To achieve a successful aesthetic result and good patient satisfaction, implant placement in the aesthetic zone demands a thorough understanding of anatomic, biologic, surgical and prosthetic principles. The ability to achieve harmonious, indistinguishable restoration from adjacent natural teeth in the aesthetic zone is very often challenging. Placement of dental implants in the aesthetic zone is a technique sensitive procedure with little room for error. The aesthetic complications can adversely impact patients’ lives and the management of the complications are invasive and costly.1 This review is going to illustrate several cases of anterior maxillary single implant treated in my practice with some protocols in place to predictably fulfil patient’s aesthetic demands.
There are some well accepted principles in the replacement of missing teeth with dental implants. Presence of minimum 1.8-2 mm bone in the buccal aspect of implant, adequate soft tissue thickness with quality keratinized tissue, restoratively driven implant surgery with precise three dimensional placement and immediate provisional restoration to support and sculpt the gingival architecture are essential for long term success.2 Immediate screw retained provisional plays a key role to preserve the gingival papillae and soft tissue contour in particular in cases with high smile line, highly scalloped gingiva and long papillae, once it is lost, it is very difficult to rebuild the soft tissue architecture. Alveolar bone loss following tooth extraction can significantly compromise the implant site due to loss of over 50% of bone volume mainly happening within the first 6 months following extraction.3 The alveolar process is the lining of the tooth’s socket and referred to as the alveolus. Although the alveolar process is made up of compact bone, it may also be called the cribriform plate as it contains various holes where Volkmann canals pass from the alveolar bone and into the PDL. The alveolar bone proper is also called the bundle bone because of the Sharpey fibers. A portion of the fibers of the PDL are inserted here. Bundle bone is a tooth related bone mostly nourished by PDL and is extremely thin. This thin bone comprises the most coronal 3-4 mm labial bone in pre maxilla and will eventually be lost to resorption following tooth removal.4 Partial Extraction Therapy is a proven approach to preserve the bone architecture and buccal Plate, PET is a unique treatment alternative that requires one surgical procedure thus reducing patient morbidity, as well as, reducing overall treatment time and cost associated with treatment.5
Case #1: Severe Internal Root Resorption
A 25 years old female with diagnosis of symptomatic root resorption associated with central left incisor (tooth 2.1) was referred for implant therapy. Some challenges in this case are unfavourable sagittal root position in the alveolar bone, thin tissue phenotype, high scalloping gingiva with long papillae and short contact areas, high aesthetic demands and high smile line. Since the biologic width is almost identical at the interproximal and buccal and palatal areas, it is expected that following extraction of this tooth without planning for immediate provisional, the interdental papillae will collapse to 2-3 mm, significantly shorter than the initial presentation with subsequent embrasure gaps and dark triangles. Intraoral scanning of the entire dentition and the cone beam computed tomography (CBCT) was used to complete the digital planning workflow in order to plan for the optimal partial extraction therapy, immediate implant placement, and provision of the immediate screw retained temporary crown. The essential role of the provisional restoration is to maintain the soft tissue architecture and to prevent tissue collapse, formation of dark triangles and open embrasures. Straumann BLX 3.5 x14 mm SLActive was used for optimal primary stability. Final Zceram Straumann ASC screw retained crown was successfully inserted. One year follow up indicated optimal aesthetics, indistinguishable restoration and very happy patient.
Fig 1

Fig. 2

Fig. 3
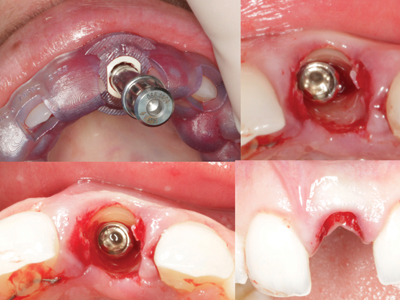
Fig. 4

Fig. 5

Fig. 6

Fig. 7

Fig. 8

Fig. 9
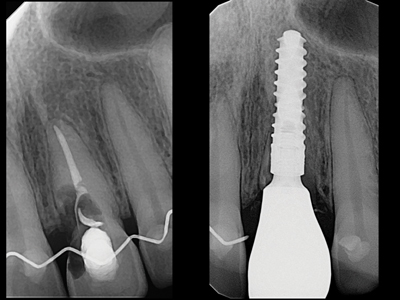
Fig. 10

Case #2: Deep Palatal Groove
A 35 years old, otherwise healthy female, presented with the hopeless maxillary right lateral incisor (FDI # 1. 2) with evidence of massive bone loss as a result of deep palatal groove extending to the apical area and subsequent communicating bacteria. Palatogingival grooves are developmental malformations quite notorious for precipitating endodontic – periodontal lesions. Owing to their inconspicuous occurrence, funnel-shaped morphology and variable extent on tooth root, they promote adherence of plaque and bacteria to levels significant for the development of pathology.6
Initial gingival recession, thin gingival phenotype, high scalloping gingiva and high smile line are some of the challenges of this case. Atraumatic extraction of tooth 1.2 followed by ridge augmentation with 50%-50% autogenous-xenogenic bone graft was completed. The palatal pedicled soft tissue graft with harvest from palate was done at the same surgical appointment to compensate for the thin tissue and to correct the existing gingival recession. 6 months later, Straumann BLX 3.5x14mm with CBCT fully guided protocol was inserted and screw retained PMMA provisional crown was fabricated chair-side to initiate tissue sculpting and papilla support. Final ceramic crown was inserted in 4 months. The two year follow-up shows stable results.
Fig. 1

