BACKGROUND:
Six years ago, in the May issue of Oral Health, I wrote a case report on the successful treatment of root resorption in the lower premolar with the help of Er,Cr:YSGG and diode lasers. The case was diagnosed as hopeless by a local endodontist who recommended extraction. The patient was willing to try a photo-acoustic approach to three-dimensional debridement of the destroyed canal space with a lingual perforation seen under a microscope by the endodontist. (Fig. 1) In 2017, this case lasted 3 years longer than anyone else anticipated and I was pretty proud of the result and this alternative to extraction which I was able to offer my patients using this new laser technology. (Figs. 2A-C) However, the article stirred quite a storm with some endodontists who felt that a) I didn’t know what I was talking about with respect to proper diagnosis, b) lasers have not been shown effective in scientific literature and c) I had no business treating this case as a general practitioner. So, I started searching the literature and learning more about diagnosis, prognosis, classification, and conventional treatments available. Why? Because I have seen more resorption cases in my practice in the last five years than in my first fifteen years since graduation in 1999.
Fig. 1

Fig. 2A

Fig. 2B

Fig. 2C

Fig. 2D

DIAGNOSIS AND CLASSIFICATION
1. The simplest and oldest possible classification of root resorption is based on the location of the lesion: internal originates inside the tooth in the pulp and external attacks the tooth from outside or the periodontium.
2. Tronstad Classification in 19881 was based on presence of inflammation.
a. Progressive Inflammatory characterized by the pulpal (internal) or sulcular (external) infection
b. Invasive Non-inflammatory characterized by its cervical location
c. Replacement Non-inflammatory characterized by ankylosis
3. Trope Classification in 19982 was based on etiology. Two conditions necessary for resorption to occur are damage to the root surface (either pre-dentin internally or pre-cementum externally) and presence of inflammation adjacent to the damaged root surface.
a. Transient or present only for a certain period of time, self-limiting
b. Progressive indicating slow chronic and ongoing assault on the tooth
4. Heithersay Invasive Cervical Resorption (ICR) Classification in 19993 focused further on Tronstad’s Invasive Non-inflammatory type of resorption and divided it into 4 Classes.(Fig. 3) This clinical classification is based on the extent of the lesion and damage to the tooth structure, it is directly related to the likelihood of success of the clinical intervention, be it restoration or endodontic therapy.
Fig. 3

5. Fuss Classification in 20034 is based on two etiological factors: injury which may be mechanical (trauma, surgical intervention excessive pressure) or chemical (high concentration peroxides and other agents) and stimulation determined by factors affecting osteoclastic cells such as infection or pressure.
a. Pulpal infection root resorption (most common)
b. Periodontal infection root resorption
c. Orthodontic pressure root resorption
d. Impacted tooth or tumor root resorption
e. Ankylotic root resorption
6. Lindskog Classification in 20065 subdivides resorption into three main groups with simple and clear distinctions which provide important clues to the appropriate clinical management.
a. Trauma induced where damage to cementum stimulates clastic activity. Can be subdivided into:
i. Surface resorption
ii. Transient apical internal resorption
iii. Pressure resorption
iv. Orthodontic resorption
v. Replacement resorption
b. Infection induced
i. Internal Inflammatory
1. Apical
2. Intraradicular
ii. External Inflammatory
iii. Communicating Internal-External
c. Hyperplastic Invasive
i. Internal (invasive) Replacement Resorption
ii. Invasive Coronal Resorption
iii. Invasive Cervical Resorption (ICR)
iv. Invasive Radicular Resorption
INVASIVE CERVICAL RESORPTION (ICR)
In this article, I would like to focus on ICR, as I am sure we are all seeing an incredible increase in the incidence of these cases recently. Radiographically, this type of resorption may appear internal at a first glance and is frequently misdiagnosed. However, if we consider where it originates, it is definitely a type of external resorption which starts in the sulcular region around the cemento-enamel junction (CEJ), invades the dentin and spreads silently towards the pulp (without invading it) and in both coronal and apical directions. (Figs. 4A,B) In the absence of
treatment, ICR will destroy the tooth structure and lead to eventual loss of the affected tooth. Hyperplastic invasive resorption presents a serious treatment challenge due to it silent and insidious nature, the process has been compared to Fibrous Dysplasia where resorbing tissue invades the tooth in a destructive uncontrolled fashion. Clinically, it may appear as a slight pinkish color change, but more-often it is simply found at recalls on routine radiographs.6
Fig. 4A

