
Failed mandibular anaesthesia is a burden on both patients and dental practitioners, as lack of profound anaesthesia can result in pain, apprehension about dental visits, and rescheduling of appointments. When considering factors such as the provider, patient, and techniques used, the incidence of failed mandibular anaesthesia has been reported to be as high as 50%.1
Normal mandibular anatomy
The inferior alveolar nerve arises from cranial nerve V3, which is one of the divisions of the trigeminal nerve. It follows a close relationship with the medial side of the mandibular ramus before entering the mandibular canal at the level of the lingula. The inferior alveolar nerve provides sensory innervation to the mandibular teeth.
The inferior alveolar nerve divides into the incisive nerve and the mental nerve in the mandibular premolar region. The mental nerve exits the canal via the mental foramen and provides sensory innervation to the mandibular buccal gingiva and lips. In most cases, the mental foramen is located apically between the first and second premolars or below the second premolar.2 The incisive nerve remains inside the mandibular canal and provides sensory innervation to teeth anterior to the mental foramen.
Fig. 1

Causes of failed mandibular anaesthesia
Mandibular injections first began in the 1880s, when William Stewart Halsted used cocaine to attempt the inferior alveolar nerve block on himself and his colleagues.4 It is important to note that these mandibular anaesthetic techniques were initially derived from the anatomy of Caucasian males.4 Numerous variations of normal anatomy due to ethnicity and gender may deviate from what was studied previously, and can have profound effects on the success of local anaesthesia injections.5 Anatomical variations reported in the literature include bifid mandibular canals, mandibular canal position, and ramus flare.6 Other contributors are patient anxiety, infection, and high metabolism.7 Dr. Waters provided a detailed review and strategies addressing these concerns in his 2020 Oral Health Group article.8
Beyond the physiological processes that affect the inferior alveolar nerve, supplemental innervation to mandibular teeth from other nerves must also be considered. There are three hypotheses of anatomical nerve variations which may contribute to failed mandibular anaesthesia.
- Cross-innervation of contralateral nerves
- Accessory innervation from the superficial cervical plexus
- Accessory innervation from the mylohyoid nerve (nerve to mylohyoid)
Cross-innervation
The hypothesis of cross-innervation from the contralateral inferior alveolar nerve has been evaluated in both patient and cadaver specimens. A study by Yonchak et al. randomized 38 subjects to receive a unilateral or bilateral inferior alveolar nerve blocks at two separate appointments.9 Each block used 3.6 mL of 2% lidocaine with 1:100,000 epinephrine. All subjects had lip numbness indicating successful inferior alveolar nerve anesthesia. From the unilateral blocks, only 39% of the central incisors, 50% of the lateral incisors, and 68% of the canines had successful anesthesia. For the bilateral blocks, 66% of the central incisors, 74% of the lateral incisors, and 76% of the canines had successful anesthesia. Since the bilateral blocks had improved anesthesia success, there is likely presence of mandibular cross-innervation. There was also a trend of increasing success rates with posterior teeth, likely due to decreasing cross branches when moving posteriorly. Since the bilateral blocks did not produce 100% successful anesthesia, there may be possible additional anastomoses of other nerves that innervate these teeth.
To increase the success rate of mandibular anesthesia of anterior teeth, bilateral incisive nerve blocks could be used routinely.
Cervical plexus innervation
The cervical plexus is a group of motor and sensory nerves originating from the anterior rami of cervical nerves C1 to C4. This plexus contains eight branches, two of which have been postulated to provide accessory innervation to the mandibular teeth. The transverse cervical nerve contains branches of C2 and C3 and provides sensory innervation to the lateral and anterior regions of the neck. The great auricular nerve also arises from branches of C2 and C3 and provides sensory innervation to skin in area of the parotid gland, auricle, and mastoid process.
Fig. 2

A study by Ella et al. evaluated the distribution of the transverse cervical and great auricular nerves by dissecting both halves of 250 fresh human cadaver heads.11 They found that 99.2% of great auricular nerves and 40% of transverse cervical nerves had contact with the mandible.
To confirm the true relationship of the cervical plexus innervating the mandibular teeth, Bitner et al. evaluated the success of anesthetizing these nerves in the mandible.12 They evaluated 40 patients diagnosed with symptomatic irreversible pulpitis who received a failed inferior alveolar nerve block confirmed by profound lip numbness. Patients either received 2 mL of 2% lidocaine 1:100,000 epinephrine or saline via the intraoral cervical plexus technique. The intraoral cervical plexus block was completed by placing a short needle through the vestibular area of the buccal mucosa below the roots of the teeth at a 45-degree angle, in direct contact with bone. In the cervical plexus block group 60% of subjects showed successful anesthesia versus none in the saline group.
These findings support the use of local buccal infiltration of mandibular teeth if there is inadequate anesthesia resulting from a correctly positioned inferior alveolar nerve block.
Fig. 3

