Background information:
The use of dental implants in the rehabilitation of partially edentulous and completely edentulous patients has been available for many years. The benefits of dental implants in improving the quality of life for these patients have been well documented. The replacement of missing teeth can take the form of both the fixed and the removable solutions. In the partially edentulous patients, the use of dental implants for the removable option is often referred to as an implant supported removable partial denture. Other names may include implant assisted removable partial denture, implant supported removable dental prosthesis or the implant-tissue – supported removable partial denture. These solutions offer an additional treatment options to partial edentulous patients whose remaining dentition may not have the adequate abutments for the conventional fixed and/ or the conventional removable prosthodontic treatment. The use of dental implants in these situations can also offer many benefits. This article aims to highlight some important concepts when designing and treatment planning for these implant supported removable partial dentures.
The Benefits of Treatment:
In evaluating several treatment options for the partially edentulous patients, one must remember the traditional options such as the fixed reconstruction using dental implants, or the traditional cast removable partial denture option. Both treatment options have been acceptable solutions for the partially edentulous patients. For the fixed reconstructions using dental implants, the number and the location of dental implants are important to the overall aesthetic and the functional outcome. However, if these cases lack the available soft and hard tissue, the additional need for invasive surgical procedures for the ridge augmentation may complicate the treatment plan. As for the use of a cast removable partial denture, these cases require the appropriate number and the proper distribution of abutments along with a proper design to be successful. In cases with long edentulous spans, severe ridge resorption, and inadequate number and the distribution of appropriate abutments, the use of dental implants in these cases can offer a more cost effective, less invasive solutions than either the fixed implant reconstruction or a traditional cast removable partial denture. The use of dental implants in these cases can provide additional support and retention as well as improving the aesthetic outcome of the case.
Three different clinical cases will be used to illustrate how dental implants can be used to rehabilitate the various partially edentulous cases to improve the support, the retention and the aesthetic using implant supported removable solutions.
Case 1
The first case is an 89 year old patient with the chief concern that her existing partial denture is loose. The patient recently lost an abutment tooth 34 that was previously supporting her mandibular cast partial denture. The denture was repaired with a tooth addition but there was no retentive element on the lower left side. When she presented to me, she was unhappy with her partial denture.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
Fig. 8
Planning Consideration
On examination, her remaining mandibular teeth are stable. However, she has a pier abutment 45 which complicates the development of a standard cast RPD with the introduction of many fulcrum points. While the tooth was still periodontally sound, the decision was made to extract 45 and plan for two dental implants to help support and to retain a lower cast partial denture. Mechanically, the location of dental implants would be best to be in the location of the molar areas. However, anatomically, due to the lack of available bone height and bone width, the decision was to place two dental implants distal to the remaining natural teeth. The advantage of this implant supported partial design would be the elimination of unaesthetic metallic clasps on the remaining mandibular teeth and to minimize the unfavourable forces that may be placed on a classic Kennedy class I RPD design. The use of a lingual apron can serve to offer some indirect retention and bracing stability. In addition to this mechanical and aesthetic advantage, should the remaining mandibular teeth deteriorate, the conversion of an implant supported overdenture can be easily facilitated by this design.
Case 2
In this second case, when the patient was presented to me, he already had dental implants placed for some of his missing teeth. The surgical treatment took a lot longer than expected. In the meantime, his dentition was becoming more and more unstable with fracturing more teeth resulting in the need to address more missing teeth and the need to modify his existing treatment plan. The cost of the treatment has increased to the point that it became unmanageable for the patient if he continued to plan for a fixed reconstruction using dental implants. The treatment plan discussion began to shift from a fixed reconstruction to a concept of implant supported partial denture as a solution to address his unstable dentition as well as the replacement of his multiple missing teeth. In the end, with the strategic use of some surveyed crowns and the already placed dental implants as implant abutment, the implant supported partial dentures behave much like a tooth supported removable partial denture with greater stability and retention. This is a classic example of converting a tooth and tissue supported type of partial denture design to a more tooth supported partial denture design. The use of implant abutments also eliminated the need for clasps placement on anterior teeth improving the overall aesthetic outcome of the case. The remaining framework also offer additional stabilization to some of the compromised teeth. In this case, the shift from a fixed solution to an implant supported removable partial allowed a cost effective method to restore function and aesthetic in this patient with multiple edentulous spans.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig 6
Fig. 7
Fig. 8
Fig. 9
Fig. 10
Fig. 11
Fig. 12
Case 3
This last case represents a common scenario from patients in the geriatric population. Treatment planning in this population has to factor into account the general health condition and functional limitations as well as the patient’s socio-economic context. Often times, the solutions represent the non standard approach to rehabilitation due to the deteriorating physical, cognitive and dental condition. The use of dental implants in a removable partial solution can be adapted to many dental condition as a way to provide additional support, retention and a method of future transition should the remaining dentition deteriorate. In this case, the patient’s cognitive awareness was deteriorating. The decision was to keep everything as simple as possible while providing some functional and aesthetic improvement.
