Abstract:
Introduction:
Implant-supported prostheses predictably lead to successful esthetic and functional rehabilitations of patients with missing teeth. Nonetheless, technical and biological complications may be encountered including those leading to a dislodgement of an implant-supported prosthesis.
Case report:
An 83-year-old female patient presented to the University of Toronto, Graduate Prosthodontic specialty clinic on an emergency basis regarding dislodgement of a screw-retained implant-supported full-arch bridge restoring an edentulous mandible. Clinical examination revealed prosthetic screw fractures at three implant sites. Following unsuccessful attempt to retrieve the fractured prosthetic screws, multi-unit abutment screws of three implants were replaced, and new prosthetic screws were inserted to retain the existing prosthesis.
Conclusions:
This case report highlights the management challenges in the assessment, diagnosis, and treatment of patients who present with a dislodged implant-supported dental prosthesis. Successful management of implant-related complications is a critical skill that ensures continued functionality of the prosthesis and supporting implants.
Introduction
Patients with fixed implant-supported prostheses may encounter time-dependent technical complications and maintenance challenges.1,2 Some examples of technical complications include loosening of retaining screws, fracture of retaining screws, abutment fracture, and implant fracture. Some of these complications may manifest clinically as dislodgement of the prostheses.3 (Fig. 1) Successful management of the technical complications, such as safe removal of fractured screw fragments, is critical to the continued use of the prosthetic components and prostheses.
Fig. 1
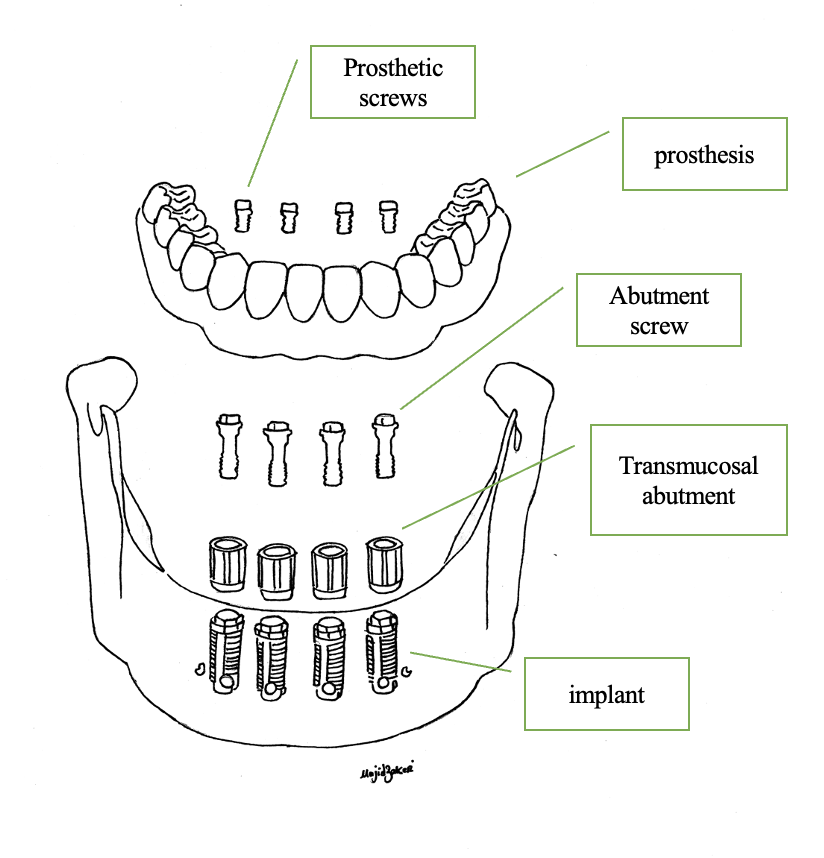
In comparison to the low frequency of abutment and implant fractures, loosening and fracture of retaining screws – such as prosthetic screws and abutment screws – are more common.4,5 Prosthetic screws are very short and narrow screws that anchor multi-unit screw-retained bridges on supporting abutments. Abutment screws are significantly longer and wider than prosthetic screws and are used to anchor abutments to implants as well as single- and multi-unit screw-retained prostheses directly to the implants. A total of 3.9% of abutment screws in screw-retained implant-supported fixed dental prostheses fractured over a five-year period,6 and 0.3% of prosthetic screws in screw-retained fixed dental prostheses fractured over a twelve-year period.2
Multiple aetiologies have been proposed for retaining screw fractures such as undetected screw loosening, excessive occlusal forces, excessive torque application, reduced preload effect, and a lack of “passive fit”.3 Fundamentally, screw fractures occur due to metal fatigue as a result of repeated excessive force application (such as occlusal forces) or uncontrolled torque that exceeds the modulus elasticity of the screw material.7
Case Report
Chief complaint and dental history
An 83-year-old female patient presented to the University of Toronto, Graduate Prosthodontic specialty clinic on an emergency basis seeking treatment for a dislodged screw-retained implant-supported full-arch bridge restoring the edentulous mandible. The patient noticed looseness of the bridge while eating, and the bridge dislodged soon after. (Fig. 2) A review of the patient’s records revealed that implants 33, 32, 31, 42, and 43 were Branemark external hex design (3.75 x 10 mm) and were placed in 1983. Implant 31 was submerged, and mandibular implant-supported full-arch bridge was retained by four implants (33, 32, 42, and 43). The mandibular bridge was delivered in 1984 and refurbished (i.e., had its veneering acrylic replaced while preserving the metal frame) in 2018 to address the wear of acrylic teeth. The patient had a history of prosthetic screw fracture in site 43 in 2015 which was resolved by a local dentist.
Fig. 2A

