Statement of Problem
It has been established that maintenance is of utmost importance in the delivery of comprehensive prosthodontic treatment. Therefore, consideration of the possible factors which impact the maintenance phase is essential to take into account during the treatment planning stage. Although, most clinicians recognize the importance of prosthesis maintenance, few of them are able to recognize what this entails in clinical practice. This can result in compromised clinical outcomes that could have been avoided if a proper maintenance protocol was followed. In addition, many patients underestimate the importance of follow-up visits with their dentists which can result in progression of undetected problems that may affect the successful outcome of the dental implant restorations.
Purpose
This scoping review has been conducted to discuss the key factors that can potentially help the clinicians in developing a thorough and clinically relevant maintenance protocol for patients with dental implant restorations.
Materials and Methods
In this scoping review we searched two data bases, with no date limits, for articles on maintenance of dental implant restorations. Out of 55 articles screened, 19 articles were included. Data from these studies were reviewed and thematically analysed to identify key factors in designing or planning maintenance protocols for dental implant restorations.
Results
A total of 18 articles were reviewed in this paper based on their relevancy to the clinical issue.
Owing to the varying prostheses, methods, and evaluation techniques, it was difficult to make an accurate comparison. The maintenance phase is complex and involves various risk factors and parameters that should be considered. These include but are not limited to health history, clinical findings and clinician/implant factors.
Conclusion
Based on the reviewed articles, it has been determined that development of the maintenance phase should be based on a thorough evaluation of the potential risk factors and the potential complications that may arise from these factors. Informed consent is paramount with respect to these potential complications and the significance of maintenance in the long-term success of the implant restoration.
Introduction
Dental implant restorations are one of the most commonly used treatments for rehabilitation of function and esthetics of partially and/or completely edentulous patients. Few studies exist that discuss the determinants in the development of the maintenance phase for an implant prosthesis. It is critical in the treatment planning phase to be cognizant of what treatment or monitoring will be required during the maintenance phase. It is the responsibility of the clinicians to explain the need for regular maintenance and recall visits to the patients. However, it is not uncommon for both the clinician and the patient to give little to no consideration to this phase until delivery and usually only after an issue has developed. Key factors need to be identified from the available literature which in turn will guide the clinician in designing and customizing maintenance protocols.
The aim of this scoping review is to address the gap in developing maintenance protocols by describing the key factors relevant in its creation. For example, in the case of patients with a history of periodontal disease, studies have shown that those patients could potentially be at a higher risk for developing implant disease.1,2 In addition, bruxism is a critical issue that should be identified by the clinicians during the treatment planning phase. In this case, an informed consent explaining the possible risk factors as well as continued maintenance visits to monitor any potential changes is of critical importance.
A thorough explanation of these findings/risk factors with an emphasis on the need for maintenance could have a positive outcome on patient compliance. The patient has to be educated as to the importance of closely monitoring the final prosthesis in order to minimize the need for aggressive interventions and/or implant failures.1
Multiple studies have shown that the mechanical and biological complications related to implant restorations can develop and progress rapidly in absence of adverse signs or symptoms. Costa et al have indicated that patients who were assigned to a maintenance program following the delivery of an implant restoration have 50 % less chance of getting peri-implantitis.3 Another study has indicated that there is only a 10 % implant failure for patients with proper maintenance protocols.3 Although there is limited understanding in the mechanism of marginal bone loss around implants, adhering to a regular maintenance protocol, especially in high-risk patients, has demonstrated promise.
Materials and Methods
An electronic search was conducted through PubMed databases as well as OVID search engines with the following key words: (Maintenance or review or follow-up) and (implant* or dental implant*) and (Complication*) and (Peri-implantitis or Implantitis or bone loss). Only English-language peer-reviewed articles were reviewed. The search was not limited to date and included any relevant papers until May 2020. Inclusion criteria was developed with regard to the concept and context of the clinical problem.
Concept: Key factors (patient factors, and prosthesis factors) in designing maintenance protocol for dental implant restorations.
Context/Theory: Maintenance of dental implant restorations for each patient will help in increasing the survival and success rate of dental implants.
A review of all of the titles and abstracts was done to determine articles relevant to the topic. Studies that reviewed the relative risk factors and their impact on maintenance protocol were included. Further manual searches were conducted as determined by reviewing the reference list of the chosen articles. These papers were evaluated for potential relevance to the context of this study.
