keywords:
Dens invaginatus, endodontic treatment, pulp diagnosis, cone-beam computed tomography.
Abstract
Dens invaginatus (DI) is a dental anomaly resulting from an infolding of the enamel organ into the dental papilla during tooth development. This article elucidates how non-surgical endodontic treatment of a rare and complex Type III DI and conservative treatment of the immature maxillary central incisor allowed for complete rhizogenesis to occur. Proper clinical and imaging examinations were paramount to obtain a definitive diagnosis and accurate treatment plan for successful treatment of this case.
INTRODUCTION
Dens invaginatus (DI) is a dental anomaly resulting from an infolding of the enamel organ into the dental papilla during tooth development.1 Oehlers2 proposed the most commonly used classification system of DI in 1957 whereby the invaginations were grouped into three distinct categories according to the depth of the invagination into the root. Type I – the invagination is minimal and enamel-lined, and confined within the crown of the tooth and does not extend beyond the cementoenamel junction; Type II – the invagination is enamel-lined and extends into the pulp chamber, however it remains within the root canal and no communication with the periodontal ligament exists; Type III – the invagination extends through the root and communicates laterally or apically with the periodontal ligament. The prevalence of DI ranges from 0.04% to 10%.3,4 Type I being the most common (79%) whereas Type II (15%) and III (5%) are more rarely encountered.5 The teeth most affected are the maxillary lateral incisors while posterior teeth are less likely to be affected.6 A bilateral invagination is a rare occurrence.6,7 The morphology of the crown can vary considerably, with deviations that, in the majority of the cases, can be detected during clinical examination, such as hypoplastic or hyperplastic appearance and infolds.8
The presence of an invagination increases the risk of caries and oral microbial contamination through the coronal aspect of the invagination, leading to infection of the root canal system, which may lead to pulpal and periradicular pathology. Depending on the pulpal and periradicular status, stage of root development and depth of the invagination, different modalities of endodontic therapy have been proposed, such as nonsurgical9,10 and/or surgical11,12,13 endodontic treatment and revascularization.14 Permanent teeth with immature roots diagnosed with pulp necrosis that are treated by apexification do not undergo further root development thus resulting in a poor crown-to-root ratio.15 Due to the remaining thin root walls, the fracture risk is also increased.16 For these reasons, when deemed necessary, the treatment of immature teeth with complex anatomy such as type III DI is always challenging, even for the experienced clinician.
The present case report describes the successful nonsurgical endodontic treatment of a maxillary central incisor diagnosed with type III DI, associated with incomplete root formation and apical periodontitis, while maintaining the vitality of the surrounding pulp.
CASE REPORT
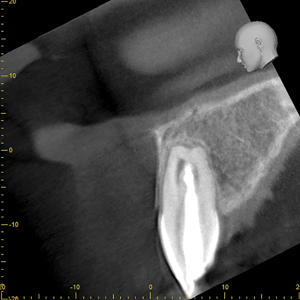
An eight-year-old Caucasian male patient was referred to a specialty private practice in Winnipeg, Manitoba, Canada, for evaluation and possible endodontic treatment of the right maxillary central incisor (#11). The patient presented with no pain or discomfort; however, his parents reported episodes of pain and swelling in the past with the need for analgesics and antibiotics to control the pain. The patient’s medical history was noncontributory and no known drug allergies were present. There was no history of dental trauma. Clinical signs of incomplete eruption and morphological variation (enlarged crown) were observed with a pronounced DI on the palatal surface. (Figs. 1A & 1B) There were no clinical signs of caries and no sinus tract was observed. The colour of the tooth did not differ from the adjacent teeth and the total number of teeth in the anterior region was normal. The tooth responded within normal limits to cold and to the electric pulp test (34/80). There was increased sensitivity to vertical percussion when compared to the adjacent teeth and slight palpation sensitivity was detected. Periodontal probing depth and mobility were within normal limits with minimal bleeding on probing. The radiographic examination revealed a type III invagination extending all the way from the crown to the apex. In addition, an immature root with a wide-open apex associated with a large periradicular radiolucency compatible with a lesion of endodontic origin (Fig. 2) was noted. Because of the complex anatomy of tooth #11, as revealed by the periapical radiograph, a limited field of view cone beam computed tomographic (CBCT) scan was advised as a supplemental examination. The coronal, axial and sagittal CBCT images showed that the invagination was separated from the main root canal with its own separate portal of exit. (Figs. 3A, 3B & 3C) The images also confirmed that tooth #11 had not yet completed root formation and that a low-dense diffuse image at the apical portion was present. Based on the clinical and radiographic examination, the diagnosis for tooth #11 was normal pulp. However, the DI was diagnosed with pulp necrosis and symptomatic apical periodontitis. The findings were discussed with the patient’s parents and a conservative treatment, where only the invagination would be disinfected, shaped and filled, without treating the main canal, was offered as the best option. Informed consent was obtained from the parents.
Fig. 1A

