Introduction
A hematoma is an abnormal collection of blood outside of a vessel that is still confined within a tissue space. A common cause of a hematoma is traumatic injury to a blood vessel wall. The location of the blood accumulation can have differing consequences depending on its compressive effects against adjacent anatomic structures. One well known example of this is the development of an epidural hematoma resulting from hemorrhage of the middle meningeal artery. This hematoma forms in the space between the dura mater and the inner table of the skull, causing compression of the brain with neurologically debilitating effects. 1 Within the dental literature, floor of mouth hematomas have been reported to be potentially life-threatening complications subsequent to mandibular implant placements. 2,3 Even routine procedures such as local anaesthesia administration via the inferior alveolar nerve block have been shown to induce hematomas possibly through needle injury to intraneural blood vessels. 4 With regards to facial trauma, subcutaneous hematomas are a common clinical finding for soft tissue injuries. 5,6 Another well recognized location of hematoma formation is a nasal septal hematoma. These typically occur following nasal trauma and if untreated, may lead to septal necrosis perforation and late-developing saddle nose deformities. Such hematomas are also more frequently observed in children post-nasal injury. 7-10 However, detailed reports of traumatic hematomas occurring elsewhere in the pediatric cranio-maxillofacial anatomy are exceedingly rare. Herein, we report the unusual formation of a hematoma within the deep temporal space of a pediatric patient secondary to blunt trauma sustained during a fall.
Case Report
The patient is a 4-year-old male who presented to the IWK Children’s Hospital emergency department in Halifax, Nova Scotia following a fall on ice while playing outdoors. The child fell from standing height with the majority of the impacted sustained to his left face. There was no noted loss of consciousness by witnesses. On arrival, he was alert, cooperative, neurologically intact (Glasgow Coma Scale score 15/15), and hemodynamically stable. There were no focal neurological deficits or other injuries detected on examination. No edema or other abnormality in the area of impact was observed clinically. Past medical history was unremarkable except for three previous episodes of otitis media treated without complications. His parents denied any drug allergies or familial coagulopathies. Given the mechanism of injury, the Otolaryngology service was consulted to rule out a temporal bone fracture or ear canal pathology. Computed tomography (CT) imaging of the head and facial bones was obtained and did not display any evidence of skull fracture or intracranial involvement. The family was reassured, discharged home with instructions, and prescribed a seven-day course of Cephalexin for recurrent otitis media that was incidentally discovered on otoscopic examination.
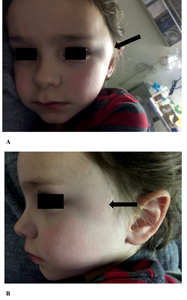
Over the next four days, there were no symptoms displayed of otitis media, but the parents noticed increasing swelling in the left temporal region. The patient also complained of increasing pain in this region. Given these changes, the patient and family returned to the emergency room for re-evaluation. The patient was examined by the emergency physician, and the Oral and Maxillofacial Surgery service was consulted. He was again found to have stable vital signs and was afebrile. Head and neck examination revealed an area of edema approximately 3×3 cm located in the left temporal region, immediately posterior to the lateral canthus. It was noted to have a blue hue in coloration, with no obvious cutaneous erythema (Fig. 1). The swelling was mildly fluctuant and was tender to palpation. Neurological screening examination and cranial nerves I-XII were normal on exam. Otoscopic exam was normal with visible tympanic membranes and no hemotympanum or discharge. The patient did not have trismus and there were no remarkable intra-oral findings.
Fig. 1
Clinical photograph of left temporal swelling upon initial presentation (arrow). A) Frontal view. B) Lateral view.
Based on the recent fall to the left face and along with the physical findings, our differential diagnosis at this time included hematoma, abscess, pseudoanuerysm, or neoplasm. Re-examination of the CT scan taken a few days earlier once again confirmed the absence of any skull or facial bone fractures. However, it was noted that there was a hypodensity consistent with a fluid-filled collection in the left deep temporal space (Fig. 2). This entity also had a slight rim enhancing appearance. Thus, CT images narrowed the differential diagnosis to either a hematoma or an abscess confined to this rarely affected anatomical space. It was also confirmed there were no missed intracranial abnormalities on the CT.
Fig. 2
Head and facial bones CT imaging with white arrow indicating the fluid-filled collection in the deep temporal space appearing as a radiolucency. No associated fractures or intracranial abnormalities noted. A) Axial view B) Coronal view.