Results
The initial search identified 55 articles that were pertinent to the context of the scientific question. After examination of the titles and abstracts, 19 articles were selected based on the predetermined inclusion criteria. Searching the references of the selected articles, as well as a hand search, resulted in additional articles. Owing to the various methods, prostheses and evaluation techniques used in the selected studies, it was difficult to make an accurate comparison among them. Several factors and determinants are involved in the development and delivery of the maintenance phase. These include but are not limited to risk factors based on medical and social history, clinical factors related to the implant or peri-implant tissues, periodontal tissues and patient compliance factors. Some of these studies even identified genetic factors related to certain inflammatory mediators.
Discussion
The findings from various studies included in this review suggest that a proper maintenance protocol is one of the most critical factors for the success of implant restorations. Moreover, understanding all of the risk factors that might impact treatment would in turn affect the maintenance protocol, especially in case of higher risk patients. Risk factors which are relevant to the development of a maintenance protocol, can be determined during the initial stages of diagnosis and treatment planning. The factors that contribute to both biological and mechanical complications include bruxism, periodontal disease or refractory periodontitis, smoking, diabetes, use of bisphosphonates or radiation treatment.16,17
Informed consent, which includes a thorough explanation to the patient before treatment begins, will greatly improve patient compliance in the maintenance phase. For this reason, accurate analysis of pre-treatment conditions of the patient such as occlusal loads and parafunctional habits are crucial. Wittneben et al stated that there is a strong association between history of attrition and prevalence of fractured and chipped porcelain in implant restorations.18
The fabrication of a nightguard as well as more frequent recall visits of the implant restorations is recommended when the patient is a bruxer in order to observe any potential mechanical complications.18 However, patients with high occlusal forces and consequently a greater number of implants placed, should have a more detailed informed consent including a comprehensive maintenance protocol. Therefore, a thorough evaluation for signs of bruxism and dental attrition is important in order to plan the number of implants required, material used for the restoration, type of occlusion developed, in addition to prescribing the use of nightguard.
Kinsel and Lin stated that there are relatively fewer complications in the case of bruxers with canine protected occlusion and the use of a nightguard.19
The concept of overloading and its subsequent effect on bone loss is not completely understood in the literature. Naret et al stated that there is no direct relation between bone loss and overload in absence of peri-implant inflammation. However, in the case of poor oral hygiene and overload, signs of bone loss are observed.20
A maintenance program is essential in patients with a history of periodontal disease as they are more vulnerable to peri‐implant disease.10 Identification of peri‐implant disease criteria is very tenuous and there exist varying opinions in the evidence reported considering peri-implantitis.21 The prevalence of peri‐implant disease differs based on the patient group studied and the disease criteria that is being used. It has been conservatively anticipated that peri-implant disease occurs in approximately 10% of implants and 20% of patients during a 5-10‐year period.21 A recent systematic review indicated that peri‐implant mucositis happens in 43% of patients, and peri‐implantitis in 22% of patients.1 On the other hand, Abrektsson stated that probing may be a less valuable tool, than initially assumed, for the diagnosis of peri-implant disease.21 Generally, bleeding on probing (BOP) has high specificity but low sensitivity (variations due to probe types, force employed, angulation etc). In this review it was shown that the prevalence of peri‐implantitis was less than 3% during a 7-16‐year period.21 In contrast to that review, another systematic review as well as expert consensus statement, indicated that bleeding on probing is the most consistent tool for peri-implant disease diagnosis.1 Moreover, accurate evaluation of the probing depth should be closely observed. There is a strong recommendation to use light probing force in order to minimize damage to the supporting periodontal tissue.1,22
Most of the peri-implant disease studies reported in the literature are based on limited sample size, frequently from university clinics, with inconsistent follow‐up time, and are mainly retrospective.23 Consequently, the cases investigated often vary greatly from one another, which makes it challenging to identify trends. The clinical methods used to form a diagnosis of peri‐implant mucositis or peri‐implantitis are inconsistent, making it difficult to pool data for a systematic reviews and meta‐analyses.1,23 Furthermore, there does not exists a body of literature with definitive maintenance protocols.14 Consequently, peri‐implant disease and recall frequency in conjunction with homecare instruction are not well understood. This makes developing maintenance protocols and recommendations problematic. Multiple studies, including a recent systematic review, have showed there is no significant variance in implant survival rate in patients with periodontitis versus those without periodontitis, if the patient is registered in a maintenance program.24,14 However, patients with a history of periodontitis did have an increased amount of marginal bone loss and an increased prevalence of peri-implantitis in association with implants, which has implications in long‐term follow‐up.16 Hardt et al. assessed bone loss and implant loss in patients with or without periodontal disease in their natural dentition.25 They found that 64% of patients with periodontal disease present in their natural dentition had peri‐implant bone loss of 2 mm or more as compared to 24% of the non-periodontal disease patients.
