The challenge currently facing reconstructive dentistry is how to obtain excellent esthetic results while preserving the biological structures involved as much as possible. Today, the clinician and the technician have materials and procedures at their disposal which make it possible to recreate esthetics and function in a simpler and more predictable way.1,2,3
One of the main clinical complications in fixed prosthodontics around natural teeth is the unsatisfactory esthetic result due to the apical migration of the gingival margin.4,5 With the BOPT (Biologically Oriented Preparation Technique) concept, the clinician and the laboratory technician can interact with the surrounding tissues modifying their shape and scalloped architecture regardless of any preexisting dental or gingival limitation.23
We know that apical migration of the gingiva is related to different factors:
- Inadequate quality and quantity of keratinized gingiva (thin biotypes are more likely to have recessions)
- Reaction to a trauma during prosthetic work (preparation, gingival retraction). Chronic inflammation due to prosthetic errors (open margins, violation of the biological width, horizontal overcontour)
- Poor oral hygiene and tooth brush trauma
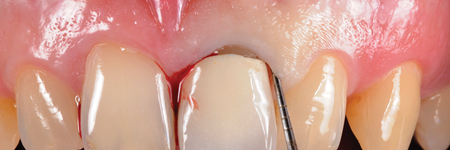
With the BOPT concept, it is possible to transfer the emergent anatomy to the prosthetic crown. This allows a free interaction with the gingiva that will adapt, shape and settle around new forms and profiles. The crown’s contours obtained with the BOPT technique may appear excessively pronounced, based on the traditional definition of “overcontour”.6 Clinically there is no overcontour, but a “different new contour” and new PCEJ (prosthetic cementoenamel junction)( Fig. 1).
Fig. 1A

Fig. 1B

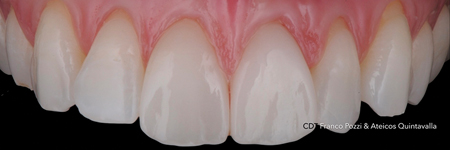
Fig. 1C

Fig. 1D

Among factors related to BOPT concept, one is particularly relevant: the preparation technique and the corresponding geometry of the finish line.
Traditionally, there are two types of dental preparations7:
1. Preparations with finishing lines (also called horizontal)
shoulder
shoulder with bevel
inclined shoulder (50 degrees and 135 degrees)
Chamfer
Chamfer with bevel
2. Preparations without finishing lines (also called vertical), described as feather edge
Horizontal preparations are preferred when the clinical and anatomical crown coincide and there is good periodontal health. Prosthetic margins are located near the cementoenamel junction (CEJ). Preparations without finish lines are more conservative and are used when the clinical crown does not coincide with the anatomic crown because of the loss of support due to periodontal disease.8,9
Although a feather-edge preparation is commonly indicated for use in periodontally involved teeth as abutments for fixed prostheses, this approach may also represent a less invasive alternative to a horizontal margin in various other clinical conditions.
This includes replacement of old crowns (Fig. 2) that have:
- inadequate quality and quantity of keratinized gingiva
- violation of the biological width
- gingival colour changes
- altered gingival architecture
Fig. 2A

Fig. 2B
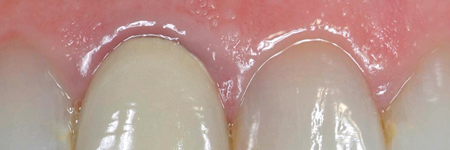
Fig. 2C

And also in conditions such as endodontically treated teeth or vital teeth in young individuals which require a modification in color or shape or are compromised by erosive-abrasive pathologies.10
Figure 3 illustrates the BOPT with NO-Prep veneers.
Fig. 3A

Fig. 3B
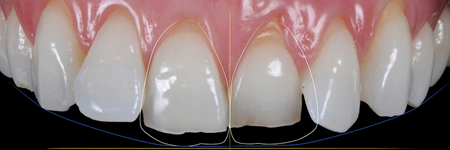
Fig. 3C
The main clinical difference between horizontal and vertical preparations is that in the first ones the margin is positioned by the dentist and leaves a well-defined line on the tooth, which is then replicated in the impression and the working model. For vertical preparations, the margin is positioned by the laboratory technician based on the gingival tissue information.
BOPT—The Restorative Procedure
Before starting the procedure, an accurate intrasulcular mapping is made with a periodontal probe in order to assess the level of the epithelial attachment (Fig. 4).
Fig. 4A

