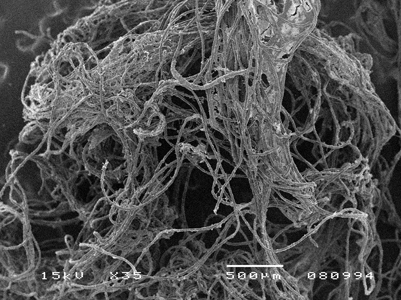
It would be beneficial if there was evidence on how to maintain implants that is measurable and predictable. Much of the information is empirical and based on the assumption that traditional oral hygiene for natural teeth will be the same for implants. In some cases this may be true, but for many it is misguided. (Figs. 1, 2 & 3)
Fig. 1

Fig. 2

Fig. 3

There are two parts to implant maintenance and success after placement: regular assessment and debridement by the dental team and daily personal oral hygiene methods.1,2 A maintenance program for the prevention of peri-implant diseases can prevent biologic complications and promote long-term success if the patient adheres to the regimen.1 Implant therapy to treat peri-implant diseases has shown a high success rate over time.2
DENTAL IMPLANT SELF-CARE
Mechanical plaque control is the cornerstone of prevention of oral disease and requires a high standard of care, on a daily basis. This is a challenge for most people with natural teeth. Some implants make it that much harder and near impossible. How can we help our patients?
Tooth brushing
There is limited research using a powered toothbrush with implants. An oscillating-rotating (OR) toothbrush with an implant brush head used with single implants was more effective for plaque removal but there was no difference for bleeding on probing (BOP) or probing pocket depth, compared to manual brushing at 3 months.3 A 12-month observational study using an OR toothbrush on implant-retained partial or full dentures showed slight improvements from baseline to 12 months for bleeding, probing, and recession but the differences were clinically negligible and no comparisons to a different oral hygiene regimen was evaluated.4 The effect of an OR toothbrush on peri-implant mucositis in the aesthetic areas found an improvement in bleeding at 3 months that continued to be maintained for 12 months, but there was no comparison to other oral hygiene regimens.5 A simple comparison of an OR toothbrush and a manual toothbrush used to clean implants supporting a complete removable overdenture showed no difference between the brushes.6
A sonic toothbrush showed more frequent brushing per day and longer brushing duration compared to manual brushing in a 2-month study. However, there were no differences in clinical parameters between the groups.7 A 6-month study did show the sonic toothbrush was significantly more effective than a manual toothbrush for plaque and bleeding indices but not for gingival index (GI) or probing pocket depth around implants.8 However, in a 12- month study there was no difference between a sonic toothbrush and a manual toothbrush for plaque index (PI), BOP, GI or for clinical attachment level, microbiological and immunological measures around implants or natural teeth.9
A systematic review from 2015 reported that there was not enough evidence to say that powered toothbrushes were effective in the management of peri-implant mucositis.10
Flossing
Dental floss is often recommended for cleaning the interdental area between the implant and natural teeth. This may work fine depending on the size and shape of the prosthesis. If it is not easy to move the floss under the prosthesis, then it may not be the best choice for the patient. Tufted floss is often recommended anecdotally along with the cross-over flossing technique. Clinicians need to be very vigilant for any changes in mucosal tissue, as floss may be more of a problem than a help as noted in published case study reports.
An observational study evaluated 10 cases of peri-implant disease that were not responding to therapy. These individuals were in an intensive oral hygiene program that consisted of supra- and submucosal debridement and plaque, bleeding and probing depth assessment on a regular basis. Radiographs were taken every two years.11 Since there was no resolution of the peri-implant mucositis and the presence of bleeding on probing plus suppuration or bone loss was evident, exploratory surgery was performed. In all 10 cases, remnants of tufted floss were found around the rough part of the implant. The floss threads were removed and nine of the cases resolved. Once the floss was removed, follow-up visits showing no bleeding on probing and pocket depth reduction. One case showed pocket depth reduction but there was still bleeding on probing. All the patients had single implants allowing for optimal oral hygiene.
A case report with a 6-year follow-up had a similar outcome. A 66 year old man was referred to the Bologna University, Division of Periodontology and Implantology for a chronic peri-implant mucositis around four mandibular implants.21 The patient also reported chin pain, recurrent swelling and spontaneous bleeding. Peri-implant mucositis was evident clinically and peri-implantitis was revealed on the radiographs. Probing of the area was painful and did not produce readings consistent with the radiographic bone loss. Exploration with a perioscope showed a filamentous foreign body that turned out to be remnants of tufted floss. (Fig. 4) The floss was removed, and complete remission was observed in 10 days. (Fig. 5) The microflora reverted back to a healthy environment and six years later clinical and radiographic data showed stable implants and healthy tissue.
Fig. 4

