According to the CDC, “47.2% of adults aged 30 years and older have some form of periodontal disease. Periodontal disease increases with age, 70.1% of adults 65 years and older have periodontal disease.”1 The numbers of adults with untreated periodontal disease are high.
The dental hygienist is front line defense in the office for periodontal disease. She or he is the first to see the patient, evaluate the periodontal status then be closely involved with treatment. Directly treating the patient, the dental hygienist is able to educate about the sequellae of periodontal disease, instruct in proper home care and actively have an important role in direct patient care.
Periodontal disease is both an inflammatory and infectious disease. Bacteria inhabit the biofilm, and the resultant infection will cause an inflammatory reaction. The local inflammatory reaction is the primary driver of the disease, which will activate the innate immune system response. Failure to encapsulate or control the inflammation within the gingival tissues will result in the expansion of the response into the bone, causing the destruction of connective tissue and alveolar bone. In periodontal disease, the inflammatory response is not effective in resolving the lesion but actually perpetuating it. We need to control both the infection and the inflammation for periodontal health.2,3,4
Traditional non-surgical treatments of scaling and root planning as well as mechanical removal of plaque are historically delegated to the hygienist. Antibacterials were added to treatment regimens during the mid-seventies, and have been added to the standard periodontal treatment arsenal.5,6 In the nineties, sustained release delivery of antimicrobials, such as PerioChip® and Arrestin®, were added to non-invasive periodontal treatment.7,8,9 We are now looking into host modulation10 used in conjunction with the other therapies available.11,12 The additional antimicrobial, anti-inflammatory and tissue rebuilding patches are easily incorporated into the traditional treatment.12,13 Focusing on the on the host aspect of periodontal disease, these modulation therapies work to decrease or inhibit the destructive effects of the host response and increase more protective, healing aspects, allowing the immune inflammatory reaction to bacterial plaque to be less damaging to the tissues.14 Please see Figure 1.
Figure 1
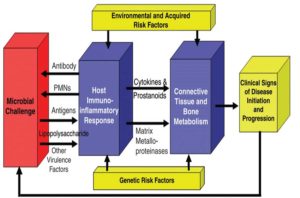
Periodontal Disease Model (Kornman, K. J Periodontol • August 2008)14
Working with the model of host modulation and increasing the healing components of the inflammatory response is a proactive method of treating periodontal disease. Dental hygienists are able to expand their functions to utilize a novel non-invasive treatment, along with their traditional scaling and root planning procedures, which provides anti-inflammatory, tissue rebuilding and antibacterial therapy. PerioPatch™ is a wound healing patch that contains high dose, focused delivery of bioactives derived from plants.15 The indication for these unique healing patches are for acute or highly inflamed sites, post scaling and root planing, recession and a myriad of other therapeutic needs. PerioPatch™ reduces inflammation and promotes healing. This patch uniquely absorbs exudate from the gingiva and crevicular fluid to aid in healing. Used with PeriActive™ rinse, there is an additive effect of anti-inflammatory, antibacterial and promoting tissue healing. Please see Table 1 and Figures 2 and 3.
Table 1: PeriActive™ and PerioPatch™ Uses
PERIACTIVE AND PERIOPATCH MAY BE USED
• Adjunctive to Scaling and Root Planing
• Early stage recession
• Adjunctive to surgical treatment and extractions
• Treat and prevent peri-implantitis
• Oral wounds
• Intraoral chemical burns
• Traumatic ulcers or abrasions
• Cheek bites
• Denture sores
• Every day rinse for gingivitis and periodontal patients
Figure 2
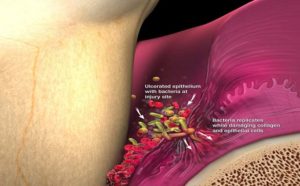
Periodontal pocket with ulcerated epithelium and bacteria attacking the collagen
Figure 3