Fig. 4B

PREDISPOSING FACTORS
Heithersay3 lists a number of potential predisposing factors leading to the development of ICR, such as trauma, orthodontic tooth movement, surgery and intra-coronal bleaching, but most cases I see clinically do not fit into any of these categories. Unknown etiology, lack of treatment options and poor prognosis, is what connects all these cases. The process reminds me of auto-immune diseases, such as diabetes or rheumatoid arthritis where the body attacks itself because it is no longer recognized as self. The signal telling osteoclasts to stop when they encounter cementum or dentin is missing and the normal process of bone remodelling does not stop at the interface with the tooth but, instead, continues into the tooth thus destroying it. We know that some auto-immune diseases can be triggered by viral infections, so is it a far stretch to suggest that ICR pandemic we are witnessing is also caused by an unknown viral infection damaging signal identifiers on the surface of dentin or cementum at the CEJ.
Of course, it could also be simply due to exponential increase in orthodontic treatment and both vital and non-vital bleaching in our cosmetically driven society. In the last twenty years, the concentration of both at-home and in-office bleaching gels increased from 3% hydrogen peroxide and 10% carbamide peroxide to 35% and 22% respectively. Orthodontic treatment went from being a luxury only some parents could afford to a right of passage every teenager is expected to go through and parents plan for it the same way they contribute to their kids RESP’s.
TREATMENT
In order to be successful at ICR treatment, first and foremost, proper diagnosis and localization of the lesion is essential. Once diagnosed, it is not enough to eliminate the cause of the lesion, a complete removal and inactivation of the resorptive tissue is necessary to prevent recurrence. Due to invasive nature of infiltrative resorption, small channels are created within dentin and may be interconnected with the periodontal ligament apically to the location of the main body of the lesion. For small and localized Class 1 and 2 ICR lesions, Heithersay reported treatment success rate to be close to 100%. Moderate Class 3 lesions have lower 77.8% success rate, but for the extensive Class 4 lesions only 12.5% success can be expected if treatment is attempted. A clinician must disclose the reported success rates of treatment and informed consent must include three treatment options: 1) No treatment followed by tooth extraction when becomes symptomatic; 2) Immediate extraction and prosthetic replacement; 3) Access, debridement and restoration of the resorptive lesion.7 In case of Class 1 and 2 lesions, debridement and restoration is typically chosen, but in case of Class 3 or 4 option 1 or 2 makes more sense, unless, of course, the patient is determined to explore all possible avenues, no matter how slim the chances of success may be; and the clinician is willing to practice Hero-dontics.
The decision whether to treat, simply observe or refer to a specialist and make it their responsibility depends on the knowledge, skill and experience of the dentist initially diagnosing ICR. Some of the factors influencing the decision are:
Access. Can I get to the entirety of the lesion and remove it completely? Do I have the tools required to expose, visualize and remove ICR lesion?
Restorability. Do I have the material to restore the missing tooth structure? Is my material compatible with the moist sub-gingival environment. Do I have hemostasis under control?
Longevity. How much of the tooth structure is destroyed by ICR? Will the tooth last another 5-10 years after all the effort on your part and expense on the part of your patient?
Theoretically, ICR will grow slowly and asymptomatically, without ever invading the pulp, as it is walled off by a protective pre-dentine and dentine barrier. It may take many years for tooth to become symptomatic, (Fig. 5) so No Treatment is a valid option.
Fig. 5
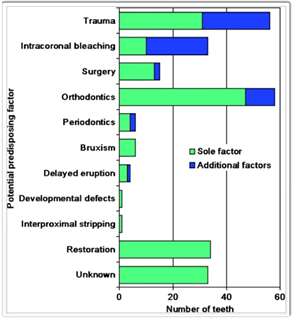
Fig. 5A

Fig. 5B

Fig. 5C
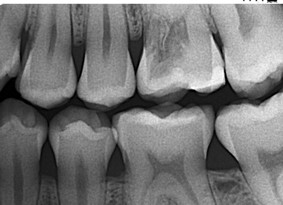
Fig. 5D

If one is lucky, the lesion will start at CEJ and progress coronally faster than apically or towards the pulp. In this case we would see a pinkish color creeping under the shell of enamel and, if we move our explorer subgingivally, we will fall into the lesion where it first entered the tooth. These Class 1 or 2 Heithersay classification lesions usually carry much better prognosis and are treated in the same fashion as a subgingival Class V decay with restorations using materials, such as glass ionomers (Gi), resin modified glass ionomers (RMGI) and mineral trioxide aggregate (MTA). In this situation, all tissue lasers, such as Er,Cr:YSGG 2780nm Waterlase Iplus or Express (Biolase, Irvine, CA) are invaluable in their ability to remove both hard tissue of the tooth, soft tissue of the ICR lesion and control of hemostasis long enough to place final restoration in the same appointment. (Fig. 6A-D)
Fig. 6A

