Introduction:
There can be a lot of flexibility when it comes to workflows and treatment plans for patients with a terminal dentition. These cases are life changing and thus should be well planned and executed. Using a digital workflow can enable proper treatment planning right from the start. These workflows allow restoratively driven implant placement to ensure that the final prosthesis has enough space for material strength and restorative components. The surgery itself can also be planned to be fully guided, ensuring precise placement of the dental implants.
Implant planning begins with the final prosthesis in mind. For patients who need to feel the “snap” of a denture for psychological reasons, implant retained overdentures can be a great prosthesis. It is also a solution that bridges the gap between a regular complete denture and a fixed solution which may exceed the patient’s financial budget. An implant retained overdenture is beneficial when compared to a fixed solution in patients who have minimal interarch space allowance, require maxillary lip support, have a high smile line which would show the prosthetic-tissue junction, or require more latitude in palatal adjustments for phonation purposes.1,2,3 Furthermore, cleaning the prosthesis and the implants are simpler and easier for patients with a removable solution.1
There is much less available literature on maxillary overdentures when compared to mandibular overdentures. Recent systematic reviews have shown that non-splinted maxillary overdentures have a similar survival rate to splinted maxillary overdentures. These designs are associated with high implant and prosthetic survival as well as high patient satisfaction and quality of life.4,5,6
This article presents a method of planning implant surgery for maximum stability and predictability, followed by the restorative procedures of fabricating a maxillary implant retained overdenture.
Treatment Planning Phase:
Treatment planning of a terminal dentition starts by determining where the incisal edge should be located for the final prosthesis.7
Frequently, the occlusal plane of the terminal dentition patient is greatly altered due to tooth wear and tooth movement. Finding the optimal incisal edge based on the face is important to determine where the final prosthesis needs to be, thus determining the position of the dental implants.
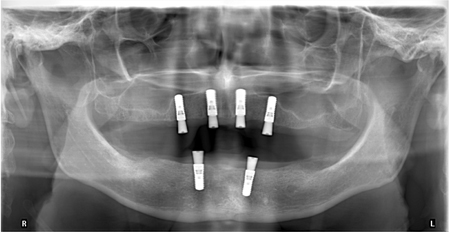
Through digital software (BlueSkyPlan 4; Bluesky Bio), the CBCT file (.DICOM) and the intraoral scan of the patient (.stl) were merged together to plan the implant placement. A minimum of four implants are recommended to ensure a high survival rate for both splinted and unsplinted maxillary overdentures.8 In this case, sufficient bone volume was present, and the implants were paralleled to each other digitally to ensure minimal divergence from a single path of insertion. This allowed for decreased wear on both the overdenture attachments and inserts, as well as increased retention for a longer duration.9,10
With regards to the surgical guide design, the teeth in the implant locations were planned to be extracted first, and then the guide designed to seat on the remaining posterior dentition. This enabled stability of the guide during implant surgery. Planning this involved digital “extractions” of the teeth and flattening of the digital model. Although it has been reported that mucosa and tooth supported guides are both accurate, a tooth supported guide was chosen for ease of use during surgery.11,12 Once the implants were fully placed, the remaining
posterior teeth were then extracted. In this case, four dental implants (4.1x12mm RC Bone Level, Straumann) were submerged to allow for healing and an immediate denture was delivered and relined during the healing period.
Fig. 1

Fig. 2

Fig. 3

Fig. 4
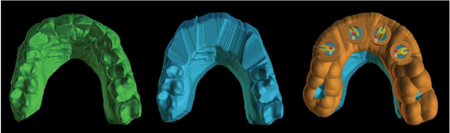
Fig. 5

Fig. 6
Prosthetic Phase
After 4 months of uneventful healing, the implants were uncovered and healing abutments were placed. Four Straumann Novaloc attachments were torqued to manufacturer’s recommendations. Being a removable prosthesis, proper denture principles were followed. This included the use of custom trays, border molding, followed by a final impression with impression copings. The proper border extensions helps support the prosthesis, provide adequate lip support, and prevent future food impaction.
One benefit of placing 4 implants was the ability to reduce palatal coverage on the maxillary prothesis. This improved patient quality of life by increasing their ability to taste as well as allowing them to feel the temperature of what they are consuming.13 Patients with a severe gag reflex also benefit greatly from reduced palatal coverage.14 The disadvantage of a reduced palate is the decreased strength of the prosthesis and the increased risk of fracture.15 This problem was solved using a metal framework which enabled the removal of the palate while providing enough strength to support both the acrylic denture and the teeth. The metal reinforcement also provided increased rigidity to the prosthesis, which helped distribute forces more evenly to the implants and the remaining soft tissue support.16
Fig. 7
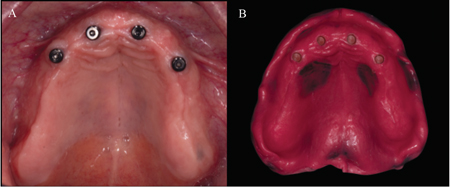
Fig. 8

rim to ensure proper seating and easy retention of the occlusal rims as centric relation at a predetermined vertical dimension is registered.
Fig. 9