Fig. 4B

Fig. 4C
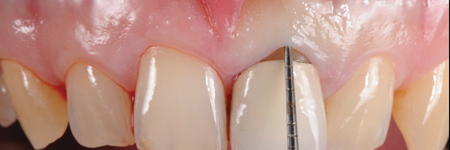
Fig. 4D
Feather-edge tooth preparation is performed with a flame bur separating the interproximal contact points and following the gingival contour in order to erase the natural tooth undercuts and to enable an adequate fit of the restorations (Fig. 5).
A minimum space of 0.3 mm at the margin, 0.5 mm along the axial walls, and 1 to 1.5 mm on the occlusal surface to ensure sufficient resistance of the restoration, is provided at the completion of tooth reduction. The final form of the preparation is slightly conical (2 to 6 degrees) making possible a complete 360-degree view of the cervical perimeter of the natural abutment (Fig. 5D).
Fig. 5A

Fig. 5B

Fig. 5C

Fig. 5D

The bur interacts at the same time with the sulcular internal wall and with the epithelial component of the gingival attachment (gingitage technique). In this way, the existing CEJ or existing horizontal finishing line is erased. This will allow for the creation of a finish area within which the crown margin can be moved coronally or apically.
Temporary crown relining is key to understanding how to create a new CEJ. The new temporary crown margin with a new shape and form, is positioned in the sulcus, no deeper than 0.5 to 1 mm, fully respecting the biologic width (controlled invasion of the gingival sulcus) (Fig. 6).
Fig. 6A

Fig. 6B

Gingitage preparation, together with the reduction of the tooth, will create a space that will be filled by a clot from intrasulcular bleeding. The intrasulcular portion of the temporary crown’s margin will support the gingival margin circumferentially, allowing the clot stabilization into a fully structured gingival tissue (clot preservation). The healing process will determine the reattachment and thickening of the gingival tissue, which will mold and adapt to the new emergence profile (Fig. 7).
Fig. 7A

Fig. 7B

Fig. 7C

After a minimum of four weeks, the gingival tissue will be stabilized and it will be possible to take the impression to finalize the restoration.
Cementation of the definitive crown is done utilizing rubber-dam when the finish line is located juxtagingivally. In this case a conventional adhesive procedure including etching, priming, and bonding of the tooth surface is performed and a light-cured resin cement is used. When the margin is placed inside the intrasulcular compartment, alternative systems to isolate the environment from moisture (such as retractors for the lips, cotton rolls, or retraction cords to control the sulcular fluid) are used (Fig. 8).
Fig. 8A

environment from moisture (such as retractors for the lips, cotton rolls, or retraction cords to control the sulcular fluid) are used.
Fig. 8B

If coronal or apical migration of soft tissue, according to the esthetic expectations is needed, we can modify both the temporary crown and final crown margin, creating a new prosthetic CEJ, more coronally or more apically. In few weeks, the gingival margin will adapt to the new emergence profile (Fig. 9).
Fig. 9A

Fig. 9B

BOPT—The Laboratory Procedure
The development of the impression will allow the technician to identify the finishing area on the working model. A red mark is traced with a 0.5 mm pencil over the gingival contour projecting it on the abutment’s wall (red line) (Fig. 10).
Fig. 10A

Fig. 10B

When the apical part of the model is exposed, it will be marked with a blue line. The area between the two lines, the red and the blue ones, is called the “finishing area” and within this area we create the final crown margin (Fig. 11).
Fig. 11

In the BOPT technique, the finishing line is the prosthetic crown’s margin itself. This margin can be shortened or extended both in the temporary or final restoration at different intrasulcular levels, without harming the quality of fit. Positioning the crown margin more apically or coronally will depend on the depth of the sulcus and on the esthetic needs, but the crown margin will never invade the epithelial attachment. This is the adaptation forms and profiles concept (Fig. 12).
Fig. 12

With the feather edge preparation, a crown margin can be shortened or extended at different intrasulcular levels without harming the quality of fit
a. natural tooth
b. chamfer preparation
c. feather edge preparation
d. coronal crown margin
e. apical crown margin
As an alternative to what other authors have proposed for restorations with feather edge preparations11,12 the BOPT technique introduces a new concept based on an observation that it is the gingival profile that adapts itself in a symmetrical way to the coronal emergence profile (Fig. 13) and not the reverse (adaptation forms and profiles concept)13,14 (Fig. 14).
Fig. 13