Fig. 1B

Fig. 2
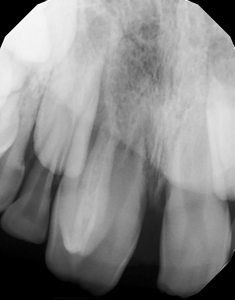
Fig. 3A

Fig. 3B

Fig. 3C

Local anesthesia was achieved with buccal infiltration of 4% articaine and epinephrine 1:200.000, rubber dam isolation was placed and the access cavity was prepared under 8 times magnification and illumination. Pulpal necrosis was clinically confirmed and the root canal was copiously irrigated with 2.5% sodium hypochlorite using a 30-gauge side-vented needle. The working length was measured using an electronic apex locator (EAL) and the canal was shaped using a reciprocating file system. Subsequently, the root canal was dried with paper points and a calcium hydroxide paste (Ultracal™ XS–Ultradent) was used as an intracanal medicament. The access opening was closed with a temporary filling and the patient was instructed to return after 30 days.
After 30 days, the tooth was anesthetized and isolated as previously described. The temporary filling was removed and the DI was thoroughly rinsed with 2.5% sodium hypochlorite and activated with a plastic sonic tip (EndoAcivator; Dentsply Sirona) in order to remove the calcium hydroxide. The canal was dried using paper points and a calcium hydroxide paste was placed once again as an intracanal medicament. The access was temporary sealed with an intermediate restorative material (IRM–Dentsply Sirona). The patient was instructed to return for the third session 90 days later at which point, the same procedures were conducted.
The final treatment session was scheduled to occur 9 months later, as per the patient’s request, as he commutes 4 hours for treatment. At this time, after profound anesthesia and proper rubber dam isolation were achieved, a #35 K-file was used to gently clean the canal walls while 17% EDTA was used to remove the smear layer. The canal was then dried using paper points and filled with gutta-percha and a Bioceramic sealer (Endosequence HiFlow–Brasseler) using the warm vertical compaction technique. The access was immediately sealed with a composite resin in order to avoid micro-leakage. (Fig. 4)
Fig. 4

Follow-up visits were performed at 12 and 36 months. At both follow-up appointments, the tooth displayed no discolouration and eruption continued to occur normally. (Figs. 5A & 5B) Additionally, the tooth responded positively to the cold test, which indicated that the pulp in the main root canal was vital. The patient was asymptomatic and the tooth was fully functional. There was no radiographic evidence of periradicular pathology and CBCT images demonstrated periradicular healing with resolution of the apical lesion, establishment of the periodontal ligament space, and completion of root growth. (Figs. 6A, 6B, 6C & 6D)
Fig. 5A

