
A case is presented on how an endodontic infection can contribute to extra-oral sinus tract, and the problems in diagnosis that can be related to this type of case. A literature search failed to show a pictorial progression of a cutaneous sinus tract. This report, with help from the patient, shows a diagrammatic progression of the skin lesion to a patent sinus tract on the skin surface. This report also shows difficulty of diagnosis, both within dermatology and also within the dental discipline of endodontics.
Kay (name substituted for privacy reasons) is a 25 year-old female. Kay has a medical history of angioedema and multiple sclerosis (MS). She reports and allergy to penicillins and azithromycin. Her medications include Levonorgestrel for birth control, Ocrelizumab for MS and anti-histamines as needed for her angioedema.
In Jan 2020 Kay presented at the Emergency Room (ER) of her local hospital complaining of left-sided facial swelling and palatal swelling on the same side. Kay was given antibiotics and advised to see her dentist by the ER staff. Kay proceeded to go to her dentist, who after examining her said everything appeared to be normal, and that the palatal swelling could possibly be linked to her angioedema. The facial swelling subsided, and all seemed to be fine.
After a period of about 18 months, the facial swelling returned. Kay’s dentist wasn’t sure that it was a tooth, as the dental diagnosis was elusive. It was suspected the facial swelling was angioedema, so Kay’s dentist arranged to have her referred to a dermatologist. Kay explained to the dermatologist that she was getting a bruise on her face. (Fig. 1, photo provided by patient)
Fig. 1

Kay reported she was given a steroid cream, antibiotics and antifungals. The discomfort continued, and the facial lesion that resembled a bruise progressed to a dimpled structure. (Fig. 2)
Fig. 2

The left-facial lesion progressed until swelling was evident with a yellow head on the raised lesion. (Fig. 3)
Fig. 3

When the lesion became raised, Kay reports going back to her dermatologist who proceeded to lance and squeeze the lesion. Kay described this as some of the most intense pain she has ever felt. Furthermore, this action failed to resolve the lesion. In some desperation, Kay went back to her dental office who referred her to our endodontic specialty office.
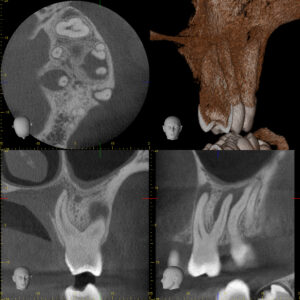
Upon meeting Kay, her appearance at that time was as follows in Fig. 4. Strangely, her initial endodontic examination was normal in all regards. However, her clinical examination did not match her radiographic appearance, as the periapical radiograph suggested rarefaction was present between 26 and 27. Furthermore, PA and CBCT imaging was consistent with apical rarefaction at the apex of each root of 26. (Figs. 5 &6)
Fig. 4

Fig. 5

Fig. 6
The clinical exam was re-performed and Kay reported feeling cold to dry cotton pellet application on 25, 26 and 27. The cold test was determined to be unreliable in this case, and thus was not considered in the diagnosis. In light of this new information, a diagnosis of 26 pulp necrosis with (probable) chronic apical abscess was determined.
Kay’s treatment was performed in two stages. The first was access and calcium-hydroxide (CaOH) placement. Three months after initial treatment with CaOH Kay presented for follow up with her facial lesion as shown in Fig. 7.
Fig. 7

The case was completed approximately 7 months after the initial treatment. On the day of completion, the facial lesion is shown in Figs. 8 and 9, while the final radiograph is also shown.
Fig. 8

Fig. 9

The case was re-evaluated approximately 18 months after the initiation of the root canal therapy. It can be seen in the Pre-Operative coronal view CBCT of the MB root that bone was missing around the entire apex. Apical areas that penetrate the buccal cortex may be at risk for hypochlorite accidents, fortunately this was not the case here.1 After 18 months of healing, the bone has regenerated around the MB root. (Fig. 11 & 12)
Fig. 10

Fig. 11

Fig. 12
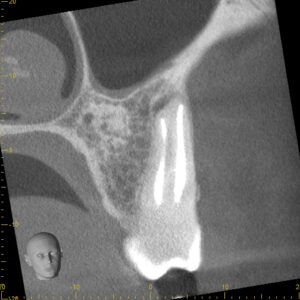
Similar bony regenerative properties of non-surgical endodontic treatment can be seen around the palatal root. (Figs. 13 & 14)
Fig. 13

Fig. 14

The cutaneous appearance approximately 18 months after treatment is seen in Fig. 15.
Fig. 15

Cutaneous sinus tracts are an uncommon presentation from necrotic teeth, that are typically found in a 4:1 ratio favouring mandibular teeth2 over maxillary teeth. When the buccinator muscle is attached coronal to the apical foramen, exudate will tend to collect in the buccal space. The lateral border of the buccinator space is the overlying skin and subcutaneous tissue. Regardless of the proximity of exudate in the buccal space to the skin surface, in most circumstances a cutaneous sinus tract does not form. In this case, the length of each root was in the 23-25mm range, long enough to be beyond the buccinator attachment, ultimately collecting in the buccal space and resulting in a cutaneous sinus tract. The most common sinus tract presenting on facial skin is dental infection, yet it is often not considered as early in the differential diagnosis as it should be.4 Unfortunately, many patients who experience cutaneous sinus tracts are misdiagnosed for extended periods, with at least half being submitted to dermatological surgical procedures.3 In Kay’s circumstance, her dermatological lancing, and various drugs to treat her skin condition was unnecessary, as the treatment of choice was non-surgical root canal treatment. It is encouraged in the dermatological and dental communities to consider an odontogenic origin if a cutaneous sinus tract is observed. In Kay’s case, it would appear that a facial scar may be the result of the dermatological incision. Surgical intervention of cutaneous sinus tracts should only be considered once odontogenic origin has been ruled out.
Oral Health welcomes this original article.
References
- Souza,EM at al. Mapping the periapex anatomical pattern of teeth involved in sodium hypochlorite accidents: a cross-sectional quasi-experimental study. Int End J. Aug 2021.54:8. 1212-1220
- Muzaffer,E. et al. Treatment of extraoral cutaneous sinus tracts with non-surgical endodontic intervention: report of six cases. J Istanb Univ Fac Dent. 2015; 49(2): 35–40.
- Cantatore JL, et al. Cutaneous dental sinus tract, a common misdiagnosis: a case report and review of the literature. Cutis. 2002;70:264–7.
- Lewin-Epstein J, et al. Cutaneous sinus tracts of dental origin. Arch Dermatol 1978; 114: 1158–1161.
About the Author

Dr. Campbell spent the first half of his career in the Armed Forces as a General Dentist. The second half of his career has been spent as a board-certified specialist in Endodontics. He is the Head of Endodontics at the University of Alberta, and enjoys private practice in Edmonton and in the Comox Valley.