Fig. 5
Based on these case reports, caution is advised when recommending tufted floss.
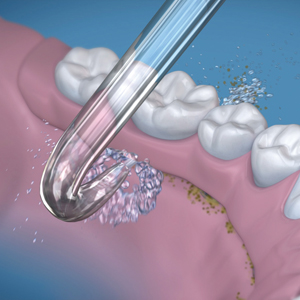
Oral irrigator/ water flosser
A water flosser has been compared to brushing and flossing with single implants and was twice as effective for reducing bleeding and preferred by the patients. (Fig. 6)13 Water flossing was also compared to the CIOTIPlus systematic brushing sequence (chewing, inside, outside) followed by tongue cleaning and interdental cleaning with dental floss or interdental brushes, and then a second brushing.14 The water flossing group showed a significantly better reduction in mucositis severity score compared to the CIOTIPlus group.
Fig. 6

The hydrodynamic shear forces of pulsating water allow access around the implant interface and the prosthesis, where other devices cannot reach. This is a promising, easy and logical way to clean implants.
A new tip designed to direct the water under an implant retained denture was introduced to the market for use with a Waterpik® Water Flosser. (Fig. 7) The tip is used from the lingual area and directed under the denture.
Fig. 7
Interdental brushes
There is very little information about the efficacy of interproximal brushes (IB) with implants. A cross-sectional study evaluated the accessibility of interdental brushes (0.5 mm) and the peri-implant condition. Fifty patients with 171 implants were included in the study. Fifty-four percent of the prostheses prevented access for proper proximal cleaning. Subjects with good access had a 62% prevalence of peri-implant disease vs 80% for those with poor access.15
A cross-over study compared the plaque removal ability of a straight soft IB and a waist-shaped IB.16 Both natural teeth and implants (n=102) providing 816 sites were included in the study, but the efficacy was not reported separately. The waist-shaped IB provided better plaque removal for all aspects of the tooth or implant evaluated, with the exception of the buccal sites.
Another study evaluated a waist-shaped IB against a straight IB for cleaning the implants for over dentures in elderly patients. In this case, two brushes were used on either side of the implant and there was no difference between the brushes.17
SUMMARY
It is glaringly obvious that the evidence for preventing and controlling peri-implant diseases is lacking. Logically, single implants can be maintained, similarly to natural teeth, if the prosthesis allows access and the risk factors are minimized. There is a need for innovation and data to support patients with advice on the best self-care for different types of implants and prosthetics. Denture retained implants are a challenge for both dental professionals and patients alike.
As the placement of implants is commonplace, the incidence of peri-implant mucositis and peri-implantitis will continue to be a problem impacting oral health and quality of life. More research and innovation are needed in this area.
Oral Health welcomes this original article.
References
- Monje A, Aranda L, Diaz KT et al. Impact of maintenance therapy for the preventions of peri-implant diseases: a systematic review and meta-analysis. J Dent Res 2016; 95(4):372-379.
- Roccuzzo M, Layton DM, Roccuzzo A, Heitz-Mayfield LJ. Clinical outcomes of peri-implantitis treatment and supportive care: A systematic review. Clin Oral Impl Res 2018; 29(Suppl 16):331-350.
- Allocca G, Pudylyk D, Signorino F, Grossi GB, Maiorana C. Effectiveness and compliance to an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial. Int J Impl Dent 2018; https//doi.org10.1186/s40729-018-0150-6.
- Vandekerckhove B, Wuirynen M, Warren PR, Strate J, van Steenberghe D. The safety and efficacy of a powered toothbrush on soft tissues in patients with implant-supported fixed prostheses. Clin Oral Invest 2004; 8:206-210.