Fig. 5B

Fig. 6A
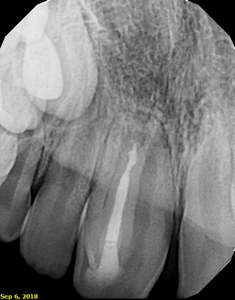
Fig. 6B

Fig. 6C
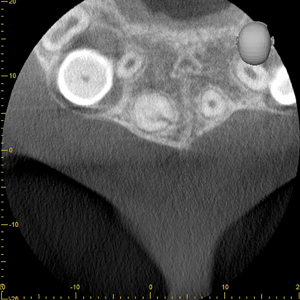
Fig. 6D
DISCUSSION
The present article reports on a challenging case where an immature tooth with a normal pulp and an open apex had a Type III DI with pulp necrosis and symptomatic apical periodontitis. The correct understanding of the morphology of the invagination and its relationship to the pulpal status of the main canal of the tooth was fundamental in order to establish an accurate treatment plan. Interestingly, due to the large periradicular radiolucency detected radiographically and previous episodes of pain and swelling, a non-responsive pulpal test was expected. However, the vitality of the pulp in the main root canal was seen to be maintained. The lack of communication between the vital pulp tissue in the main canal and the necrotic tissue in the invaginated canal explains the positive response to pulp testing. Preserving the vitality of the main canal was of paramount importance as further root development can be anticipated in the presence of a normal pulp.15,17 For that reason, non-surgical endodontic treatment was proposed solely on the invagination without treating the main canal.18 Endodontic treatment of the invaginated tooth can be challenging due to difficulties during access opening, cleaning, shaping and filling of the root canal system.19,20 In the present case, the canal in the DI was conservatively located with the aid of a dental operating microscope. Ricucci et al.21 reported that the invagination may contain remnants of the dental papilla that become necrotic and serve as a source of nutrients for bacterial flourishment. In addition, because of the communication with the oral environment, saliva can continuously seep into the invagination, also contributing to the delivery of bacteria and nutrients into this pseudo-canal.21
The use of a CBCT scanner provided relevant details of the internal anatomy of this invaginated tooth and allowed for accurate delineation of the extension of the periapical lesion. CBCT scan images are more precise than conventional periapical radiographs and provide the data necessary for the establishment of an accurate diagnosis, treatment plan and postoperative follow-up.20,22,23,24 After endodontic treatment or revascularization of immature permanent teeth, apical closure can be expected as the most consistent radiographic finding within a 1-year follow-up.25 In the current case report, CBCT images taken at the 12 and 36-month follow-up revealed complete apical closure, thickening of the root canal walls and the absence of periradicular pathology.
CONCLUSION
In this case report, the authors have demonstrated that nonsurgical conservative endodontic treatment of a complex Dens Invaginatus (DI) proved to be successful in promoting the healing of the periradicular tissues, while maintaining the vitality of the pulpal tissue in the main canal. Such an option should be contemplated and attempted as a first choice, regardless of the size of the periradicular pathology. CBCT images are an essential tool in the diagnosis and management of teeth with complex anatomy.
Oral Health welcomes this original article.
References
- Hülsmann M. Dens invaginatus: aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J 1997;30:79-90.
- Oehlers FA. Dens invaginatus (dilated composite odontome). I. Variations of the invagination process and associated anterior crown forms. Oral Surg Oral Med Oral Pathol 1957;10:1204-18 contd.
- Alani A, Bishop K. Dens invaginatus. Part 1: classification, prevalence and aetiology. Int Endod J 2008; 41:1123-36.
- Kusgoz A, Yildirim T, Kayipmaz S, Saricaoglu S. Nonsurgical endodontic treatment of Type III dens invaginatus in maxillary canine: an 18-month follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:e103-6.
- Ridell K, Mejàre I, Matsson L. Dens invaginatus: a retrospective study of prophylactic invagination treatment. Int J Paediatr Dent 2001;11:92-7.
- Grahnen H, Lindahl B, Omnell K. Dens Invaginatus. I. A clinical, roentgenological and genetical study of permanent upper lateral incisors. Odontologisk Revy 1959; 10:115–37.