Wennstrom et al. indicated that bone loss was minimal for patients engaged in a maintenance program even though they had history of periodontal disease.26 Monje et al. stated that the prevalence of implant failure is 4 times greater in patients with aggressive generalized periodontitis as compared to those with a healthy periodontium.19 It appears, based on the literature available, that patients with a history of periodontal disease are at a significantly higher risk, in the short-term, for increased bone loss and a greater long‐term risk for implant loss when compared to those without a history of periodontal disease. Maintenance plans have been proven to mitigate these short and long-term results.24
One of the most critical risk factors associated with biologic complications in implant restorations is diabetes mellitus. This can negatively influence the long-term success of treatment, particularly if associated with additional risk factors such as periodontitis, poor oral hygiene or smoking.20,16
Important considerations involve both low HbA1C levels (< 7%) as well as how long the patient has been diabetic.20 Marginal bone loss as well as peri-implantitis occur more frequently in diabetic patients due a collagen disorder that compromises the healing process and bone formation around dental implants.20
Smoking may also elevate the risk of implant failure in diabetics,38 and although the mechanism of bone loss is not entirely understood, it involves a disturbance in the formation and integrity of collagen.16
The most proven controllable risk factor for implant success is reducing or eliminating smoking habits. Tobacco products contribute significantly to periodontal disease and smoking is a preventable risk factor for biologic complications with dental implants.20 Patients who are heavy smokers, defined in one study by smoking more than 30 cigarettes a day, have amplified chances of implant loss compared to those who smoke a fewer number of cigarettes.16
The negative influence of smoking seem to be reduced in patients adhering to a consistent maintenance program.16 It was shown that smokers with poor oral hygiene have higher chance of bone loss compared to non-smokers with poor oral hygiene.20
Due to the increased risk of subgingival plaque as well as the potential of residual marginal cement, cement retained restorations have a higher risk of peri-implant disease. For this reason, the placement of supra-gingival margins and meticulous cementation procedure is indicated in cement retained restorations. (Fig. 1)
Fig. 1
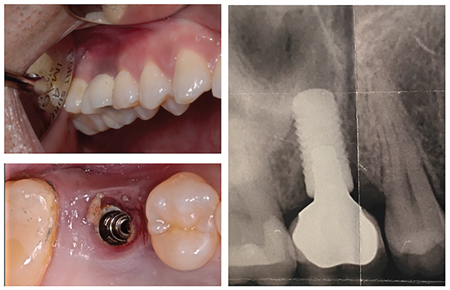
Heitz‐Mayfield et al. indicated that the periodontium associated with cement retained restorations was less responsive to a mucositis treatment after both one- and three-month follow-ups.27 In this study, the baseline bleeding on probing (BOP), suppuration, plaque and pocket depth were measured and recorded. For this reason, many studies recommend planning screw-retained restorations. If a cement retained restoration is unavoidable due to an excessive angulation of the implant positioning, the pre-cementation technique should be employed to allow for maximum elimination of excess cement.27
Heitz-Mayfield et al in 2020 publication introduced the implant disease risk assessment tool, which estimates the risk of a patient to develop peri-implantitis. The combination of risk factors included in this tool can be used for the development of any dental implant restoration maintenance protocol.
Material selection is a means by which the operator can control the risk factors as well. For example, using an all-metal occlusion and a nightguard are shown to decrease implant failure due to mechanical complications.19
As the esthetics of monolithic zirconia restorations improves, utilization of these restorations is likely to increase as long as wear of titanium fixtures from the zirconia can be minimized. The provisional stage is an important tool in the evaluation of the potential risk factors in the long-term success of the restoration. This is particularly significant for full‐arch implant‐supported fixed restorations. High occlusal forces that cause a fracture of the provisional restoration should be an indication for the use of a stronger occlusal material, the use of more implants or of a segmented prosthesis. Moreover, issues with cleansibility and phonetics can be identified during the provisional stage. Modifications can be done in the provisional restoration before moving forward to the definitive restoration. Once form, function and cleansibility have been established, basing the final restoration on the provisional, will result in more predictable outcomes.