Although the CT imaging showed a solitary, fluid-filled entity within the left deep temporal space, it was not possible at this point to determine if the collection represented an abscess or a hematoma. Therefore a decision was made to confirm the diagnosis by performing a fine-needle aspirate (FNA) of the lesion. The patient’s consent was obtained through the parents. A combination of intranasal fentanyl (at a dose of 1 µg/kg) and midazolam (at a dose of 0.1 mg/kg) was administered for mild sedation and topical anesthetic (EMLA cream) was applied to the left temporal region. Using palpation, the area of most fluctuance was identified and a 20-gauge needle was introduced. This was immediately followed by positive aspiration of approximately 2ml of sero-sanguineous fluid. Gross examination of the aspirated fluid was not consistent with purulent exudate, however, they were still sent for culture and sensitivity testing. Importantly, it was noted that upon puncture to the space there was a noticeable decompression detected. Gauze and pressure dressing was subsequently applied to the injection site which further drained more sero-sanguineous fluid. The patient was then placed in a head-wrap dressing (Barton’s wrap) ensuring pressure over the left temporal region. The patient was admitted overnight for observation. The patient had an unremarkable hospital stay and was discharged home in the care of his parent’s the following day. The parents were given instructions on how to change the Barton dressing on a daily basis until the follow-up appointment scheduled three days later.
Final microbiological analysis (after 48 hours of incubation) from the FNA contents showed no growth of organisms, hence ruling out an abscess or infected hematoma. On follow-up appointment three days later, the left temporal swelling had subsided remarkably, and there were no signs or symptoms of infection in the area. A follow-up appointment one-week later, and again four months later, showed no remarkable findings other than resolution of the left temporal region swelling, along with restoration of facial symmetry (Fig. 3). The patient showed no alterations of mental status or focal neurological concerns at each follow-up appointment. The parents raised no concerns regarding his recovery.
Fig. 3
Head and facial bones CT imaging with white arrow indicating the fluid-filled collection in the deep temporal space appearing as a radiolucency. No associated fractures or intracranial abnormalities noted. A) Axial view B) Coronal view.