Fig. 6B

Fig. 6C

Fig. 6D

However, eventually the tooth will become symptomatic or simply break due to the destruction of internal dentin structure. In 2011, a female patient presented with painful tooth 34, sensitivity to percussion and negative cold test indicating necrosis. (Fig.7) Clinical examination did not find decay, restoration, fractures, no history of trauma, vital bleaching or orthodontic tooth movement. Only after periapical X-ray was taken and diagnosis of necrotic tooth with periapical pathology was confirmed, we could see the cervical subgingival lesion of Class 3 ICR responsible for the symptoms. In Class 3 and 4 lesions, removal of the resorptive tissue will inevitably lead to pulp involvement, if it is not already involved, and so endodontic treatment will be a necessary part of your protocol, should you decide to treat these lesions. Access to the canal should be performed through the resorption cavity to keep as much healthy tooth structure as possible. Eleven years later, the patient still has this tooth in function following laser-assisted photoacoustic debridement of the infiltrative fibro-vascular tissue, endodontic therapy and placement of subgingival Class 5 composite restoration.
Fig. 7A

Fig. 7B

Fig. 7C

tooth 34L.
Fig. 7D

tooth 34L.
The reason for such poor success rates for the treatment of Class 4 ICR lesions is that the defect could not be reached without surgery to remove alveolar bone and/or orthodontic extrusion. Strictly internal treatment through endodontic therapy and TCA is preferred but whether careful mechanical and chemical debridement can stop the resorptive process, completely eliminate invasive tissue and leave sufficient radicular structure intact to offer longevity to the tooth is the most important question in the decision-making process whether to treat or extract. This is where I feel all-tissue lasers such as Waterlase IPlus (Biolase, Irvine, CA) can aid in minimally invasive, controlled removal of fibro-vascular invasive tissues while preserving healthy radicular tooth structure using photo-acoustic shock waves generated during the unique photon-induced water-mediated ablation process.
CONVENTIONAL TREATMENT WITH
TRICHLORACETIC ACID (TCA)
Treatment of Class 1 and 2 lesions consists of curettage of the fibrous-vascular tissue from the resorption cavity and restoring the defect with a suitable restorative material. Topical application of 90% TCA will cause coagulation necrosis which renders the resorptive tissue avascular and provides haemorrhage control in sub-gingival environment to allow placement of a restoration. It may also help prevent recurrence by inactivating potential resorptive cells which may exist further away from the main lesion. The 90% aqueous solution of TCA on a small cotton pellet is applied for 1-2 minutes with gentle pressure to the resorptive lesion.
Treatment of Class 3 and 4 lesions will inevitably have pulp involvement and endodontic therapy should be performed through the resorption cavity after completing initial access and debridement, as with Class 1 and 2 lesions. TCA application may need to be extended to 3-4 minutes and repeated 2-3 times depending on the extent of the lesion. Next, infiltrating tissue encircling the canal must be removed either with hand instruments or Gates-Glidden drills. When using rotary instrument, care must be taken to avoid perforations. TCA is applied internally to help visualize the extent of resorption defect and the canal is dressed with an antibiotic/ corticosteroid paste, such as Ledermix8 which has been shown to have anti-clastic properties, or calcium hydroxide and Cavit (3M/ESPE) and left alone for 2-3 weeks. Upon re-entry, temporary filling and intra-canal dressing are removed by irrigation and sonic activation, resorption cavity should be examined again and treated with TCA, if necessary, prior to obturation and restoration. TCA is a hemostatic agent with a pH of 1, manufactured by chlorination of acetic acid, and has been used in medicine and dentistry for over a century.9 When applied to the resorptive tissue, it contacts both hard tissues (dentin and enamel) and soft tissues around the compromised tooth. Schwartz et al in 20107 warn against contact of TCA with gingival tissues as it is very caustic and will cause burns when in contact, not exhibit any inflammatory reaction and healed uneventfully.10 The duration of 90% TCA application has been shown to progressively influence microhardness and affect bond strength. 30 seconds application creates rough enamel surface, 60 second application results in exposure of enamel prisms and after 90 seconds, the etched pattern disappears, and erosion of the enamel is observed. Dentin treated with 90% TCA is severely demineralized and is not a good substrate for placement of GI restorations because of the lack of available calcium or for bonded restorations because dentin bonding agents cannot fully infiltrate the demineralized tooth structure. Before any restorative procedure is attempted, the tooth surface must be refreshed with a slow speed round burr to provide hard dentin surface.7 In 1994, Galun et al11 showed TCA to be an effective dentin conditioner which increased shear and tensile bond strength of GI restorations (but in lower concentrations of 35% and 50% than used in the treatment of ICR). Hemostatic effectiveness of lower concentration of TCA is similar to the 90% formulation. After irrigation with water, there is no debris left to interfere with bonding and the absence of smear layer observed enables deeper penetration into the dentinal tubules. Perhaps, more research is needed to show that TCA concentrations of 35%-50% can be equally effective at coagulation necrosis in the treatment of ICR while avoiding caustic collateral damage to the gingival tissues and acting as an excellent dentin conditioner, controlling bleeding and crevicular fluid, for bonding GI restorations.
FOLLOW UP AND DISCUSSION
The case of Class 4 ICR on tooth 45 treated in 2014 (Figs. 1,2) has now been successful for 8 years without the invasive surgery or the use of TCA. CBCT was taken in 2017 to evaluate the fill of the resorptive defect. (Fig. 8) One can clearly see the point of initial invasion from the lingual aspect and the extent to which Endo-Rez UDMA (urethane dimethacrylate) resin based, self priming endodontic sealer (Ultradent, South Jordan, UT, USA) filled the space, previously occupied by resorptive tissue. In 2018, the lingual recession exposed the resin-filled invasive channels in the radicular dentin, the root surface was debrided, minor gingival recontouring was performed using the same minimally invasive photo-acoustic process with Waterlase IPlus Er,Cr:YSGG 2780nm laser, and Class 5 bonded composite restoration was placed.(Figs. 9A-D) In 2019, the patient was diagnosed with a very rare brain tumour, Acoustic Schwannoma and spent 6 months undergoing chemotherapy, radiation and fighting for his life. He survived this challenge with unilateral partial facial paralysis and hearing loss on the left side, just like his tooth 45 survived poor prognosis 6 years previously on the right side. No one knows or can predict what life has in store for us.
Fig. 8