Recall guidelines should be developed to consider the identified risks of the patient and should be initially reviewed during the diagnosis and treatment planning phase. Even though there might be an increase in cost and time commitment for the patient, an in‐office recall program proves to be a significant long-term benefit.28
Three-month recall visits should be planned for heavy smokers, diabetic patients with HbA1C levels above 7%. If at-home care proves to be successful, longer recall intervals could be recommended, especially after the first year.1
In any high‐risk groups, such as diabetics, smokers, or those with impaired oral hygiene, triclosan‐containing toothpastes are recommended. Water flossers can be introduced as an effective tool in patients with physical limitations.28 Multiple implant, full‐arch fixed zirconia prostheses with major tissue coverage generally have impaired cleansibility. Before proceeding with the definitive restoration, it is essential that the patient is capable of effective oral hygiene in maintaining periodontal health in association with the provisional restoration. The literature strongly recommends engaging a patient and reinforcing the importance of adhering to the maintenance programs before any signs of biological or mechanical complications arise. Interventions after any signs of peri-implant disease have arisen, can be indicative of incomplete treatment planning and case-management. Peri-implantitis is rarely reversible and can be extremely challenging to manage. It is crucial to identify the disease at the stage of peri-implant mucositis which responds to oral hygiene interventions and can be reversed with appropriate periodontal therapy. However, once the disease has progressed to peri-implantitis, there is an increased chance of bone loss and subsequently the potential loss of the whole prosthesis and/or the supporting implants.21
Maintenance will properly involve at‐home checking of cytokine levels in the crevicular fluid, possibly as regularly as once a week for patients at high risk for peri‐implant disease. The future scenarios for monitoring proinflammatory cytokine levels, tumor necrosis factor, or osteoclastogenesis‐ related cytokines (RANKL) is encouraging.23
The recall exam should involve a thorough evaluation of the medical and dental history, an assessment of the occlusion and potential variations in occlusal contacts, as well as the constancy of proximal contacts. There is a natural mesial drift of dentition and contacts with natural teeth open more often on the mesial side of implants than on the distal.24 Some authors have suggested mesial migration and resulting proximal instability increases in patients with higher biting forces.29 Continuing craniofacial growth can also result in open contacts.30 Using a screw‐retained restoration with a porcelain proximal contact, especially on the mesial, can allow easier correction of an open contact. The authors recommend a broader contact area between an implant crown and a natural tooth, which is often easier to accomplish by lightly disking the adjacent tooth prior to impressions.
Some research has shown that secure contacts can open as soon as three months after insertion of the restoration. If an open contact does occur, it is typically not until two years after insertion.29 Nightguard therapy can aid in retaining tooth position but has not been reviewed or evaluated scientifically. Open contacts can result in periodontal disease, proximal decay on the neighboring natural tooth or peri‐implant disease. Studies suggest suitable diagnostic orthogonal radiographs at prosthesis delivery and six months post-insertion, and then as required, in order to monitor crestal bone levels. Based on the material used and if the prosthesis is screw‐retained, it is advantageous to remove the prosthesis to more precisely assess peri‐implant health, educate the patient on areas demanding better oral hygiene, and, if required, recontour and polish the tissue surface of the prosthesis to increase patient approach. Recontouring the prosthesis for hygiene access is preferably completed in the provisional restoration. The patient’s ability to access and clean all areas of the prosthesis should be assessed, and proper oral hygiene instruction should be taught.
The structure of the recall exam should be considered during the planning phase before treatment has even commenced. There are various factors that should be examined during the recall appointment. This commonly includes probing depth (PD) and its variance over time. In addition, a measure of bleeding on probing (BOP) is important as this can be a key indicator for peri-implant disease.1 There are various recommendations for the regular probing around implants. This study1 indicated that probing even around healthy implants should be done with minimal forces not exceeding 0.25N. The BOP is dependent upon the probe type, diameter, angulation and force employed. This can introduce false positives if the probing is not performed correctly.