Fig. 14A

Fig. 14B
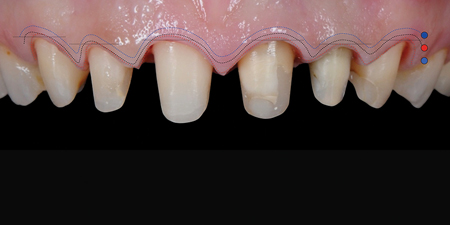
Fig. 14C
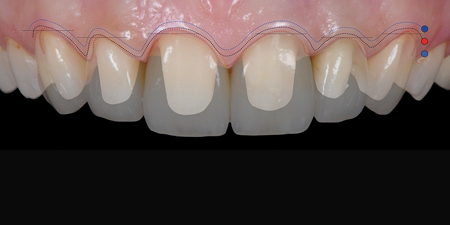
Fig. 14D

BOPT
Clinical advantages:
- Erasure of anatomical cementoenamel junction (CEJ) in unprepared teeth and deletion of the previously existing finish lines in already prepared teeth to create a finishing area.
- The possibility to position the final finishing line at different levels, within the finishing area, either more coronally or more apically, with a controlled invasion of sulcus, without affecting the quality of marginal adaptation of the restoration.
- The possibility to modulate the crown emergence profiles to create the ideal esthetic gingival architecture (adaptive forms and profiles). In this way, a new prosthetic cementoenamel junction (PCEJ) will be created.15,16
- Preservation of dental structure.
- Easy and fast to execute.
- Ease in relining and finishing temporary crowns.
- Ease in impression taking.
Biological advantages:
- Increase in gingival thickness.
- Increased stability of the gingival margin over time.
- Possibility to place the gingival margin at different levels by remodeling the emergence profiles.
Clinical and Biological Considerations
The literature contains ample criticism of the feather-edge margin, mainly because of the presence of overcontour and the consequent fragility of the crown, determined by the limited thickness of the restoration in the cervical area.17 It should be emphasized that in daily dental practice, however, these problems have no real clinical significance and do not seem to constitute a concrete risk factor either for the periodontal health or for the strength of the restoration, provided that the correct clinical and technical requisites are observed. Tissue response is seen to be optimal over time, with stability of gingival position and absolutely no signs of inflammation. This can be explained by the anatomical condition which is obtained through this approach, consisting of creating an artificial CEJ similar to the cementoenamel junction found in nature.18,19 The margin of the restoration creates an overcontour, exactly as it happens in the natural CEJ, where a change in the inclination of the profile between the root and the crown is always present. This slight marginal convexity provides support for the periodontal tissue, ensuring excellent stability of the gingival contour. The prosthesis margin remains located in the superficial portion of the intrasulcular compartment without damaging the periodontal attachment.20 Moreover, a vertical margin is compatible with a high level of precision,21 which also has an impact on the health of the marginal tissue, and facilitates a lower incidence of decay infiltration.
The strength of the final restoration (whether lithium disilicate, Zirconia or PFM) is guaranteed both by an adequate occlusal thickness and by a reinforcement of the marginal area by means of a slight enlargement of the emergence profile through a thin increment of ceramic, zirconia or metal (for PFM). This moderate increase of the marginal thickness creates a cervical collar which reinforces the restoration.22
Conclusion
With the BOPT technique, the clinician and the laboratory technician can interact with the surrounding tissues with ease and predictability. Clinical results are obtained through the restoration itself, both provisional and final (margin position, emergence profile, tooth form). This prosthetic approach, using a flapless feather edge preparation, if compared to other preparation techniques (chamfer, shoulder, etc), is simpler and faster.
We can achieve high quality clinical and esthetic results in terms of soft tissue stability at the prosthetic/tissue interface with a minimally invasive approach, preserving as much as possible the biological structures involved in the treatment.
Oral Health welcomes this original article.
References
- Edelhoff D, Brix O. All-ceramic restorations in different indications: a case series. J Am Dent Assoc 2011; 142(suppl 2):14S-9S.
- Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for posterior teeth. Int J Periodontics Restorative Dent 2002;22:241-249
- Valenti M, Valenti A. Retrospective survival analysis of 261 lithium disilicate crowns in a private general practice. Quintessence Int 2009;40: 573-579.