Fig. 2B

Clinical assessment
Extra-oral assessment was unremarkable. Intra-oral examination revealed that edentulous maxilla was restored with an implant-supported overdenture retained by a bar engaging implants 15, 13, and 23. The edentulous mandible was restored with a screw-retained implant-supported fixed full-arch bridge that was not present in the mouth. Peri-implant soft tissues in the maxilla and mandible appeared generally healthy except localized soft tissue inflammation and tenderness to palpation buccal to implant 32 associated with the edge of the multi-unit abutment that was prominently inclined buccally. (Fig. 3) There was no sensitivity to percussion of implants. Standard straight multi-unit abutments were present on mandibular implants with the abutment-bridge interface being located 4-5 mm supra-gingival. Three fractured prosthetic screws were visible clinically inside abutment screws of multi-unit abutments 32, 42, and 43 as well as within corresponding screw access channels of the dislodged prosthesis. (Fig. 2) Straight multi-unit standard abutment 33 was loose, and screw access channel of the bridge at 33 site was empty implying that the prosthetic screw 33 had loosened previously and was lost.
Fig. 3

Radiographic assessment
Radiographic examination revealed two submerged implants in sites 23 and 31. No peri-implant radiolucency was present around maxillary and mandibular implants. Implants, abutments, and abutment screws of mandibular implants appeared to be intact. Fractured prosthetic screws were present within multi-unit abutment screws of implants 32, 42, and 43. Mandibular straight abutments appeared to be of different heights, with the 32 and 42 abutments being taller than the 33 and 43 abutments. (Fig. 4)
Fig. 4

Exploratory assessment and definitive diagnosis
The basic treatment plan was formulated and consisted of three steps. First, we planned to attempt to remove fractured prosthetic screws. If removal of fractured prosthetic screws in the first step is not successful, then we planned to temporarily remove the mandibular multi-unit abutments diagnostically to measure the height of the abutments and abutment screws to order the appropriate abutment screws for implants 32, 42, and 43. Lastly, we planned to re-insert the mandibular bridge using new prosthetic screws and to double check its fit and occlusion. Specifically, we planned to assess the passive fit of the bridge as well as the quality and distribution of occlusal contacts especially in the posterior cantilevered segments. These concluding assessments of the mandibular bridge may necessitate definitive management on the basis of the diagnostic appointment. The findings of initial assessment and the management plan were discussed with the patient, and informed consent was obtained.
Treatment
First, we attempted to remove the fractured prosthetic screws at 3 sites (32, 42, and 43) utilizing a variety of tools including Endo explorer (HuFriedy DG 16, USA) and ultrasonic instruments (Dentsply, Bobcat Pro 25K). Care was taken not to damage the internal threads of multi-unit abutment screws inadvertently. Unfortunately, we were not able to remove the fractured prosthetic screws.
Next, multi-unit abutment 32 was removed using multi-unit abutment driver, and the height of the abutment was confirmed as 7 mm. (Fig. 5) On the basis of clinical and radiographic assessment, the heights of the multi-unit abutments 33, 42, and 43 were measured as 5.5 mm,
7 mm, and 5.5 mm respectively. Upon removal of multi-unit abutment 32, the soft tissue was found to be healthy around the implant, and the area was flushed thoroughly with chlorhexidine 0.12% solution.
Fig. 5