The use of minimal force during probing is essential in minimizing damage to the soft tissue.22 Suppuration should also be noted, and can be investigated by placing the gloved thumb and forefinger on the buccal and lingual of the tissue at the implant apex and using mild force coronally to express, if present, any suppuration from the sulcus.
Recall intervals for those with parafunction should be based on the potential for material fracture, compliance in nightguard use, the presence of a screw retained prosthesis, and at‐home maintenance. Patients with high occlusal forces may be at greater risk for developing open contacts. It is important to remember that high occlusal forces can result in long-term implant and prosthesis failure, due to an increase in inflammation, resulting in accelerated biologic changes such as marginal bone loss. Therefore it is essential that the presence of parafunction or heavy occlusal forces are determined as early as possible and the maintenance plan is adjusted to account for a more frequent monitoring schedule.31
The identification of potential biological and mechanical complications is the initial step in the development of a patient specific maintenance protocol. Many potential complications can be avoided with care taken at this step. (Figs. 2 and 3) Based on the total score for every patient, the frequency of the in-office and home care will be decided. This is a very simple and easy way to explain to the patient before the beginning of the treatment. The clinician should determine potential risk factors in long-term success of the treatment and present it to the patient in a checklist format. These factors can be determined through clinical exam, a thorough evaluation of the medical and dental history, social habits as well as radiographic assessment. This checklist should act as a tool in the treatment planning process. For example, in the case of a patient with poor oral hygiene, the clinician should consider material and prosthesis selection based on any clinical findings; in this case, the use of a removable implant prosthesis should be considered. The check list can also be used to motivate and engage the patient in the proper maintenance protocol that is befitting of their risk category. Visualizing a number of check marks from a long list of risk factors can reinforce the need to adhere to a strict recall schedule.
Fig. 2

5 years in function and this was detected during a routine dental examination, with lack of any previous
peri-implant maintenance visits.
Fig. 3

(Reference Book Peri-Implant Complications: A Clinical Guide to Diagnosis and Treatment 2018, by Anastasia Kelekis-Cholakis et al).
As described by Curtis et al there are steps the clinician can undertake in the development of a patient-specific maintenance protocol. These steps are:
- History
- Review
- Motivation
- Treatment options
- Informed consent
The first step is to take a thorough history and a discuss the findings with the patient. The clinician should talk to the patient about modifying behaviours to reduce or eliminate some risk factors such as smoking or poor oral hygiene. As with any behavioural modification, it is important to motivate them to make these changes and explain to them the positive impact this will have on the prognosis of their treatment. As with any treatment plan, an informed consent should be attained, ensuring the patient is aware how certain behaviours, including not adhering to a regular maintenance schedule, will affect the long-term success of their implant and prosthesis.
Conclusion
There have been great developments in implant dentistry and the proper maintenance phase, based on patient related risk factors and clinical observations, has been shown to have a dramatic effect on the long-term performance of implant restorations.
Clinicians should be aware of the importance of every step in the fabrication of the implant restoration, starting from the examination step and followed by the planning. The clear understanding of the patient of the importance of the maintenance phase is the responsibility of the clinician. Once the patient has an informed consent, the maintenance phase becomes a shared responsibility between the patient and the clinician. All these steps can introduce either a step towards a successfully performing implant restoration, or a poorly functioning restoration that can interfere with long-term success and functionality.
Finally, our objective as clinicians in implant dentistry should not be in simply achieving osseointegration of dental implants, it should extend to assuring the optimal functional, stable, and esthetic results of the implant restoration.
Oral Health welcomes this original article.
References
- Jepsen S, Berglundh T, Genco R, Aass AM, Demirel K, Derks J, et al. Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol. 2015;42 Suppl 16:S152-7.
- Qian J, Wennerberg A, Albrektsson T. Reasons for marginal bone loss around oral implants. Clin Implant Dent Relat Res. 2012;14(6):792-807.
- Gay IC, Tran DT, Weltman R, Parthasarathy K, Diaz-Rodriguez J, Walji M, et al. Role of supportive maintenance therapy on implant survival: a university-based 17 years retrospective analysis. Int J Dent Hyg. 2016;14(4):267-71.
- Velasco-Ortega E, Jimenez-Guerra A, Monsalve-Guil L, Ortiz-Garcia I, Nicolas-Silvente AI, Segura-Egea JJ, et al. Long-Term Clinical Outcomes of Treatment with Dental Implants with Acid Etched Surface. Materials (Basel). 2020;13(7).
