
Abstract
Severe mandibular hypoplasia, or micrognathia is a debilitating condition that hinders neonatal breathing, feeding, growth and development. This condition predisposes children to prolonged early life hospital admission, airway embarrassment, obstructive sleep apnea, feeding difficulties, speech delay and caregiver burnout. Many conservative and surgical approaches have been utilized to treat neonates and children for severe micrognathia. In this article, we discuss common presentations of severe congenital micrognathia, their associated challenges and treatments. We also present clinical and radiographic photographs of neonate and pediatric mandibular osteodistraction in the treatment of micrognathia and improvement of the oropharyngeal airway.
Mandibular hypoplasia is an underdeveloped or micrognathic jaw that is abnormally small and retro-positioned with respect to the maxilla. This congenital deformity does not permit adequate room for the tongue to sit passively in the oral cavity, instead it is positioned upwards and backwards over the airway causing intermittent airway obstruction, especially in the supine position and while sleeping. Obstructive sleep apnea (OSA) is often diagnosed via polysomnogram and if left untreated can lead to serious cognitive and neurodevelopmental delay, chronic hypoxia and hypercarbia, cardiovascular and pulmonary complications, and failure to thrive. Neonates with severe micrognathia have difficulties breathing and in severe cases, require early life intubation and intensive care. Feeding difficulties requiring nasogastric tubes to bypass the site of obstruction are often present as well.
Severe mandibular hypoplasia is a hallmark of many craniofacial syndromes, including Pierre Robin Sequence, and Treacher Collins Syndrome. Children with Pierre Robin Sequence have mandibular growth failure during embryogenesis that leads to an abnormally small jaw (micrognathia), upwards and backwards positioning of the tongue (glossoptosis) and often a U-shaped cleft palate. The incidence of this condition is 1 in 8500 births.1 Children with Treacher Collins Syndrome have an embryogenic underdevelopment of their mandible and midface which results in malocclusions, a steep occlusal plane and retro-positioned jaws. The incidence of this condition is 1 in 50,000 births.2 Children with both conditions are frequently diagnosed with OSA and feeding challenges which require extensive early-life multidisciplinary treatment.
Non-surgical or conservative management of the micrognathic jaw and compromised airway is always preferred to surgical treatment, if possible. In patients with Pierre Robin Sequence, 70% of the mild to moderate airway obstruction can be resolved by prone positioning, with or without nasopharyngeal airway.1 Non-invasive ventilation, including Continuous Positive Airway Pressure (CPAP) and Bi-level Positive Airway pressure (BPAP) can be used to stent open the infant’s airway in mild OSA cases. All conservative treatments require a great deal of caregiver attention, training, and expertise. Caregiver burnout is not uncommon when conservative therapies alone are used to manage severe neonatal and pediatric OSA.
Surgical management of the hypoplastic mandible with airway compromise can be accomplished utilizing tongue-lip adhesion (TLA), mandibular distraction osteogenesis (MDO) or tracheostomy. These treatment modalities are reserved for more severe cases of micrognathia-related airway compromise.
Tongue-Lip Adhesion is a surgical technique whereby the tongue is sutured to the lower lip, pulling it forwards and off the airway during the neonatal period. This procedure is reversed, usually around one year of life, when the child has grown sufficiently to hopefully allow for a more patent airway. While TLA is effective in treating OSA in children with mild to moderately retrognathic mandibles, it has a limited effect when used in patients with severe micrognathia.
Mandibular Distraction Osteogenesis (MDO) is a surgical technique utilized for the treatment of the severely hypoplastic mandible. It relies on the principle of osteodistraction which forms new bone between surfaces of bone segments that are gradually separated by incremental traction. The principle introduced by Dr. Gavriil Ilizarov, a Soviet Orthopedic Surgeon in 1948.3 He utilized an external fixation device to apply gentle traction to long bone fractures of soldiers returning from World War II. He found that the traction not only led to better wound healing but lengthened the limb by producing new bone between the broken segments. His technique was later refined and adapted to the craniofacial skeleton in 1992 by Dr. J. G McCarthy, a Plastic Surgeon in New York, USA. A corticotomy was made in the bilateral mandible and external pin fixation devices were applied to both sides of the mandible. The devices were gradually turned, forming bone between the cut segments, and relieving the airway obstruction. Since its inception, MDO has been proven an effective and rapid method to improve neonatal mandibular position and thereby relieve OSA and feeding challenges.