- Rasperini G, Pellefrini G, Cortella A et al. The safety and acceptability of an electric toothbrush on peri-implant mucosa in patients with oral implants in aesthetic areas: a prospective cohort study. Eur J Oral Implantol 2008;1(3):221-228.
- Tawse-Smith A, Duncan W, Payne AGT, Thomson WM, Wennström JL. Relative effectiveness of powered and manual toothbrushes in elderly patients with implant supported mandibular overdentures. J Clin Periodontol 2002;29():275-280.
- Lee J, Lim JH, Lee J et al. Efficacy of sonic-powered toothbrushes for plaque removal in patients with peri-implant mucositis. J Periodontol Impl Sci 2015;45:56-61.
- Wolff L, Kim A, Nunn M, Bakdash B, Hinrichs J. Effectiveness of a sonic toothbrush in maintenance of dental implants. A prospective study. J Clin Periodontol 1998;25(10):821-828.
- Swierkot K, Brusius M, Leismann D et al. Manual versus sonic-powered toothbrushing for plaque reduction in patients with dental implants: an explanatory randomized controlled trial. Eur J Oral Implantol 2013;6(2):133-144.
- Salvi GE, Ramseier CA. Efficacy of patient-administered mechanical and/or chemical plaque control protocols in the management of peri-implanti mucositis. A systematic review. J Clin Periodontol 2015; 42(Suppl16):S187-S201.
- Van Velzen FJJ, Lang NP, Schulten EAJM, Ten Bruggenkate CM. Dental foss as a possible risk for the development of peri-implant disease: an observational study of 10 cases. Clin Oral Impl Res 2015;00:1-5.
- Montevecchi M, De Blasi V, Checchi L. Is implant flossing a risk-free procedure? A case report with a 6-year follow-up. Int J Oral Maxillofac Impl 2016;31:e790-e83.
- Magnuson B, Harsono M, Stark PC, Lyle D, Kugel G, Perry R. Comparison of the effect of two interdental cleaning devices around implants on the reduction of bleeding: A 30-day randomized clinical trial. Compend of Contin Ed in Dent 2013; 34(Special Issue 8):2-7.
- Bunk D, Eisenburger M, Häckl S, Eberhard J, Stiesch M, Grischke J. The effect of adjuvant oral irrigation on self-administered oral care in the management of peri-implant mucositis: a randomized controlled clinical trial. Clin Oral Impl Res 2020;00:1-13. DOI: 10.1111/clr.13638.
- Pons R, Nart J, Valles C, Salvi GE, Monje A. Self-adminstered proximal implant-supported hygiene measures and the association to peri-implant conditions. J Periodontol 2020;1-11.
- Chongcharoen N, Lulic M, Lang NP. Effectiveness of different interdental brushes on cleaning the interproximal surfaces of teeth and implants: a randomized controlled, double-blind cross-over study. Clin Oral Impl Res 2011;23:635-640.
- Chen Q, Ge Y, Chai J, Feng H, Liu J, Pan S. The effectiveness of waist-shaped and straight-shaped interdental brushes in cleaning implant overdenture attachments: a self-controlled clinical trial. J Oral Implantol. In review process.
About the Author
 Deborah M. Lyle is the Director of Clinical and Professional Affairs at Water Pik, Inc. Her 40-year career includes positions in clinical practice, education, and corporate research. Deborah has presented numerous lectures on oral disease prevention and health promotion, worldwide. She has written over 55 articles and research manuscripts and received the ADHA/Johnson & Johnson Dental Hygiene Award of Excellence and the IADR/Colgate Oral Health Research Award.
Deborah M. Lyle is the Director of Clinical and Professional Affairs at Water Pik, Inc. Her 40-year career includes positions in clinical practice, education, and corporate research. Deborah has presented numerous lectures on oral disease prevention and health promotion, worldwide. She has written over 55 articles and research manuscripts and received the ADHA/Johnson & Johnson Dental Hygiene Award of Excellence and the IADR/Colgate Oral Health Research Award.