- Albrektsson T, Canullo L, Cochran D, De Bruyn H. “Peri-Implantitis”: A Complication of a Foreign Body or a Man-Made “Disease”. Facts and Fiction. Clin Implant Dent Relat Res. 2016;18(4):840-9.
- Derks J, Schaller D, Hakansson J, Wennstrom JL, Tomasi C, Berglundh T. Effectiveness of Implant Therapy Analyzed in a Swedish Population: Prevalence of Peri-implantitis. J Dent Res. 2016;95(1):43-9.
- Marcantonio C, Nicoli LG, Marcantonio Junior E, Zandim-Barcelos DL. Prevalence and Possible Risk Factors of Peri-implantitis: A Concept Review. J Contemp Dent Pract. 2015;16(9):750-7.
- Rinke S, Rasing H, Gersdorff N, Buergers R, Roediger M. Implant-supported overdentures with different bar designs: A retrospective evaluation after 5-19 years of clinical function. J Adv Prosthodont. 2015;7(4):338-43.
- Rinke S, Roediger M, Eickholz P, Lange K, Ziebolz D. Technical and biological complications of single-molar implant restorations. Clin Oral Implants Res. 2015;26(9):1024-30.
- Salinas T, Eckert S. Implant-supported single crowns predictably survive to five years with limited complications. J Evid Based Dent Pract. 2012;12(3 Suppl):213-4.
- Papaspyridakos P, Chen CJ, Chuang SK, Weber HP, Gallucci GO. A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. Int J Oral Maxillofac Implants. 2012;27(1):102-10.
- Salinas T, Eckert S. Implant-supported single crowns predictably survive to five years with limited complications. J Evid Based Dent Pract. 2010;10(1):56-7.
- Gruica B, Wang HY, Lang NP, Buser D. Impact of IL-1 genotype and smoking status on the prognosis of osseointegrated implants. Clin Oral Implants Res. 2004;15(4):393-400.
- Joda T, Ferrari M, Gallucci GO, Wittneben JG, Bragger U. Digital technology in fixed implant prosthodontics. Periodontol 2000. 2017;73(1):178-92.
- Roccuzzo M, De Angelis N, Bonino L, Aglietta M. Ten-year results of a three-arm prospective cohort study on implants in periodontally compromised patients. Part 1: implant loss and radiographic bone loss. Clin Oral Implan Res. 2010;21(5):490-6.
- Alsaadi G, Quirynen M, Komarek A, van Steenberghe D. Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection. J Clin Periodontol. 2007;34(7):610-7.
- Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015;42 Suppl 16:S158-71.
- Wittneben JG, Buser D, Salvi GE, Burgin W, Hicklin S, Bragger U. Complication and failure rates with implant-supported fixed dental prostheses and single crowns: a 10-year retrospective study. Clin Implant Dent Relat Res. 2014;16(3):356-64.
- Kinsel RP, Lin D. Retrospective analysis of porcelain failures of metal ceramic crowns and fixed partial dentures supported by 729 implants in 152 patients: patient-specific and implant-specific predictors of ceramic failure. J Prosthet Dent. 2009;101(6):388-94.
- Tawil G, Younan R, Azar P, Sleilati G. Conventional and advanced implant treatment in the type II diabetic patient: surgical protocol and long-term clinical results. Int J Oral Maxillofac Implants. 2008;23(4):744-52.
- Albrektsson T, Buser D, Sennerby L. Crestal bone loss and oral implants. Clin Implant Dent Relat Res. 2012;14(6): 783-91.
- Todescan S, Lavigne S, Kelekis-Cholakis A. Guidance for the maintenance care of dental implants: clinical review. J Can Dent Assoc. 2012;78:c107.
- Mombelli A, Marxer M, Gaberthuel T, Grunder U, Lang NP. The microbiota of osseointegrated implants in patients with a history of periodontal disease. J Clin Periodontol. 1995;22(2):124-30.
- Garcia-Bellosta S, Bravo M, Subira C, Echeverria JJ. Retrospective study of the long-term survival of 980 implants placed in a periodontal practice. Int J Oral Maxillofac Implants. 2010;25(3):613-9.
