
Abstract
Endodontic surgical treatment of a root end pathology can be very successful when properly diagnosed. PRF, a type of blood derived concentrate, has shown promising results to improve healing of the surgical site as well as improve patient post operative pain and quality of life. The present article describes in detail the clinical application of PRF combined with mineralized/demineralized freeze-dried bone (M/DNFDB), and PRF membrane in the management of periapical lesions. The purpose of this case report is to encourage clinicians by adding to the existing literature about the combined use of PRF, graft material, and PRF barrier membrane in the treatment of periapical lesions. A review of literature reveals that there is little documentation of case reports using a combination of PRF, M/DMFDB, and PRF membrane in the management of periapical lesions.
Platelet-Rich Plasma (PRP) has been used in different facets of medicine since the 1970s when it was first described by hematologists.1 More recently, Platelet-Rich Fibrin (PRF) is shown to have more benefit than PRP in all aspects of wound healing, specifically, and soft/hard tissue regeneration.2
Currently, there is significant evidence that shows the benefits of PRF. Some benefits include the following: increased angiogenesis,3 anti-inflammatory properties,4 decreased pain,5 antimicrobial effects,6 decreased swelling post operatively.7 This article presents a case where, in addition to sound clinical techniques, PRF is used to improve healing.
The current article presents a case where a non-healing apical lesion is treated surgically. The provider uses a combination of PRF, M/DMFDB, and a PRF membrane to promote improved hard and soft tissue healing with a goal to preserve buccal maxillary bone thickness. 12-month recall and CBCT imaging show complete healing of the surgical site.
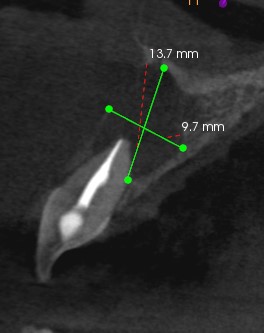
A 17-year old male with no significant medical history presented to the authors private practice for evaluation and treatment of #8. Clinical and radiographic examination completed as well as all the customary release forms and paperwork. (Figs. #1 & #2) Clinical examination showed probing depths and mobility were within normal limits and no evidence of sinus tract. Radiographic examination shows existing dental treatment on tooth #8 including root canal therapy and lingual composite filling. (Fig. #1) Extensive bone loss is apparent around the apex of #8. CBCT revealed an absence of the buccal plate with a thin palatal plate. (Fig. #2) Tooth #8 is symptomatic to palpation.
Fig. 1

Fig. 2
Teeth #8 had a diagnosis of previously treated, symptomatic apical periodontitis with a good prognosis. The following treatment was recommended to the patient: #8 apicoectomy with autologous PRF and bone graft.
The following steps were used to complete the treatment
- Local anesthesia: Buccal and palatal infiltration of the following, Lidocaine with 1:100K epinephrine and 1:50K epinephrine.
- PRF: Blood is drawn from the patients right arm, antecubital fossa region, with a 21G x ¾ butterfly-type needle (Vacuette).12 (Fig. #3) One green and one red test tube (A-prf.com, France) were then spun in a centrifuge (DUO Quattro) for 14 minutes.
- PRF material is then prepared into a thin clot and two membranes. The liquid from the green tube was mixed with M/DFDB (maxxeus.com). (Fig. #4)
- Prepare a full mucogingival flap, locate the lesion, develop a suitable crypt, and root-end resection with a surgical handpiece and 556 bur. Curettage of the entire lesion (Fig. #5) and application of ferric sulfate 20% to aid in hemostasis. Root end preparation with UltraSonic tip (Kerr USA). Retrofill placed with bioceramic material (Edge Endo, USA). Placement of: PRF plug against the palatal plate of the crypt, (Fig. #6) PRF sticky bone into the crypt, (Fig. #7) and 2 PRF membranes. (Fig. #8) Suture using monoglyc 4-0 (A-prf.com, France).9
Fig. 3

Fig. 4

Fig. 5

Fig. 6

Fig. 7

Fig. 8

Post operative care includes the following: a 2-week postoperative visit to observe healing as well as a 1-year visit. Accelerated soft tissue healing was observed at the time of the 2-week visit. Additionally, the patient reported minimal pain or swelling a few days after the surgery was completed. At the 1-year recall appointment, the surgical site is evaluated radiographically both 2D (Fig. #9) and 3D. (Fig. #10) Adequate healing occurred post operatively, evidenced by these two images.
Fig. 9

