minnesota emphasizes cosmetic, comprehensive, and sports dentistry.
To see more articles from the July/August 2020 issue, please click here!