Mylohyoid innervation
The mylohyoid nerve is a branch of cranial nerve V3 that splits from the inferior alveolar nerve prior to entry into mandibular foramen. It courses medially to the mandibular body and lies in the floor of the mouth. This nerve provides motor supply to the mylohyoid muscle and anterior belly of the digastric. An early study completed in 1972 by Frommer et al. concluded that 20% of nerve fibers from mylohyoid fit description of pain fibers, supporting the possibility of sensory innervation to the mandibular teeth.13
Fig. 4
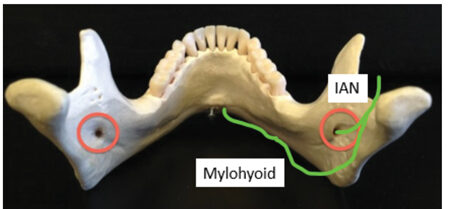
A study completed by Wilson et al. evaluated the branching point of the mylohyoid nerve from the inferior alveolar nerve in 37 adult human cadavers.15 They found that the mean branching distance from the mandibular canal was 14.7 mm, higher than the usual level (10 mm) advised in the standard inferior alveolar nerve block technique. They also found that the nerve may be shielded from local anesthetic solution by the sphenomandibular ligament. In addition, there was a 43% incidence of extension of the mylohyoid nerve to foramina on the lingual aspect of the mandible and this extension occasionally joined the contralateral incisive nerve. Therefore, the mylohyoid nerve may provide both accessory and contralateral innervation to the mandibular teeth. The standard mandibular block may fail to anesthetize this nerve due to inferior landmark positioning and anatomical interference.
Several injection methods have been postulated to overcome the accessory innervation of the mandibular teeth from the mylohyoid nerve. A commonly used technique is to administer local anesthesia distal to the lingual aspect of the tooth.16 This injection should remain superficial and not exceed a depth of 2–3 mm below the mucosa. The needle tip should also remain close to mandible to avoid more medial structures such as Wharton’s duct and the lingual artery.
Fig. 5

Another mandibular nerve block technique that successfully anesthetizes the mylohyoid nerve is the Gow-Gates block. This injection technique involves approaching the neck of the condyle from the contralateral premolars. This way, the needle insertion point is higher and may anesthetize the inferior alveolar nerve prior to branching of the mylohyoid nerve. Some studies suggest a 95%+ success rate of mandibular anesthesia with proper Gow-Gates technique, likely due to anesthesia of these accessory nerve fibers.17
Fig. 6