- Behr M, Hansmann M, Rosentritt M, Handel G. Marginal adaptation of three self-adhesive resin cements vs. a well-tried adhesive luting agent. Clin Oral Investig 2009;13:459-464.
- Beuer F, Aggstaller H, Edelhoff D, Gernet W. Effect of preparation design on the fracture resistance of zirconia crown copings. Dent Mater J 2008;27:362-367.
- Sorensen JA. Standardized method for determination of crown fidelity. J Prosthet Dent 1990;64:18–24
- Pardo GL.A full cast restoration design offering superior marginal characteristics J.Prosthet Dent1982;48:539– 543.
- Amsterdam M, Abrams L. Periodontal prosthesis. In Cohen (eds). Periodontal therapy, ed 4. St.Louis: CV Mosby Co, 1968.
- Di Febo G. Freni Sterrantino S. Treatment of a case of advanced periodontitis: Clinical procedures utilizing the ‘combined preparation technique’ Int J of Perio Rest Dent 1985;5:52–62.
- Schmitt J, Wichmann M, Holst S, Reich S. Restoring severely compromised anterior teeth with zirconia crowns and feather-edged margin preparations: a 3-year follow-up of a prospective clinical trial. Int J Prosthodont 2010;23:107-109.
- Abrams L. Graduate periodontal and prosthetic lectures. Boston University 1971. Boston: Boston University Press, 1971.
- Kay HB. Criteria for restorative contours in the altered periodontal environment. Int J Periodont Rest Dent 1985;5:42–63.
- Loi I. Protesi su denti naturali nei settori di rilevanza estetica con tecnica BOPT: Case series report. Dental Cadmos 2008;76:51–59.
- Loi I, Galli F., Scutellà F. Di Felice A. Il contorno coronale protesico con tecnica di preparazione BOPT (Biologically Oriented Preparation Technique) :considerazioni tecniche. Quintessenza Internazionale 2009;25:4–19.
- Abrams L. Graduate periodontal and prosthetic lectures. Boston University 1971. Boston: Boston University Press, 1971.
- Kay HB. Criteria for restora- tive contours in the altered periodontal environment. Int J Periodont Rest Dent 1985;5:42–63.
- Proos KA, Swain MV, Ironside J, Steven GP.Influence of margin design and taper abutment angle on a restored crown of a first premolar using finite element analysis. Int J Prosthodont 2003;16:442-449.
- Loi I, Galli F, Scutellà F, Di Felice A. Il contorno coronale protesico con tecnica di preparazione BOPT (Biologically Oriented Preparation Technique): considerazioni tecniche.
- Pardo GI. A full cast restoration design offering superior marginal characteristics. J Prosthet Dent 1982;38: 539-543.
- Gargiulo AW, Wentz FM, Orban BJ. Dimensions and relations of the dentogingival junction in humans. J Periodontal 1961;32:261-267.
- Çömlekog ˘lu ME, Dündar M, Gokce B, Özcan M, Güngör MA, Artunç C. Influence of cervical finish line type on marginal adaptation of zirconia ceramic crowns. Oper Dent 2009;34:586-592.
- Cortellini D, Parvizi A. Rehabilitation of severely eroded dentition utilizing all-ceramic restorations. Pract Proced Aesthet Dent 2003;15: 275-282.
- Biologically oriented preparation technique (BOPT): a new approach for prosthetic restoration of periodontically healthy teeth Ignazio Loi, MD, DDS Private Practice, Cagliari, Italy Antonello Di Felice, CDT Private Practice, Rome, Italy The European Journal of Esthetic Dentistry, Volume 8, number 1, spring 2013.
About the Author
 Stefano Conti received his DDS degree at the University of Medicine and Surgery, School of Dentistry, in Parma, Italy in 1989. He is a lecturer at the Masters Program of Implantology and the Masters Program of Facial Esthetics at the University of Parma, School of Dentistry. He works in private practice in Parma, Italy and Kiev, Ukraine, where he has restricted his clinical work to Implant Surgery and Esthetics around natural teeth and Implants.
Stefano Conti received his DDS degree at the University of Medicine and Surgery, School of Dentistry, in Parma, Italy in 1989. He is a lecturer at the Masters Program of Implantology and the Masters Program of Facial Esthetics at the University of Parma, School of Dentistry. He works in private practice in Parma, Italy and Kiev, Ukraine, where he has restricted his clinical work to Implant Surgery and Esthetics around natural teeth and Implants.
Follow the Oral Health Group on Facebook, Instagram, Twitter and LinkedIn for the latest updates on news, clinical articles, practice management and more!