- Swanson WF, McCarthy FM Jr. Bilateral dens in dente. J Dent Res 1947;26:167-71.
- Rotstein I, Llamosas E, Choi K-S. Endodontic therapy in teeth with anatomical variations. In: Rotstein I, Ingle JI, editors. Ingle’s Endodontics. 7th ed. Raleigh, NC: PMPH USA; 2019. p. 866–9.
- Brooks JK, Ribera MJ. Successful nonsurgical endodontic outcome of a severely affected permanent maxillary canine with dens invaginatus Oehlers type 3. J Endod 2014; 40:1702-7.
- Goel S, Nawal RR, Talwar S. Management of Dens Invaginatus Type II Associated with Immature Apex and Large Periradicular Lesion Using Platelet-rich Fibrin and Biodentine. J Endod 2017;43(10):1750-1755.
- Chaniotis AM, Tzanetakis GN, Kontakiotis EG, Tosios KI. Combined endodontic and surgical management of a mandibular lateral incisor with a rare type of dens invaginatus. J Endod 2008;34:1255-60.
- Vier-Pelisser FV, Pelisser A, Recuero LC, Só MV, Borba MG, Figueiredo JA. Use of cone beam computed tomography in the diagnosis, planning and follow up of a type III dens invaginatus case. Int Endod J 2012;45:198-208.
- Wayama MT, Valentim D, Gomes-Filho JE, Cintra LT, Dezan E Jr. 18-year follow-up of dens invaginatus: retrograde endodontic treatment. J Endod 2014;40:1688-90.
- Yang J, Zhao Y, Qin M, Ge L. Pulp revascularization of immature dens invaginatus with periapical periodontitis. J Endod 2013;39:288-92.
- Lee S, Park YT, Setzer FC. Combined Regenerative and Vital Pulp Therapies in an Immature Mandibular Molar: A Case Report. J Endod 2020;46:1085-1090.
- Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol 2002;18:134-7.
- Bishop K, Alani A. Dens invaginatus. Part 2: clinical, radiographic features and management options. Int Endod J 2008;41:1137-54.
- Gonçalves A, Gonçalves M, Oliveira DP, Gonçalves N. Dens invaginatus type III: report of a case and 10-year radiographic follow-up. Int Endod J 2002; 35:873-9.
- Ballal S, Sachdeva GS, Kandaswamy D. Endodontic management of a fused mandibular second molar and paramolar with the aid of spiral computed tomography: a case report. J Endod 2007;33:1247-51.
- Vier-Pelisser FV, Morgental RD, Fritscher G, Ghisi AC, Borba MG, Scarparo RK. Management of type III dens invaginatus in a mandibular premolar: a case report. Brazilian Dental Journal 2014; 25:73-8.
- Ricucci D, Milovidova I, Siqueira JF Jr. Unusual Location of Dens Invaginatus Causing a Difficult-to-Diagnose Pulpal Involvement. J Endod 2020;46:1522-1529.
- Fernández R, Cadavid D, Zapata SM, Alvarez LG, Restrepo FA. Impact of three radiographic methods in the outcome of nonsurgical endodontic treatment: a five-year follow-up. J Endod 2013;39:1097-103.
- Kfir A, Telishevsky-Strauss Y, Leitner A, Metzger Z. The diagnosis and conservative treatment of a complex type 3 dens invaginatus using cone beam computed tomography (CBCT) and 3D plastic models. Int Endod J 2013;46:275-88.
- Silva E Souza Pde A, de Almeida BV, Tartari T, Alves AC, Tuji FM, Silva E Souza MH Jr. A clinical report of Type III dens invaginatus: relevant aspects of a combined therapeutic approach. Gen Dent 2013;61:56-9.
- Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod 2012;38:1330-6.
About the Authors
 Rodrigo Cunha has a Private Practice limited to Endodontics in Winnipeg–Manitoba. Dr. Cunha is the Founder of the Winnipeg Endodontic Study Group.
Rodrigo Cunha has a Private Practice limited to Endodontics in Winnipeg–Manitoba. Dr. Cunha is the Founder of the Winnipeg Endodontic Study Group.
 Alanna Junaid graduated from the University of Manitoba in 2014. Since that time, she has been practicing as a general dentist in Winnipeg.
Alanna Junaid graduated from the University of Manitoba in 2014. Since that time, she has been practicing as a general dentist in Winnipeg.
 Giselle Nevares has a Private Practice Limited to Endodontics in Recife–Brazil. She is also an Assistant Professor at Centro Odontológico de Estudos e Pesquisas (COESP).
Giselle Nevares has a Private Practice Limited to Endodontics in Recife–Brazil. She is also an Assistant Professor at Centro Odontológico de Estudos e Pesquisas (COESP).












