Implant supported dentures provide many individuals with a better quality of life, but this is not without some challenges. Specifically, what is the recommended self-care for this type of prosthesis? There are two areas for discussion: removable dentures and fixed dentures.
Research in the area of implant self-care is limited and often based on low-level evidence or expert opinion.1 The 11th European Workshop on Periodontology on the primary prevention of peri-implantitis, reported that manual and powered toothbrushes are an effective tool for managing peri-implant mucositis when combined with a professional maintenance program.2 This does not give dental professionals much to go on and neglects to clarify if the evidence is based on research for a single implant, multiple implants, or implants for edentulous individuals.
Self-care for implant supported dentures
A consensus report initiated by the American College of Prosthodontists provides clinical practice guidelines for recall and maintenance for people with implant supported dental restorations.3 The recommendations for at-home maintenance for implant supported removable full dentures include tooth brushing the implant components twice daily with a soft bristled brush and the use of a topical oral agent. The prosthesis is cleaned twice a day with a soft brush and a denture-cleaning agent and removed and stored in a cleaning solution when sleeping.
Recommendation for fixed implant supported dentures is similar, with twice daily brushing and the use of interdental aids adapted for cleaning under the denture and around the implant, if access is possible. Use of an oral topical agent is also advised.3
Professional intervention including oral hygiene instructions and mechanical debridement show a reduction in clinical signs of inflammation but added measures such as antimicrobial agents, antibiotics, or air-abrasives did not provide an added benefit.2 Recommended intervals for professional intervention is 6-months or more frequently if the patient has confounding risk factors.3
Case Report
The lack of good evidence prompted a question–Is a manual toothbrush and water flosser an effective regimen for cleaning around implant components of removable dentures? The study was approved by the university institutional review board for human subjects and registered on clinicaltrials.gov (NCT04462341). The study was designed to compare two oral hygiene regimens: manual toothbrush and water flosser (Fig. 1) or manual toothbrush only. The primary focus was bleeding on probing outcomes around the implants over 6 weeks. Due to the ongoing COVID-19 pandemic, recruitment was suspended and months later the study was closed.
Fig. 1A

Fig. 1B

A 75-year-old black woman under medical treatment for hypertension and high cholesterol was able to attend all treatment visits prior to ending the study and provides a snapshot of one case using a water flosser. She has a mandibular implant supported denture with two implants at #33 and #43 and was attentive to her oral hygiene. (Table 1) Initially, bleeding on probing was present on 7 of 8 sites with no mobility, and probing depths ranged from 2-4 mm. (Table 2) The gingiva on marginal ridge was also assessed with no redness or swelling evident. The denture was cleaned ultrasonically, and the implants were debrided using hand scalers with an implant specific tip.
Table 1
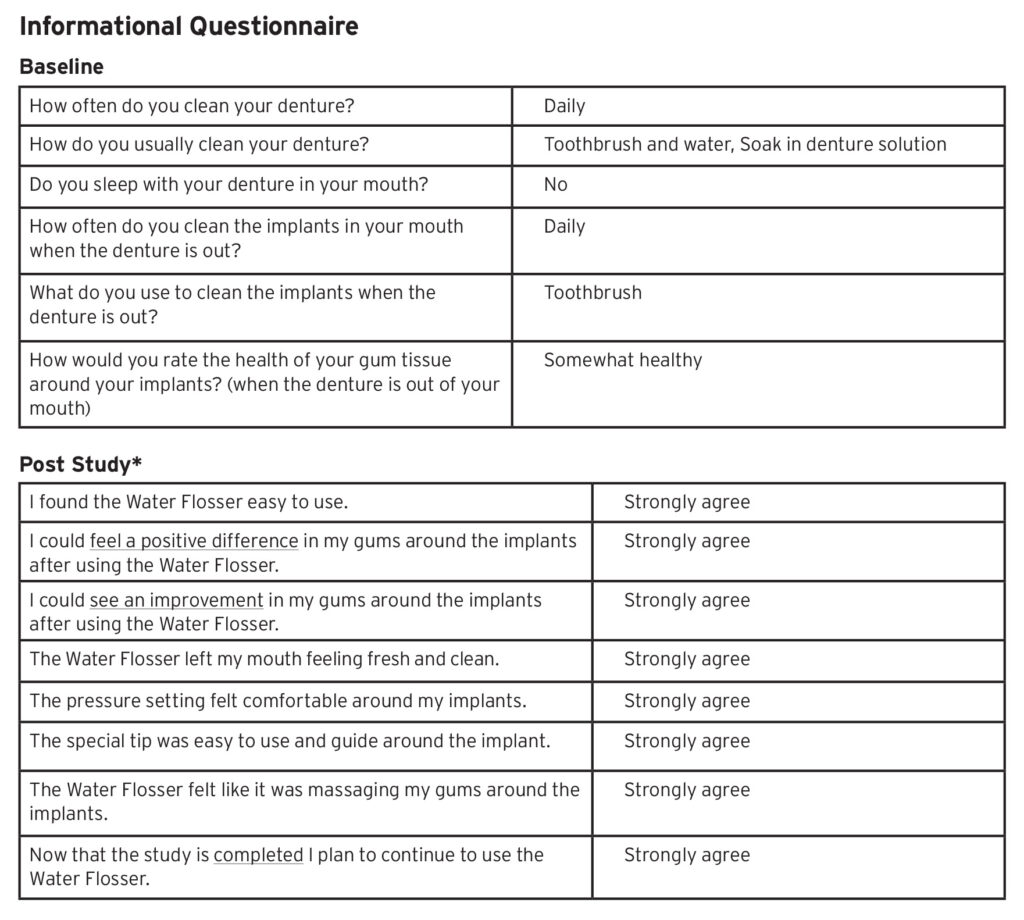
*All statements had a Likert Scale answer choice of Strongly agree to Strongly disagree.
Table 2