A review article by Sutton states that the mylohyoid nerve fibers innervating mandibular anterior teeth can be anesthetized by inserting the needle near the inferior retromental foramen (inferior to genial tubercles) via extra-oral approach.16 There is no other literature evaluating the efficacy of this method.
Conclusion
The high incidence of failed mandibular anesthesia may be due to anatomical variations of nerves. Cross-innervation of contralateral nerves can be addressed with bilateral nerve blocks. Accessory innervation from the superficial cervical plexus may be successfully countered by using an intraoral cervical plexus block, on the buccal aspect of the mandible. Accessory innervation from the mylohyoid nerve can be addressed by using a Gow-Gates block, lingual infiltration, or an extraoral infiltration near the inferior retromental foramen. If these methods fail, one could consider the use of supplemental intraligamentary or intraosseous injections. These suggestions are summarized in Table 1.
Table 1
| Aberrant nerve pathway | Mandibular teeth innervated | Injection technique | Supplemental injection |
| Cross-innervation | Teeth anterior to mental foramen | Bilateral incisive nerve blocks | |
| Superficial cervical plexus | Posterior teeth | Local buccal infiltration | |
| Mylohyoid nerve | Posterior and anterior teeth | Local lingual infiltration Gow-Gates block Extraoral inferior retromental foramen injection | Intraligamentary injection Intraosseous injection |
Oral Health welcomes this original article.
References
- Mikesell, P., Nusstein, J., Reader, A., Beck, M., & Weaver, J. (2005). A comparison of articaine and lidocaine for inferior alveolar nerve blocks. Journal of endodontics, 31(4), 265–270. https://doi-org.myaccess.library.utoronto.ca/10.1097/01.don.0000140576.36513.cb
- Pelé, A., Berry, P. A., Evanno, C., & Jordana, F. (2021). Evaluation of Mental Foramen with Cone Beam Computed Tomography: A Systematic Review of Literature. Radiology research and practice, 2021, 8897275. https://doi.org/10.1155/2021/8897275
- Innervation of the dentition. (2014, January 26). Wikimedia Commons. https://commons.wikimedia.org/wiki/File:Innervation_of_the_dentition.png
- Matas R. (1952). The story of the discovery of dental anesthesia by nerve blocking; achievements of
William Stewart Halsted. Surgery, 32(3), 530–537. - Shalini, R., RaviVarman, C., Manoranjitham, R., & Veeramuthu, M. (2016). Morphometric study on mandibular foramen and incidence of accessory mandibular foramen in mandibles of south Indian population and its clinical implications in inferior alveolar nerve block. Anatomy & cell biology, 49(4), 241–248. https://doi.org/10.5115/acb.2016.49.4.241
- Wolf, K. T., Brokaw, E. J., Bell, A., & Joy, A. (2016). Variant Inferior Alveolar Nerves and Implications for Local Anesthesia. Anesthesia progress, 63(2), 84–90. https://doi.org/10.2344/0003-3006-63.2.84
- Potocnik, I., & Bajrovic´ , F. (1999). Failure of inferior alveolar nerve block in endodontics. Endodontics & dental traumatology, 15(6), 247–251. https://doi.org/10.1111/j.1600-9657.1999.tb00782.x
- Waters, B. (2020, February). Mandibular Anesthesia: Troubleshooting and Overcoming Failure to Anesthetize. Oral Health Group. https://www.oralhealthgroup.com/features/mandibular-anesthesia-troubleshooting-and-overcoming-failure-to-anesthetize/
- Yonchak, T., Reader, A., Beck, M., & Meyers, W. J. (2001). Anesthetic efficacy of unilateral and bilateral inferior alveolar nerve blocks to determine cross innervation in anterior teeth. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics, 92(2), 132–135. https://doi-org.myaccess.library.utoronto.ca/10.1067/moe.2001.115720
- Saripalli, R., Kasaraneni, S., Yadavilli, S. S., & Alluri, L. (2022). Superficial Cervical Plexus Block in Selective Cases of Oral and Maxillofacial Surgery as an Alternative to General Anesthesia: A Case Presentation. Cureus, 14(1), e21371. https://doi.org/10.7759/cureus.21371
- Ella, B., Langbour, N., Caix, P., Midy, D., Deliac, P., & Burbaud, P. (2015). Transverse cervical and great auricular nerve distribution in the mandibular area: a study in human cadavers. Clinical anatomy (New York, N.Y.), 28(1), 109–117. https://doi-org.myaccess.library.utoronto.ca/10.1002/ca.22369
- Bitner, D. P., Uzbelger Feldman, D., Axx, K., & Albandar, J. M. (2015). Description and evaluation of an intraoral cervical plexus anesthetic technique. Clinical anatomy (New York, N.Y.), 28(5), 608–613. https://doi-org.myaccess.library.utoronto.ca/10.1002/ca.22543
- Frommer J, Mele FA, Monroe CW. (1972). The possible role of the mylohyoid nerve in mandibular posterior tooth sensation. J Am Dent Assoc 85:113–117
- Mandibular foramina. (2012, February). Wikimedia Commons. https://commons.wikimedia.org/wiki/File:Mandibular_foramina.jpg
- Wilson, S., Johns, P., & Fuller, P. M. (1984). The inferior alveolar and mylohyoid nerves: an anatomic study and relationship to local anesthesia of the anterior mandibular teeth. Journal of the American Dental Association (1939), 108(3), 350–352. https://doi-org.myaccess.library.utoronto.ca/10.14219/jada.archive.1984.0005
- Sutton R. N. (1974). The practical significance of mandibular accessory foramina. Australian dental journal, 19(3), 167–173. https://doi-org.myaccess.library.utoronto.ca/10.1111/j.1834-7819.1974.tb05034.x
- Haghighat, A., Jafari, Z., Hasheminia, D., Samandari, M. H., Safarian, V., & Davoudi, A. (2015). Comparison of success rate and onset time of two different anesthesia techniques. Medicina oral, patologia oral y cirugia bucal, 20(4), e459–e463. https://doi.org/10.4317/medoral.20526
- Base of mandible–close up–anterolateral view. (2014, July 21). Wikimedia Commons. https://commons.wikimedia.org/wiki/File:Base_of_mandible_-close_up-_anterolateral_view01.png
About the Author

Lucia Santos is a current second-year dental anesthesiology resident at the University of Toronto, where she had previously completed her Doctor of Dental Surgery degree. She is also conducting research at the Hospital for Sick Children (SickKids) where she focuses on neonatal pain management. She can be reached at lucia.santos@mail.utoronto.ca.