The case can easily be approached with full fixed implant reconstruction for the maxilla. Or considering full maxillary clearance and to replace the missing teeth with a conventional denture or any implant supported removable solutions. Instead, the decision was to keep the remaining teeth and to have some dental implants as abutments for a tooth and implant supported partial overdenture. This treatment allows the patient to maintain his current posterior support as well as improving the retention, support and aesthetic of his maxillary arch. Should any of the maxillary teeth become symptomatic, the prosthesis can be easily modified for future addition or a conversion to a full arch prosthesis. This approach will keep most of the dental treatment as conservative as possible while at the same time allows flexibility to convert the prosthesis into other prosthetic solutions when needed.
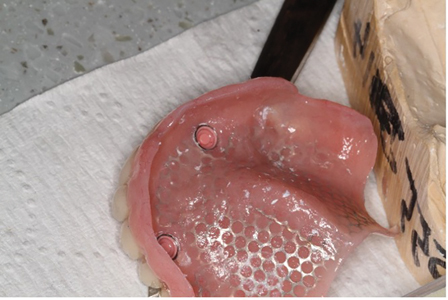
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Treatment Planning
In planning for an implant supported removable partial dentures, there are some additional considerations that are important for both the surgical and prosthetic planning.
1/ Path of Insertion During Pre-surgical planning
Whenever possible, planning ahead the proposed path of insertion for the partial denture would be helpful. If anatomically feasible, the dental implants should be placed along the same path of insertion. By doing so, there will be more prosthetic options to ensure the implant supported partial denture will work favourably with the implants.
2/The Location Of Dental Implants Should Be Planned Based On Anatomic And Opposing Occlusal Factors.
The decision of where to place the dental implant can be influenced by the available bone. However, the available interocclusal space and the type of occlusal factors are also important consideration during the planning phase. Interocclusal space evaluation should factor in the prosthetic space required for accommodating the housing and the abutment attachments. For the more common attachments such as the locators, the required space from the occlusal plane to the crestal aspect of the dental implant should be at least 8 to 8.5mm.
In addition, the opposing occlusal plane and occlusal forces should be analyzed carefully along with the possible fulcrum lines of the RPD design. If planned strategically, the location of the dental implant can improve the denture support and can minimize denture movement.
3/Framework design consideration
In designing the framework for the partial denture, the consideration should also factor in whether to use the implant abutment for both stability, support and retention. Stability can be viewed in three planes and the resistance to these three planes can be provided by the framework design and proper clasp design. In situations where the design lacks adequate resistance to both horizontal and vertical forces, the retentive element of the implant abutment may deteriorate quickly as a result of excessive forces directed to the retentive element.
In addition, the use of framework or mesh reinforcement should be planned well to ensure the denture has the thickness and strength to withstand the occlusal forces and to minimize the risk of denture fracture.
Proper understanding of the denture framework design is important for the success for this type of prosthesis.
Execution consideration and Potential Complication
1/Tooth preparation with the implant angulation in mind
During the tooth preparation phase, it would be helpful to place impression copings on the implants to help with preparing guide planes, rests seats and modifying the height of contour. This can help ensure the proposed path of insertion is as parallel to the implants as possible.
2/Fixture Level Impression to keep restorative options open
The decision of what abutments to use can be planned in advance. However, it is the author’s preference to make this type of restorative decision until after the tooth position has been tried and verified. As a result, during the prosthetic treatment, a fixture level impression is often planned instead of an abutment level impression. This master cast will then allow the lab technician to select any abutments appropriate after the case is properly mounted and the available prosthetic space can be carefully analyzed. Sometimes what was planned may turn out to be unsuitable and by having a fixture level impression, the option to select other restorative abutments is still possible.