The decision whether to perform Hero-dontics and treat Class 3-4 ICR or to take the easy road and extract, should not be taken lightly. Discussion with patients and explanations of different options available, pros and cons of each is critical for the informed consent. The patient from Fig. 4A (tooth 46) is being followed by a periodontist and chose no treatment, the patient from Fig. 4B (tooth 37) chose to have his tooth extracted once it became symptomatic 2 years after initial diagnosis and decision not to treat nor seek specialist consultations to discuss other options. Post-orthodontic patient from Fig. 5 (tooth 26) has had me follow his tooth for the past 10 years with no treatment and is still asymptomatic, the ICR is clearly progressing and will eventually lead to the loss of the tooth and the patient is aware. The patient from Fig. 7 (tooth 34) presented with pain and chose to try and treat the Class 3 ICR lesion, she is very happy with her decision 11 years later. The patient from Figs.1,2,8,9 is also happy with his decision to try and save his “hopeless” tooth, after 8 years, it’s still going strong.
Fig. 9A

Fig. 9B

restoration 2018
Fig. 9C

restoration 2018
Fig. 9D

My most recent case is illustrated in Figs. 10,11 with CBCT before and after treatment and 2-year follow-up. It is everyone’s worst nightmare: losing 2 front teeth, 31 and 41. The patient with no history of trauma, bleaching or orthodontic treatment was being followed after keratocyst enucleation in 42/43 area 2 years prior. The keratocyst returned and ICR lesions in teeth 31 and 41 were accidental findings on CBCT. He chose to have ICR lesions treated after a consult with an endodontist and advice to do nothing or extract the teeth. Whether he made the right decision or not, time will tell, but for now, four years later, the teeth 31 and 41 appear to be stable and are asymptomatic; the area of recurrent keratocyst I am less optimistic about, but the oral surgeon has treated it again and is monitoring for possible recurrence.
Fig. 10A
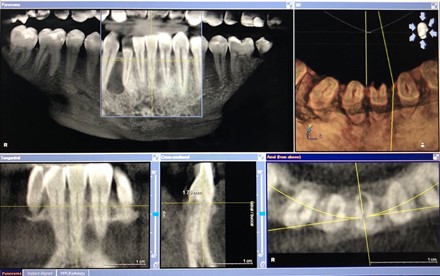
Fig. 10B

Fig. 11A
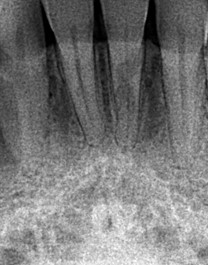
Fig. 11B
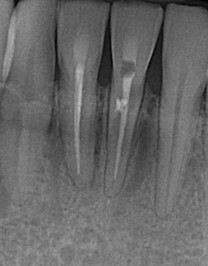
Fig. 11C