Internal aspects of all implants were confirmed to be free of damage, and multi-unit abutment screws 32, 42, and 43 were replaced with new ones (Fig. 6) and torqued to manufacturer’s recommendations (15 Ncm) using multi-unit screwdriver and torque wrench. The prosthesis was re-inserted, and the passivity of the prosthesis was tested clinically using several methods. For example, the one-screw test involved hand-tightening a single prosthetic screw at a time and assessing the prosthesis-abutment interface for any gap, which would have represented a misfit.8 No misfit was detected, and all prosthetic screws were inserted and hand-tightened using slot screwdriver. Periapical radiographs also confirmed complete seating of the abutments and prosthesis. (Fig. 7) Occlusal assessment revealed heavy occlusal contacts on the posterior cantilevers, (Fig. 8) and occlusal adjustment were performed to provide even, well-distributed contacts in maximal intercuspation. All prosthetic screws were torqued according to the manufacturer’s recommendation (15 Ncm) using slot screwdriver and torque wrench.
Fig. 6

Fig. 7A

Fig. 7B

Fig. 8

acrylic teeth immediately upon re-insertion of the prosthesis.
Screw access channels were covered with PTFE film tape (3M) and clear polyvinyl siloxane material (Exaclear, GC), and the patient was scheduled for a one-month follow-up re-assessment.
Follow-up
The patient returned one month later for a follow-up re-assessment. The patient did not report any complications or discomfort during chewing or at rest. Clinical assessment revealed a stable mandibular full-arch bridge with bilateral contact in maximal intercuspation and harmonized contacts in lateral excursion. Localized soft tissue inflammation around implant 32 had improved significantly with no purulent discharge and no symptoms upon palpation.
Provisional restorations were removed from screw access channels, and the prosthetic screws were retorqued to 15 Ncm according to manufacturer instructions using a slot screwdriver and torque wrench. Screw access channels were closed with PTFE film tape (3M) and A3 resin composite (3P ESPE) restorations. (Fig. 9) Optimum occlusion was confirmed. The patient was very pleased with the care received. A follow-up visit was planned in one year.
Fig. 9