A demonstration, verbal and written instructions on the water flosser and implant tip was provided. She continued cleaning her denture as she normally did, used the water flosser around the study implants twice a day, gradually increasing the pressure to setting #7 (based on her comfort level), and recorded the setting and usage in a diary.
At 3-weeks, bleeding on probing was found at 4 sites (only on implant #43) with no edema or redness on the mandibular ridge. The diary showed consistent use of the water flosser and cleaning of the denture. At 6-weeks, bleeding on probing was found at 1 site and no edema or redness was found on the mandibular ridge. (Fig. 2) The subject was compliant and happy with the results. (Table 1) The probe was placed as close to the mesial, buccal, distal and lingual of the implant at each visit. Probing depths show a 1 mm variation in both directions most likely due to potential site difference in probe placement due to implants not having anatomical guidance to improve repeatability of probe placement.
Fig. 2A

Fig. 2B

Summary
Evidence for the optimum maintenance of implant supported restorations is lacking, is of poor quality, or based on empirical or traditional protocols for natural dentitions.1,3 Research is badly needed. In the meantime, dental professionals must make decisions for their patients. Recommending a Waterpik Water Flosser with specialized tips (Figs. 1 & 3) may be helpful.
Fig. 3

Oral Health welcomes this original article.
References
- Bidra AS. Daubert CM, Garcia LT et al. A systematic review of recall regimen and maintenance regimen of patients with dental restorations-Part 2: implant-borne restorations. J Prosthodont 2016; 25:S16-S31.
- Jepsen S, Berglundh T, Genco R, et al. Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol 2015; 42(Suppl.16):S152-S157.
- Bidra AS, Daubert DM, Garcia LT, et al. Clinical practice guidelines for recall and maintenance of patients with tooth-borne and implant-borne dental restorations. J Prosthodont 2016; 25:S32-S40.
About the Author
 Dr. Magnuson is Associate Professor and Assistant Director of Biostatistics and Experimental Design, Tufts University, School of Dental Medicine, Boston, MA. She has clinical research experience in the fields of oral hygiene, tooth whitening, dental restorative materials, and Sjögren’s Syndrome. She has published articles, abstracts, and book chapters and had poster presentations at scientific meetings on these subjects.
Dr. Magnuson is Associate Professor and Assistant Director of Biostatistics and Experimental Design, Tufts University, School of Dental Medicine, Boston, MA. She has clinical research experience in the fields of oral hygiene, tooth whitening, dental restorative materials, and Sjögren’s Syndrome. She has published articles, abstracts, and book chapters and had poster presentations at scientific meetings on these subjects.
 Deborah Mancinelli-Lyle is Director, Professional & Clinical Affairs, Water Pik, Inc. Her 40-year career includes positions in clinical practice, education, and corporate research. Deborah has presented numerous lectures on oral disease prevention and health promotion, worldwide. She has written over 55 articles and research manuscripts.
Deborah Mancinelli-Lyle is Director, Professional & Clinical Affairs, Water Pik, Inc. Her 40-year career includes positions in clinical practice, education, and corporate research. Deborah has presented numerous lectures on oral disease prevention and health promotion, worldwide. She has written over 55 articles and research manuscripts.