Fig. 2
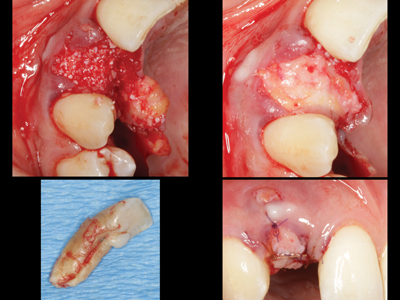
Fig. 3
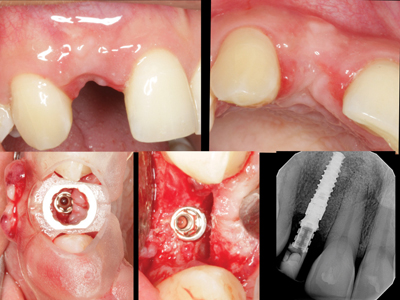
Fig. 4

Fig. 5

Fig. 6

Fig. 7

Fig. 8

Case #3: Management of Peri-implant Soft Tissue Deficiency
This clinical report describes the use of a sub epithelial connective tissue graft to recontour a soft tissue margin discrepancy for a single-implant crown in the anterior maxilla. This procedure demonstrates that the use of soft tissue autograft to correct an aesthetic deficiency may be a feasible approach to establish new and stable peri-implant soft tissue. A 34 years old female patient presented to our office with a dental implant placed about 10 years ago by another practitioner and since then, she noticed the apical migration of soft tissue around implant in the area of 1.1. She had a previous soft tissue surgery and new implant restoration to address the asymmetrical smile; however, that did not seem to resolve her concerns and instead she was left with some incision scars and irregularities on peri-implant soft tissue. In this case, the existing crown was removed and a thick, wide and long de-epithelialized CTG was harvested from palate and was tucked under the tunnel prepared under buccal, palatal, mesial and distal soft tissue. 6-0 Nylon Stabilizing sutures with interrupted and vertical sling was applied to stabilized the graft. 4 months later, new impression for a new screwed retained ceramic crown with ideal sub gingival emergence profile was fabricated. Patient was very pleased with the aesthetic outcome. Although the implant was placed slightly more buccal and apical, the soft tissue compensation could provide acceptable aesthetic for the patient.
Fig. 1

Fig. 2

Fig. 3

Fig. 4

Fig. 5

Fig. 6

Fig. 7

Fig. 8

Fig. 9

Fig. 10
Oral Health welcomes this original article.
References
- Dent Clin North Am 2006 Jul;50(3):391-407, vi. doi: 10.1016/j.cden.2006.03.007.
- 10 Keys for Successful Esthetic-Zone Single Immediate Implants, April 2017, Volume 38, Issue 4, Page 197
- Chapter 8 Wound Healing of Extraction Sockets Roberto Farina, Leonardo Trombelli, 13 April 2012
- Lindhe’s Clinical Periodontology and Implant Dentistry, 2 Volume Set, 7th Edition
- Gluckman H, Salama M, Du Toit J. Partial Extraction Therapies (PET) Part 1: Maintaining Alveolar Ridge Contour at Pontic and Immediate Implant Sites. Int J Periodontics Restorative Dent. 2016 Sep-Oct;36(5):681-7. doi: 10.11607/prd.2783. PMID: 27560672.
- Sharma S, Deepak P, Vivek S, Ranjan Dutta S. Palatogingival Groove: Recognizing and Managing the Hidden Tract in a Maxillary Incisor: A Case Report. J Int Oral Health. 2015;7(6):110-114.
About the Author
 Dr. Mehdi Noroozi is a board-certified periodontist who provides the full scope of surgical periodontal and dental implant therapy. Dr. Noroozi has a special interest in esthetic and reconstructive periodontics and implantology. In addition to private practice, Dr. Noroozi is a clinical assistant professor in the department of graduate periodontics at the University of British Columbia where he is involved in didactic and clinical teaching of periodontics at post-graduate level. Dr. Noroozi has lectured nationally and internationally and published on various topics related to periodontics and implantology. He can be reached at info@implantperiospecialist.com IMPrESS Perio Implant Center, Vancouver, British Columbia, Canada.
Dr. Mehdi Noroozi is a board-certified periodontist who provides the full scope of surgical periodontal and dental implant therapy. Dr. Noroozi has a special interest in esthetic and reconstructive periodontics and implantology. In addition to private practice, Dr. Noroozi is a clinical assistant professor in the department of graduate periodontics at the University of British Columbia where he is involved in didactic and clinical teaching of periodontics at post-graduate level. Dr. Noroozi has lectured nationally and internationally and published on various topics related to periodontics and implantology. He can be reached at info@implantperiospecialist.com IMPrESS Perio Implant Center, Vancouver, British Columbia, Canada.