Discussion
This case report describes the management of a dislodged screw-retained implant-supported full-arch bridge. The clinical and radiographic assessment revealed that the prosthesis dislodged due to multiple prosthetic screw fractures.
Multiple aetiologies have been reported for the abutment or prosthetic screw fracture including the lack of passive fit, undetected screw loosening, excessive occlusal forces, and lack of controlled torque.3 For example, the lack of passive fit of the bridge framework can result in unfavorable prosthesis movements due to flexion and compression forces leading to loosening or fracture of prosthetic screw.9 In a multi-unit screw-retained bridge, an undetected loosened or fractured prosthetic screw at only one implant site can exist for an extended period of time before the increased forces on the remaining screws cause them to loosen or fracture as well leading to a clinically detectable bridge looseness or dislodgement.9
Excessive occlusal force may lead to metal fatigue and subsequently cause screw fracture. Similarly, uncontrolled torque application that exceeds the modulus of elasticity of the screw material and cause its fracture.7 In our clinical case, excessive occlusal contact was noticed on the distal most acrylic teeth which could have contributed to screw fractures and the bridge dislodgement. (Fig. 8)
More than 30 techniques for managing a fractured abutment or prosthetic screw have been described.10 Care must be taken not to damage the internal threads of the implant or abutment during attempts to retrieve fractured abutment screw or fractured prosthetic screw.10 In some situations, fractured prosthetic screws cannot be retrieved safely with use of methods such as a hand instrument, an ultrasonic scaler or a screw retrieval kit due to “cold welding”. In this case, the multi-unit abutment or, in some implant systems, the multi-unit abutment screw can be replaced.
This clinical case demonstrates the challenges encountered in appropriate management of a screw-retained implant-supported full-arch bridge that is made up of multiple prosthetic components (prosthesis, prosthetic screws, abutments, and abutment screws) and multiple interfaces (prosthesis-abutment interface and implant-abutment interface). Having a good understanding of the implant system and its component designs as well as having back-up components in stock are critical when managing prosthetic complications that may require replacement of components.
Conclusion
Technical complications with implant-supported fixed dental prosthesis may manifest as dislodgement of the prosthesis. This case report highlights the management challenges in the treatment of a patients who present with a dislodged implant-supported full-arch bridge and the significance of radiographic and exploratory assessment in guiding definitive care.
Oral Health welcomes this original article.
References
- Chochlidakis K, Einarsdottir E, Tsigarida A, Papaspyridakos P, Romeo D, Barmak AB, et al. Survival rates and prosthetic complications of implant fixed complete dental prostheses: An up to 5-year retrospective study. J Prosthet Dent. 2020;124:539–46.
- Papaspyridakos P, Bordin TB, Kim YJ, El-Rafie K, Pagni SE, Natto ZS, et al. Technical complications and prosthesis survival rates with implant-supported fixed complete dental prostheses: A retrospective study with 1- to 12-year follow-up. Journal of Prosthodontics. 2020 Jan 1;29(1):3–11.
- Henry PJ, Laney WR, Jemt T, Harris D, Rcs F, Krogh PHJ, et al. Osseointegrated implants for single-tooth replacement: A prospective 5-year multicenter study. Int J Oral Maxillofac Implants. 1996;11:450–5.
- Lindquist L, Carlsson G, Jemt T. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants. Clin Oral Impl Res. 1996;7:329–36.
- Attard NJ, Zarb GA. Prospective study treatment outcomes in IS-FDP. Int J Prosthodont. 2004;17:417–24.
- Kreissl ME, Gerds T, Muche R, Heydecke G, Strub JR. Technical complications of implant-supported fixed partial dentures in partially edentulous cases after an average observation period of 5 years. Clin Oral Impl Res. 2007 Dec;18(6):720–6.
- Tolman DE, Laney WR. Tissue-integrated prosthesis complications. Int J Oral Maxillofac Implants. 1992;7:477–84.
- Kan JY, Rungcharassaeng K, Bohsali K, Goodacre CJ, Lang BR. Clinical methods for evaluating implant framework fit. J Prosthet Dent. 1999;81:7–13.
- Katsavochristou A, Koumoulis D. Incidence of abutment screw failure of single or splinted implant prostheses: A review and update on current clinical status. J Oral Rehabil. 2019;46(8):776–86.
- Mizumoto RM, Jamjoom FZ, Yilmaz B. A risk-based decision making tree for managing fractured abutment and prosthetic screws:
A systematic review. J Prosthet Dent. 2018;119:552–9.
About the Authors
 Majid Zakeri earned the DDS degree from Mashhad University of Medical Science, Iran. After practicing general dentistry in Iran and in Canada, he was accepted into the Graduate Prosthodontists Program at the University of Toronto where he is currently a 2nd year resident.
Majid Zakeri earned the DDS degree from Mashhad University of Medical Science, Iran. After practicing general dentistry in Iran and in Canada, he was accepted into the Graduate Prosthodontists Program at the University of Toronto where he is currently a 2nd year resident.
 David Chvartszaid is a Prosthodontist and a Periodontist. He is the director of the Graduate Prosthodontics Program at the University of Toronto and the dentist-in-chief at Baycrest Hospital. He is the past president of the Association of Prosthodontists of Canada.
David Chvartszaid is a Prosthodontist and a Periodontist. He is the director of the Graduate Prosthodontics Program at the University of Toronto and the dentist-in-chief at Baycrest Hospital. He is the past president of the Association of Prosthodontists of Canada.
RELATED ARTICLE: Transition From A Removable To A Fixed Implant-Supported Prosthesis: A Case Report