Fig. 10

Discussion
With proper diagnosis and use of diagnostic imaging, apical microsurgery can be a very successful treatment option.10 When infections persist after non-surgical options have been exhausted, a surgical approach can be used to achieve the desired result. However, in some cases, an apicoectomy is performed knowing that the tooth will eventually be replaced with a dental implant in the future. In a case such as this, the quality of bone is most important. The quality of bone can include density and thickness. If an improvement in thickness is the desired result, an overfill of graph material in a convex fashion can be used. The current article tries to show steps that will promote good bone healing and maintain or even improve bone thickness.
Platelet rich fibrin (PRF) material is used in this case presentation because of the overwhelming evidence in the literature surrounding the use of this material. Almost 25 years have passed since PRF was first introduced into medicine and then dentistry. Since then, a few modifications have been made to collect methods. Heparin is no longer used in test tubes and the centrifuge protocol has been changed to a “low-speed centrifuge concept”. These factors and others, including the presence of leukocytes, have had a significant improvement in healing quality.10
Despite this evidence, PRF appears to be infrequently used in endodontic offices in the United States. In the author’s opinion, this may be due to several factors including unfamiliarity with the benefits of PRF and difficulties in drawing patient blood. However, further studies should be conducted to identify the frequency of use of PRF in an endodontic office.
The present article looks to elucidate the option of grafting a periapical surgery site and the type of graft materials to consider using. In an article by T. J. Lui et al, a meta-analysis was performed on different regenerative techniques and materials used to improve outcomes of endodontics surgery. This study shows that generally, the use of regenerative techniques significantly improved the outcome of endodontic surgery when compared to using no regenerative techniques at all. It also showed that the application of collagen membranes or autologous platelet concentrates, of which PRF is one, alone was associated with a trend for better outcomes. Furthermore, the same study showed that the combined use of collagen membranes and bovine-derived hydroxyapatite significantly improved the outcome.11 It is therefore reasonable to conclude that graft material which includes bone, PRF, and PRF membrane would promote significantly better healing, than using no regenerative material at all. More studies implementing PRF during apicoectomy procedures would be required to prove this hypothesis.
Oral Health welcomes this original article.
References
- Alves R, Grimalt R. A review of Platelet-rich Plasma: HIstory, Biology, Mechanism of Action, and Classification. Skin Appendage Disord 2018; 4:18-24.
- Ling H, Ye L, Xiulian H, Yu Z, Hui W. A comparative study of platelet rich fibrin (PRF) and platelet-rich plasma (PRP) on the effect of proliferation and differentiation of rat osteoblasts in vitro. OS,OM,OP,OR&E. 2009;11:707-713.
- Herrera-Vizcaino C, Choukroun J, Ghanaati S. Platelet-rich secretome induces three dimensional angiogenic activation in vitro. Eur Cell Mater. 2019;4:250-264.
- Nasirzade J, Gruber R. Platelet-Rich Fibrin Elicits an Anti-inflammatory Response in Macrophages.J Periodontal. 2019;2:244-252.
- Lektemur Alpn A et al. PRF improves wound healing and postoperative discomfort after harvesting subepithelial connective tissue graft from palate: a randomized controlled trial. Clin Oral Investig. 2019;5.
- Ko YP. Fibrinogen is at the interface of the host and Defense and Pathogen Virulence in Staphylococcus Aureus infection. Sem Thromb Hemost.. 2016;10:408-421.
- Massimo Del F, Valentina C, Alessandra L, Silvio T. Effect of Platelet Concentrate on Quality of Life after Periradicular Surgery: A randomized Clinical Study. JOE 2012:4;733-739.
- Apicoectomy #8 with PRF; Reno, NV: Tim Adams; 2022 Jan 29. Video:7:09. Available from: https://youtu.be/cy1lPRH1XuU
- Rubinstein R, Kim S. Long-Term follow up of cases considered healed one year after apical microsurgery. JOE 2002;5:378-383.
- Choukroun J, Miron R. Platelet Rich Fibrin in regenerative dentistry. Wiley Blackwell, 2017.
- T. J. Liu, J. N. Zhou, L. H. Guo. Impact of different regenerative techniques and materials on the healing outcome of endodontic surgery: a systematic review and meta-analysis. Int. Endo Jour 2021; April: 536-555.
- Venipuncture in an Endodontic office, PRF, IV Sedation; Reno, NV: Tim Adams; 2022 Jan 29. Video:8:26. Available from: https://youtu.be/yqtNpLhD0h8
About the Author

Tim Adams maintains a private practice in Reno, NV. He attended Brigham Young University, where he earned his Bachelor of Science in physics with a minor in French. After obtaining his dental degree from Temple Dental School in Philadelphia, he was commissioned into the US Army. Eventually, he received orders to deploy to Balad, Iraq for six months. After his military service, he was accepted into the endodontic residency program at Lutheran Medical Center in Brooklyn, NY. He received his certificate of Endodontics in 2013. Then achieved Diplomate Status in 2015. Dr. Adams is certified in IV conscious sedation.