Scaling and curettage cleaning the infected pocket
PerioPatch™ contains extracts of three optimized botanicals (Centella asiatica, Echinacea purpurea and Sambucus nigra), all found to be clinically effective in reducing inflammation and prohealing. Studies have shown Centella increases collagen production. Centella exhibits anti-bacterial activity in addition to reducing the glucoronidase, which has been associated with gingival inflammation. Both Sambucus and Echinacea exhibit anti-inflammatory and anti-bacterial effects.16,17
After scaling and root planing an affected site, placement of this topical healing PerioPatch™ will draw out the inflammatory exudate and help tissue regeneration by facilitating the deposition of collagen in the wound area.18 The patch is a hydrogel, which has been utilized in wound healing in medicine. It is a novel approach in dentistry, applying bioactives directly to the tissue. Unlike locally applied antibiotics, this patch sits on the outer aspect of the gingival tissue and draws out inflammatory exudate while acting as a barrier.19 The dental hygienist or dentist will place the initial patch (Figure 4). The patch remains in place for approximately fifteen to sixty minutes, and then the outer cellulose backing will fall off. The hydrogel can remain on the tissue for up to five hours, but is usually no more than sixty minutes. Depending on the clinical extent of treatment, multiple patches may be placed. While placing the patch, it is helpful for the patient to observe. The patient will then apply one more patches on the first day and two patches for the next three days on the affected areas. It is important to instruct the patient they should not eat or drink during this time the patch is in place to maximize the effectiveness of the hydrogel. In conjunction with the PerioPatch™, the use of a botanical, non-alcohol rinse of PeriActive™ will further decrease inflammation, decrease plaque and improve healing to the area.
Figure 4

Adhering the PerioPatch™ to affected area
Figure 4B

Inflammation is drawn to the patch while immune cells are brought into the infected area
The hydrogel serves several purposes: it will protect and cover the pocket to prevent any further irritation, while absorbing the excess inflammatory fluid. This will result in a decrease in clinical inflammation20 and an increase in collagen and fibroblast deposition, allowing for better healing of the area. Focusing on delivering direct bioactives that will assist in healing and reducing inflammation, along with a diligent effort by the patient with oral home care, the reduction in pocket depths are apparent.
PerioPatch™ not only helps draw out exudate and reduce inflammation but will enhance the gingiva to repair (Figures 5, 6, 7 & 8). The average volume of gingival crevicular fluid in a healthy individual is 3µL. For a patient with moderate periodontal disease, the fluid volume is 20 µL. Patients with advanced periodontal disease have fluid levels of 44µL PerioPatch™ can absorb up to 140µL within an hour. The patch gives the patient immediate relief while accelerating healing and protecting the site. This reparative function is key in helping our patients with their periodontal issues. Drawing out the pro-inflammatory fluid from the gingival and sulcus will rebalance the tissues by assisting the natural healing and tissue repair.20 The favorable reduction in pocket depths, improvement in bleeding upon probing, along with the increase in clinical attachment gains have been demonstrated (Figures 9 & 10).21,22
Figure 5
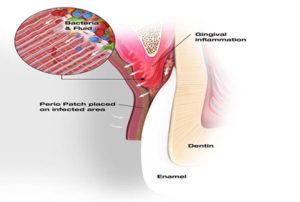
Bacteria and inflammatory fluid are drawn to the PerioPatch™
Figure 6
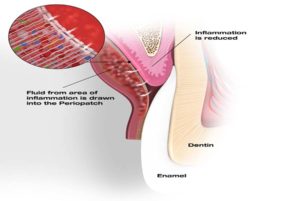
Inflammation is reduced and healing fibroblast cells are depositing collagen
Figure 7

Healing cells close the ulceration and fibroblast cells deposit collagen
Figure 8
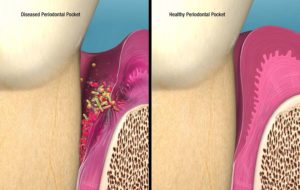
Infected pocket vs. Healthy pocket post treatment
Figure 9

Mean PD Reduction and CAL Gains at 4-6 Weeks above SRP with PerioPatch™ versus Approved Adjunctive Antimicrobials22
Figure 10
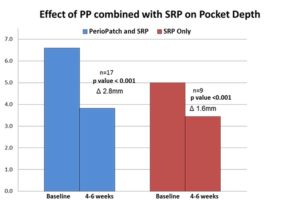
Combined effect of utilizing both PerioPatch™ hydrogel and PeriActive rinse on reducing pocket depths 22
Figure 11