Fig. 10

Conclusion:
This case illustrates just one of the ways to plan and execute a removable implant retained maxillary prosthesis. Using digital software combined with traditional techniques, the patient’s needs were be met with a prosthesis which is great yet affordable. Reduced palatal coverage improved the patient’s quality of life, and the removable prosthesis was also easy to clean and maintain.
Oral Health welcomes this original article.
References
- Zitzmann, N. U., & Marinello, C. P. (1999). Treatment plan for restoring the edentulous maxilla with implantsupported restorations: removable overdenture versus fixed partial denture design. The Journal of Prosthetic Dentistry, 82(2), 188–196. https://doi.org/10.1016/S0022-3913(99)70155-1
- Sadowsky, S. J. (2007). Treatment considerations for maxillary implant overdentures: A systematic review. Journal of Prosthetic Dentistry, 97(6), 340–348. https://doi.org/10.1016/S0022-3913(07)60022-5
- Sadowsky, S., & Zitzmann, N. (2017). Protocols for the Maxillary Implant Overdenture: A Systematic Review. The International Journal of Oral & Maxillofacial Implants, 31, s182–s191. https://doi.org/10.11607/jomi.16suppl.g5.2
- Wang, F., Monje, A., Huang, W., Zhang, Z., Wang, G., & Wu, Y. (2016). Maxillary Four Implant-retained Overdentures via Locator® Attachment: Intermediate-term Results from a Retrospective Study. Clinical Implant Dentistry and Related Research, 18(3), 571–579. https://doi.org/10.1111/cid.12335
- Anadioti, E., Gates, W. D., Elpers, J., De Kok, I. J., & Cooper, L. F. (2019). Retrospective cohort analysis of maxillary overdentures retained by unsplinted implants. Journal of Prosthetic Dentistry, 122(3), 301-308.e1. https://doi.org/10.1016/j.prosdent.2018.10.014
- Di Francesco, F., De Marco, G., Gironi Carnevale, U. A., Lanza, M., & Lanza, A. (2019). The number of implants required to support a maxillary overdenture: a systematic review and meta-analysis. Journal of Prosthodontic Research, 63(1), 15–24. https://doi.org/10.1016/j.jpor.2018.08.006
- Spear F. (1999). The maxillary central incisal edge: a key to esthetic and functional treatment planning. Compendium of continuing education in dentistry (Jamesburg, N.J. : 1995), 20(6), 512–516.
- Di Francesco, F., De Marco, G., Sommella, A., & Lanza, A. (2019). Splinting vs Not Splinting Four Implants Supporting a Maxillary Overdenture: A Systematic Review. The International Journal of Prosthodontics, 32(6), 509–518. https://doi.org/10.11607/ijp.6333
- Al-Ghafli, S. A., Michalakis, K. X., Hirayama, H., & Kang, K. (2009). The in Vitro Effect of Different Implant Angulations and Cyclic Dislodgement on the Retentive Properties of an Overdenture Attachment System. Journal of Prosthetic Dentistry, 102(3), 140–147. https://doi.org/10.1016/S0022-3913(09)60134-7
- Teimoori, H., Shayegh, S. S., Zavaree, M. A., Hakimaneh, S. M. R., Khodadad, F., Shidfar, S., & Baghani, M. T. (2018). Effects of excessive implant angulation on retention of two types of overdenture attachments during cyclic loading. Journal of Contemporary
- Dental Practice, 19(10), 1221–1227. https://doi.org/10.5005/jp-journals-10024-2408
- Raico Gallardo, Y. N., da Silva-Olivio, I. R. T., Mukai, E., Morimoto, S., Sesma, N., & Cordaro, L. (2017). Accuracy comparison of guided surgery for dental implants according to the tissue of support: a systematic review and meta-analysis. Clinical Oral Implants Research, 28(5), 602–612. https://doi.org/10.1111/clr.12841
- Gerhardt, M. N., Kreuzer, K. B., & Shinkai, R. S. A. (2021). Literature on the accuracy of guided surgery for dental implants: A scoping review. Journal of Osseointegration, 13(3), 127–137. https://doi.org/10.23805/JO.2021.13.03.5
- da Silva, R. O. C., Lacerda, W. F., Henn, I. W., Chaiben, C. L., Machado, M. Â. N., & de Lima, A. A. S. (2021). Relationship between taste perception and use of upper complete dentures. Special Care in Dentistry, 41(2), 244–250. https://doi.org/10.1111/scd.12559
- Farmer, J. B., & Connelly, M. E. (1984). Palateless dentures: Help for the gagging patient. The Journal of Prosthetic Dentistry, 52(5), 691–694. https://doi.org/10.1016/0022-3913(84)90143-4
- Simões, I. Í. N., Spyrides, S. M. M., Schanuel, F. R. da S., & De Mello, E. B. (2017). Estudo comparativo de sobredentaduras implantorretidas esplintadas e não-esplintadas sem cobertura palatal: Uma revisão de literatura. Brazilian Dental Science, 20(4), 32–41. https://doi.org/10.14295/bds.2017.v20i4.1482
- Takahashi, T., Gonda, T., & Maeda, Y. (2016). Effects of Reinforcement on Denture Strain in Maxillary Implant Overdentures: An In Vitro Study Under Various Implant Configurations. The International Journal of Oral & Maxillofacial Implants, 31(6), e162–e167. https://doi.org/10.11607/jomi.4711
About the Author
 Max Li is a board-certified prosthodontist and a fellow of the RCDC. He received his dental degree from the University of Toronto and his specialization from the University of Manitoba. He currently maintains a full-time specialty practice in Toronto and teaches as a clinical instructor at the University of Toronto Faculty of Dentistry.
Max Li is a board-certified prosthodontist and a fellow of the RCDC. He received his dental degree from the University of Toronto and his specialization from the University of Manitoba. He currently maintains a full-time specialty practice in Toronto and teaches as a clinical instructor at the University of Toronto Faculty of Dentistry.