Discussion
The clinical, radiographic and procedural findings of this case were consistent of a hematoma in the left deep temporal space secondary to blunt trauma. Although subcutaneous hematomas secondary to maxillofacial trauma is a common sequelae of injury 6,10,11 the description of hematoma formation specifically in the temporal region of the cranio-maxillofacial anatomy is rare, especially for the pediatric patient. To this date, there has only been one other report of a temporal hematoma which occurred on the right temporal region that persisted for 12 years secondary to blunt trauma when the patient was just four months old. 12 Such a lesion was eventually surgically removed and was histopathologically confirmed to be a chronic hematoma. However, this hematoma differed from the present case in that its formation was within the subcutaneous tissues superficial to the temporoparietal fascia consistent with the published CT findings, and not within the deep temporal space. 12 The deep temporal space lies deep to the temporalis muscle and superficial to the temporal bone of the cranium, extending from the temporal line superiorly to the level of the zygomatic arch inferiorly, where it is confluent with the infratemporal space. It is considered one of the four masticator spaces. In contrast, the superficial temporal space lies superficial to the temporalis muscle but deep to the temporoparietal fascia. There is one other report of an abscess formation from a hypothesized hematoma as a result of aggressive physiotherapy for trismus treatment. However, the evidence for a hematoma, or the conversion of a hematoma to an infected hematoma/abscess was never substantiated (i.e. through imaging) and the exact anatomical location was never completely specified. 13 Therefore, it is to the best knowledge of the authors that this is the first published case of an acute post-traumatic hematoma occurring in the deep temporal space within a pediatric patient.
The sources of bleeding vessels into the deep temporal space in the present case may be due to injury to the deep temporal arteries or the deep temporal veins which lie within this anatomical space. It is possible that a blunt or crush impact caused enough damage to the mentioned vessels leading to hemorrhage into the deep temporal space. Another possible source may be injury to perforator vessels just deep to the temporalis muscle.
Most hematomas, especially if subcutaneous in origin, are self-limiting. Pressure application and ice are acute conservative management options for subcutaneous hematomas smaller than 2 cm. Subcutaneous hematomas that are larger than 2 cm or with continued expansion may be drained with a fine needle or a small incision can be made to induce gravity-dependent drainage. The latter technique is commonly employed to drain auricular hematomas secondary to auricular trauma. 14 Drainage of larger hematomas should be considered to prevent ischemic damage to the surrounding structures. This is well documented with nasal septal hematomas as they require surgical drainage in order to prevent ensuing ischemic damage to the nasal septum. 8,9 Although development of chronic hematomas in the cranio-maxillo facial complex are extremely rare,12 there remains a remote possibility that the hematoma in the presenting case may have become a similarly chronic lesion if there had been no intervention.
Other trauma to the temporal region that have been reported in children include post-traumatic pseudoanuerysms due to injury of the superficial temporal artery. 15,16 Although also a vascular injury, pseudoanureysms are anatomically distinct from hematomas, defined as a collection of blood between the adventitia and muscularis propria of the arterial wall. The CT imaging and clinical presentation in the current case certainly did not support the differential for a pseudoanuerysm. Injuries involving blunt force trauma to the scalp have been shown to produce scalp hematomas, while trauma to the thin temporal bone can produce the much more serious and potentially devastating epidural hematoma. 1,17 Both types of lesions are more frequently associated with skull fractures and traumatic brain injury, especially in children. 17
The development of a facial swelling in a pediatric patient can be due to a myriad of conditions. The differential diagnosis is broad and may include an abscess, vascular malformation, hematoma, or a neoplasm. History and examination are key to narrowing the differential diagnosis and directing appropriate treatment. The recent history of trauma in the presented case along with clinical examination and radiographic evidence favoured a hematoma, albeit situated in an unusual location. If trauma is suspected in a pediatric patient, healthcare workers should be keen on seeking out the source of the trauma, ensuring the reported mechanism fits the pattern of injury. The sudden onset of facial swelling in a pediatric patient can be a cause of great concern for families. Therefore, appropriate and prompt management is critical to the well-being of both the patient and the family.
Declaration of Patient Consent
Full patient consent has been obtained both verbally and in written form via the parents’ permission to publish the case details, photos, and radiographic imaging of the presented case. OH
Oral Health welcomes this original article.
References
- Case ME. Accidental traumatic head injury in infants and young children. Brain Pathol 2008;18:583-589.
- Kalpidis CD, Setayesh RM. Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol 2004;75:631-645.
- Vehmeijer MJ, Verstoep N, Wolff JE, Schulten EA, van den Berg B. Airway Management of a Patient with an Acute Floor of the Mouth Hematoma after Dental Implant Surgery in the Lower Jaw. J Emerg Med 2016;51:721-724.
- Smith MH, Lung KE. Nerve injuries after dental injection: a review of the literature. J Can Dent Assoc 2006;72:559-564.
- Niazi KT, Raja DK, Prakash R, Balaji VR, Manikandan D, Ulaganathan G, et al. Massive expanding hematoma of the chin following blunt trauma. J Pharm Bioallied Sci 2016;8:S182-S184.
- Gassner R, Tuli T, Hachl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg 2003;31:51-61.
- Gupta G, Mahajan K. Nasal Septal Hematoma. StatPearls. Treasure Island (FL), 2018.
- Sayin I, Yazici ZM, Bozkurt E, Kayhan FT. Nasal septal hematoma and abscess in children. J Craniofac Surg 2011;22:e17-19.
- Puricelli MD, Zitsch RP, 3rd. Septal Hematoma Following Nasal Trauma. J Emerg Med 2016;50:121-122.
- Haug RH, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:126-134.
- Gassner R, Tuli T, Hachl O, Moreira R, Ulmer H. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuries in 10 years. J Oral Maxillofac Surg 2004;62:399-407.
- Tada H, Hatoko M, Tanaka A, Yurugi S, Iioka H, Niitsuma K. Chronic expanding hematoma in the temporal region. J Craniofac Surg 2006;17:567-570.
- Gokkulakrishna JJ, V.K. Arora, Ashish Sharma, Anmol, Agarwal. Physiotherapy for Trismus: Caution!!! Heal Talk 2010:33-34.
- Summers A. Managing auricular haematoma to prevent ‘cauliflower ear’. Emerg Nurse 2012;20:28-30.
- Ayling O, Martin A, Roche-Nagle G. Primary repair of a traumatic superficial temporal artery pseudoaneurysm: case report and literature review. Vasc Endovascular Surg 2014;48:346-348.
- Rubio-Palau J, Ferrer-Fuertes A, Garcia-Diez E, Garcia-Linares J, Marti-Pages C, Sieira-Gil R. Traumatic pseudoaneurysm of the superficial temporal artery: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol 2014;117:e112-114.
- Burns EC, Grool AM, Klassen TP, Correll R, Jarvis A, Joubert G, et al. Scalp Hematoma Characteristics Associated With Intracranial Injury in Pediatric Minor Head Injury. Acad Emerg Med 2016;23:576-583.
About the Authors

Johnson Cheung obtained his DDS from the University of Toronto in 2015 and is currently the 3rd-Year Resident at the Oral & Maxillofacial Surgery program at Dalhousie University, Halifax, Nova Scotia.
Corresponding author: johnson.cheung01@gmail.com

Bradley Fisher obtained his DDS from the University of Alberta in 2011 and is currently the Chief Resident of the Oral & Maxillofacial Surgery program at Dalhousie University, Halifax, Nova Scotia. He received his MD and MSc from Dalhousie University in 2018.

Ben Davis received his DDS from the University of Western Ontario in 1992 and his Diploma in Oral and Maxillofacial Surgery and Anesthesia from The University of Toronto in 1997. Following a surgical Fellowship in OMFS at the QE II HSC, he began his academic career at Dalhousie where he is currently Professor in the Department of Oral and Maxillofacial Sciences and its affiliated teaching hospitals. He is also the present Dean of the Faculty of Dentistry at Dalhousie University. He is a past president of the Canadian Association of Oral and Maxillofacial Surgeons and is heavily involved with the Royal College of Dentists of Canada.
RELATED ARTICLE: A Rare Complication of a Retrobulbar Hematoma Formation
Follow the Oral Health Group on Facebook, Instagram, Twitter and LinkedIn for the latest updates on news, clinical articles, practice management and more!