3/Attachment Pick up Flexibility
In implant supported removable partial denture, in addition to the selecting the correct abutments, the attachments should be connected to the prosthesis accurately in order to function properly. In using attachments, they are incorporated into the denture with a metal cap or a housing. This housing can be connected to the denture by the acrylic. It can also be casted to the metal framework. Or it can be laser welded to the metal framework. In designing the prosthesis, it is the author’s experience to keep the housing separate from the metal framework if possible. At the insertion appointment, if the attachments are not engaging to the abutments, the housing can be easily removed from the acrylic and they can be picked up again during a chairside procedure.
Unlike clasps on teeth, the teeth have a level of flexibility due to the presence of periodontal ligament. With attachments on implant abutments, there is no room for forgiveness as implants do not move. To design an implant supported RPD, it is important to have a strategy to counteract any possible denture processing error so the attachments can be related to the abutments correctly at chairside if needed.
Conclusion/Summary:
The use of dental implants in a removable solution in a partial edentulous patient can be a versatile, cost effective and conservative treatment solution for many patients. This article presents three different clinical cases to illustrate how dental implants are used to improve the support, retention and the aesthetic outcome of the removable prosthesis. The additional treatment planning and execution consideration have been discussed as well. An implant supported removable partial denture can offer an alternative treatment solution for partial edentulous patients who may not be candidates for the more invasive treatment solutions.
Oral Health welcomes this original article.
References
- Bergendal, B., Anderson, J. D., & Müller, F. (2009). Comprehensive Treatment Planning for the Patient with Complex Treatment Needs. In Osseointegration and Dental Implants (pp. 43–62). Wiley‐Blackwell. https://doi.org/10.1002/9780813804644.ch3
- Carr, A. B., & Brown, D. T. (2016). Considerations for the Use of Dental Implants with Removable Partial Dentures. In McCracken’s Removable Partial Prosthodontics (Thirteenth Edition, pp. 146–153). https://doi.org/10.1016/B978-0-323-33990-2.00012-2
- Gates WD 3rd, Cooper LF, Sanders AE, Reside GJ, De Kok IJ. The effect of implant-supported removable partial dentures on oral health quality of life. Clin Oral Implants Res. 2014 Feb;25(2):207-13. doi: 10.1111/clr.12085. Epub 2012 Dec 21. PMID: 23278481.
- Simon H, Yanase RT. Terminology for implant prostheses. Int J Oral Maxillofac Implants. 2003 Jul-Aug;18(4):539-43. PMID: 12939005.
- Müller, F., Barter, S., & Barter, S. (Stephen). (2016). Implant therapy in the geriatric patient. Quintessence Publishing Company, Ltd.
- Ali, Z., Baker, S. R., Shahrbaf, S., Martin, N., & Vettore, M. V. (2019). Oral health-related quality of life after prosthodontic treatment for patients with partial edentulism: A systematic review and meta-analysis. The Journal of Prosthetic Dentistry, 121(1), 59–68.e3. https://doi.org/10.1016/j.prosdent.2018.03.003
About the Author
 Beatrice Leung received her Doctor of Dental Surgery degree at the University of Toronto. After graduation, she completed a General Practice Residency at the Boston Medical Center and a three-year Prosthodontics Residency Program at the University of Pittsburgh, while earning a Master of Public Health degree. Following these programs, she became certified as a fellow of the Royal College of Dentists of Canada as well as the diplomate of the American Board of Prosthodontics. Since then, she has been in private practice in the Toronto for the last 15 years. She recently joined the Faculty at University of Toronto as an Assistant Professor and was named an Honourary Class Member from the class of 2021, 2022 and 2023. Dr. Leung is a recipient of the 2019-2020 Dr. Bruce Hord Master Teacher Award.
Beatrice Leung received her Doctor of Dental Surgery degree at the University of Toronto. After graduation, she completed a General Practice Residency at the Boston Medical Center and a three-year Prosthodontics Residency Program at the University of Pittsburgh, while earning a Master of Public Health degree. Following these programs, she became certified as a fellow of the Royal College of Dentists of Canada as well as the diplomate of the American Board of Prosthodontics. Since then, she has been in private practice in the Toronto for the last 15 years. She recently joined the Faculty at University of Toronto as an Assistant Professor and was named an Honourary Class Member from the class of 2021, 2022 and 2023. Dr. Leung is a recipient of the 2019-2020 Dr. Bruce Hord Master Teacher Award.