Pretreatment
Figure 12

Pretreatment
Figure 13

Patch in place
Figure 14

One-day post-op
Figure 15

One-year post-op
Figure 16

Pretreatment
Figure 17

Pretreatment
Figure 18

Patch in place
Figure 19

Post treatment one-month
Figure 20

Post treatment three months
References
1. https://www.cdc.gov/oralhealth/periodontal_disease/ Accessed March 2, 2017
2. Teles, R., Teles, F., Frias-Lopez, J., Paster, B., Haffajee, A. Lessons learned and unlearned in periodontal microbiology. Periodontol 2000. 2013 Jun; 62(1): 95–162.
3. Cochran, DL. Inflammation and Bone Loss in Periodontal Disease. Journal of Periodontology August 2008, Vol. 79, No. 8s, Pages 1569-1576,
4. Brasswell, Laura D. Targeting the host Dentistry Today http://www.dentistryiq.com/articles/wdj/print/volume-2/issue-2/focus-on-perio/targeting-the-host.html
5. Slots J, Ting M. Systemic antibiotics in the treatment of periodontal disease. Periodontology 2000. 2002;28:106–176.
6. Beliveau, D, et al. Benefits of Early Systemic Antibiotics in Localized Aggressive Periodontitis. A Retrospective Study J Clin Periodontol. 2012 Nov; 39(11): 1075–1081.
7. Friedman M, Steinberg D. Sustained-release delivery systems for treatment of dental diseases. Pharm Res. 1990 Apr;7(4):313-7
8. Williams RC, Paquette DW, Offenbacher S, et al. Treatment of periodontitis by local administration of minocycline microspheres: a controlled trial. J Periodontol 2001;72:1535-1544.
9. Jeffcoat MK, Palcanis KG, Weatherford TW, Reese M, Geurs NC, Flashner M. Use of a biodegradable chlorhexidine chip in the treatment of adult periodontitis: clinical and radiographic findings. J Periodontol 2000;71:256-62.
10. Golub LM, et al. Modulation of the host response in the treatment of periodontitis. Dentistry Today 1998; 17(10):102-109.
11. Paquette DW, Levine WZ. Adjunctive Treatment of Periodontal Disease with Self-Adhesive Hydrogel Wound Dressing: Case Series. Compend Contin Educ Dent. 2015 Jun;36(6): e12-4.
12. Levine WZ, Samuels N, Eliya- Barsheshet MM, Grbic JT. A Novel Treatment of Gingival Recession using a Botanical Topical Gingival Patch and Mouthrinse. J Contemp Dent Pract 2013;14(5):948-953.
13. Samuels N, Saffer A, Wexler ID, Oberbaum M. Localized Reduction of Gingival Inflammation Using Site-specific Therapy with a Topical Gingival Patch. J Clin Dent 2012;23:64–67
14. Korman, K. Mapping the Pathogenesis of Periodontitis: A New Look Journal of Periodontology August 2008, Vol. 79, No. 8s, Pages 1560-1568
15. Paquette, ibid
16. Punturee K, Wild CP, Kasinrerk W, Vinitketkumnuen U. Immunomodulatory activities of Centella asiatica and Rhinacanthus nasutus extracts. Asian Pac J Cancer Prev. 2005;6(3):396400.
17. Mishima S, Saito K, Maruyama H, et al. Antioxidant and immunoenhancing effects of Echinacea purpurea. Biol Pharm Bull. 2004;27(7):10041009.
18. Nemcovsky, Carlos E. A novel device to enhance soft tissue healing: Clinical applications of PeriZone PerioPatchTM in a variety of cases. Dental Products Report September 2012
19. Saffer, A., Samuels, N. A Novel Adjuvant Treatment to Scaling and Root Planing With a Topical Gingival Patch: A Case Series. Clinical Advances in Periodontics. August 2012, Vol. 2, No. 3, Pages 123-127
20. Smiley CJ, Tracy SL, Abt E, et al. Evidence-based clinical practice guideline on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc 2015;146:525-35.
21. Saffer, ibid
22. Paquette, ibid
23. Levine, ibid
 Sheri B. Dongier is a leading dental clinician, author, international educator, and consultant who currently practices dentistry in Lincolnwood, IL. Dr. Doniger is an avid researcher, frequently contributing to an array of dental publications on a variety of topics. She is a member of the IZUN Oral Healthcare Scientific Advisory Team. Please free to contact Dr. Doniger at www.donigerdental.com. Clinical photos courtesy of Dr. William Z. Levine.
Sheri B. Dongier is a leading dental clinician, author, international educator, and consultant who currently practices dentistry in Lincolnwood, IL. Dr. Doniger is an avid researcher, frequently contributing to an array of dental publications on a variety of topics. She is a member of the IZUN Oral Healthcare Scientific Advisory Team. Please free to contact Dr. Doniger at www.donigerdental.com. Clinical photos courtesy of Dr. William Z. Levine.