CONCLUSION
There is no question that Invasive Cervical Resorption is becoming more prevalent in 21st century than ever before but the treatment options and prognosis have not changed much in the last 30 years. Etiology is still very much unknows, although some predisposing factors, such as trauma, internal bleaching, surgery and orthodontic tooth movement have been suggested. Diagnosis of ICR almost inevitably spells a death sentence to the affected tooth. I hope this article will shed some light on the classification of resorption in general and, specifically, where ICR fits into the greater scheme of things. Proper diagnosis is essential for informed consent and improved prognosis of treatment, should access, debridement and restoration be selected by the patient.
Whether we choose to treat, observe or refer, one thing is for certain: we need to collaborate with each other and look towards new technologies to help improve existing success rates in order to save more teeth in this ICR pandemic.
Oral Health welcomes this original article.
Acknowledgements: Thank you to the Capital Endodontics of Ottawa, ON, Canada for providing pre-op photo of the ICR defect intra-coronally, as seen through the microscope.
Thank you to Dr. Justin Kolnick of Westchester, NY, USA for reviewing this article.
Disclosure: The author of this article is a Clinical Mentor and Key Opinion Leader for Biolase, Irvine, Ca, but has no financial interests in the sales of Biolase lasers.
REFERENCES
- Tronstad L. Root resorption – etiology, terminology and clinical manifestations. Endod Dent Traumatol 1988; 4:241-252.
- Trope M, Root resorption of dental and traumatic origin: Classification based on etiology. Pract Periodontics Aesthet Dent 1998; 10:515-522.
- Heithersay, G.S. Invasive cervical resorption an analysis of potential predisposing factors. Quintessence Internatioonal 1999; 30.2.
- Fuss Z, Tsesis I, Lin S. Root resorption – diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol 2003; 19:175-182.
- Lindskog S, Heithersay GS, Peirce AM. Dental resorptions. In: Scandinavian Yearbook of Dentistry. Blackwell Munksgaard, 2006.
- Heithersay GS. Management of tooth Resorption. Australian Dental Journal 2007; 52(1S):105-121.
- Schwartz RS, Robbins JW, Rindler E. Management of Invasive Cervical Resorption; Observations from Three Private Practices and a Report of Three Cases. JOE 2010; 36(10):1721-30
- Pierce A, Lindskog S. The effect of an antibiotic/corticosteroid past on inflammatory root resorption in vivo. Oral Surg Oral Med Oral Pathol 1987; 64:216-220.
- Khoroushi M, Tavasoli. The Effect of Trichloracetic Acid as a Hemostatic and etching Agent on the Morphological Characteristics and Shear Bond Strength of Resin Composite to Enamel. Operative Dentistry 2010; 35(2):187-193.
- Heithersay GS, Wilson DF. Tissue responses in the at to trichloracetic acid – and agent used in the treatment of invasive cervical resorption. Australian Dental Journal 1988; 33(6): 451-461.
About the Author
 Dr. Marina Polonsky graduated from the University of Toronto, Canada in 1999, with the Dean’s Gold Medal of Achievement. Dr. Polonsky holds a Mastership with WCLI (World Clinical Laser Institute), Mastership with ALD (Academy of Laser Dentistry), Master of Science degree in Lasers in Dentistry from RWTH University in Aachen, Germany. She is a founder of the Canadian Dental Laser Institute (CDLI), Dr. Polonsky is a Chief Editor of Laser Dentistry issue of the Oral Health Journal and is a member of the Executive Committee of Oral Health. Dr. Polonsky is the author of multiple scientific papers and case reports on the use of lasers in dentistry, she serves on the editorial advisory boards for JLAD (Journal of Laser-Assisted Dentistry) and LIDS (Lasers in Dental Science) by Springer
Dr. Marina Polonsky graduated from the University of Toronto, Canada in 1999, with the Dean’s Gold Medal of Achievement. Dr. Polonsky holds a Mastership with WCLI (World Clinical Laser Institute), Mastership with ALD (Academy of Laser Dentistry), Master of Science degree in Lasers in Dentistry from RWTH University in Aachen, Germany. She is a founder of the Canadian Dental Laser Institute (CDLI), Dr. Polonsky is a Chief Editor of Laser Dentistry issue of the Oral Health Journal and is a member of the Executive Committee of Oral Health. Dr. Polonsky is the author of multiple scientific papers and case reports on the use of lasers in dentistry, she serves on the editorial advisory boards for JLAD (Journal of Laser-Assisted Dentistry) and LIDS (Lasers in Dental Science) by Springer