- Hardt CR, Grondahl K, Lekholm U, Wennstrom JL. Outcome of implant therapy in relation to experienced loss of periodontal bone support: a retrospective 5- year study. Clin Oral Implants Res. 2002;13(5):488-94.
- Wennstrom JL, Ekestubbe A, Grondahl K, Karlsson S, Lindhe J. Oral rehabilitation with implant-supported fixed partial dentures in periodontitis-susceptible subjects. A 5-year prospective study. J Clin Periodontol. 2004;31(9):713-24.
- Heitz-Mayfield LJ, Salvi GE, Botticelli D, Mombelli A, Faddy M, Lang NP, et al. Anti-infective treatment of peri-implant mucositis: a randomised controlled clinical trial. Clin Oral Implants Res. 2011;22(3):237-41.
- Bidra AS, Daubert DM, Garcia LT, Gauthier MF, Kosinski TF, Nenn CA, et al. A Systematic Review of Recall Regimen and Maintenance Regimen of Patients with Dental Restorations. Part 2: Implant-Borne Restorations. J Prosthodont. 2016;25 Suppl 1:S16-31.
- Greenstein G, Carpentieri J, Cavallaro J. Open contacts adjacent to dental implant restorations: Etiology, incidence, consequences, and correction. J Am Dent Assoc. 2016;147(1):28-34.
- Daftary F, Mahallati R, Bahat O, Sullivan RM. Lifelong craniofacial growth and the implications for osseointegrated implants. Int J Oral Maxillofac Implants. 2013;28(1):163-9.
- Chambrone L, Chambrone LA, Lima LA. Effects of occlusal overload on peri-implant tissue health: a systematic review of animal-model studies. J Periodontol. 2010;81(10):1367-78.
About the Author
 Dr. Gebril is a certified Prosthodontist and a Fellow of the Royal College of Dentists of Canada. He is a member of the American College of Prosthodontists, the Association of Prosthodontists of Canada, the Canadian Dental Association, and the Nova Scotia Dental Association. He is an assistant professor at the Faculty of Dentistry, Dalhousie University.
Dr. Gebril is a certified Prosthodontist and a Fellow of the Royal College of Dentists of Canada. He is a member of the American College of Prosthodontists, the Association of Prosthodontists of Canada, the Canadian Dental Association, and the Nova Scotia Dental Association. He is an assistant professor at the Faculty of Dentistry, Dalhousie University.
 Dr. Hamdan is Associate Professor and Director of the Graduate Periodontics Program, Faculty of Dentistry at Dalhousie University, and a certified Periodontist.
Dr. Hamdan is Associate Professor and Director of the Graduate Periodontics Program, Faculty of Dentistry at Dalhousie University, and a certified Periodontist.
 Dr. Al-Waeli has a BDS, M.Sc., and Jordanian Board in Periodontics, and a PhD from McGill University. He is a third-year Periodontics resident at Dalhousie University.
Dr. Al-Waeli has a BDS, M.Sc., and Jordanian Board in Periodontics, and a PhD from McGill University. He is a third-year Periodontics resident at Dalhousie University.
 Dr. Sheikh is trained as a dental clinician and biomaterial scientist with degrees from Baqai Dental College, Queen Mary, University of London and McGill University. He completed two Post-Doctoral Fellowships at the Faculty of Dentistry, University of Toronto and at Mount Sinai Hospital. He is currently a Periodontics and Implant Surgery third-year resident at Dalhousie.
Dr. Sheikh is trained as a dental clinician and biomaterial scientist with degrees from Baqai Dental College, Queen Mary, University of London and McGill University. He completed two Post-Doctoral Fellowships at the Faculty of Dentistry, University of Toronto and at Mount Sinai Hospital. He is currently a Periodontics and Implant Surgery third-year resident at Dalhousie.
 Dr. Sachin Seth has BSc and DDS degrees from Dalhousie University. He obtained his MEd in curriculum development from Acadia University. He is currently an assistant professor and Chair of the Department of Dental Clinical Sciences at Dalhousie.
Dr. Sachin Seth has BSc and DDS degrees from Dalhousie University. He obtained his MEd in curriculum development from Acadia University. He is currently an assistant professor and Chair of the Department of Dental Clinical Sciences at Dalhousie.
Read more articles from the 2021 Proactive Intervention Dentistry issue!