There are four phases of distraction osteogenesis including corticotomy/osteotomy, the latency period, activation period, and the consolidation period. During MDO the distraction devices remain in place during the consolidation period to stabilize the immature bone. They are then removed in a second surgical procedure. CT Scan imaging is usually prior to the first surgery and intra-operatively during the second surgery. The risks of MDO include facial scarring, hardware failure, damage to cranial nerves V and VII, harm to developing teeth, infection, and temporomandibular joint dysfunction.
Over the last decade, several studies have compared the use of TLA and MDO in children with Pierre Robin Sequence who suffer from OSA and feeding difficulties.4-8 In a comparison of post-surgical outcomes between TLA and MDO on Obstructive Sleep Apnea, TLA and MDO had similar postoperative complications, but MDO had a 92% successful resolution of obstructive sleep apnea compared to 47% in TLA.9 TLA’s reliance on ‘catch-up’ growth of the mandible is not feasible in Pierre Robin Sequence, and therefore severe hypoplastic mandibles favors MDO as the treatment choice.2 Zhang et al. demonstrated that both MDO and TLA are effective alternatives to tracheostomy for patients who fail conservative management.8 These surgeries improve feeding and promote weight gain but MDO was superior to TLA in long-term resolution of airway obstruction and avoidance of gastrostomy tube placement.
Although obstructive sleep apnea has non-surgical treatment modalities, MDO presents a relatively fast permanent and predictable solution for severe OSA cases. MDO allows for an improvement in feeding for infants with severe mandibular hypoplasia, who otherwise rely on nasogastric feeding for long periods of time by advancing the mandible into an anterior position and creating sufficient oropharyngeal space for breathing and the passage of food. In a study by Zhangetal, they demonstrated 87% of infants will have successful oral feeding capacity after MDO treatment.
Prior to MDO, the end-stage surgical management for severe airway obstruction in neonates or infants was to perform a tracheostomy. This treatment is often used as a last resort however, due to the regular maintenance required by the parents to prevent mucous obstruction and the increased risk for plugging and sudden infant death. Tracheostomies also risked delaying speech development and have a high morbidity and mortality.8
In most cases, MDO is provided for neonates and infants within the first few weeks and months of life and the success of this life-changing treatment relies heavily on a well-organized team, careful planning and monitoring, follow-up, and well-informed caregivers.10 Our PRS Airway team based at the University of Alberta, Stollery Children’s Hospital has a 20-year history of MDO surgical management of OSA. In this manuscript, we discuss the workup and present surgical cases of neonates and infants with severe micrognathia who underwent MDO. These cases will highlight the positive increase in clinical mandibular position and positive clinical changes seen in the facial profile. Furthermore, an increase in the oropharyngeal airspace can be seen on the post osteodistraction radiographs.
Prior proceeding with MDO, assessment by the following team members is required: Pediatric OMFS, Pediatric Plastic Surgery, Pediatric Respiratory Medicine, Pediatric Otolaryngology, Speech Pathology, NICU/PICU Medical Leads. A preoperative clinical and radiographic assessment of the airway is completed. This includes head CT scan and evaluation of hypoxia, polysomnogram and outcomes of conservative therapies. The PRS Team then convenes to review the assessments and collaboratively decide on further therapies. Once the consensus has been reached by the PRS to proceed with MDO, a full surgical work-up is completed. This involves simulating the surgery with three-dimensional planning (3D Systems Medical Devices, Littleton, Colorado, USA), as seen in Fig. 1. The vectors and magnitude of advancement are evaluated, distractor length of the distractor and type are chosen and surgical marking guides and anatomical models are fabricated. (Fig. 2) The surgical technique involves a corticotomy-osteotomy in the mandible based on 3D planning. At our center we use an internal MDO device (Stryker or KLS Martin) to perform the osteodistraction. The activation pins that turn the osteodistraction device can be placed through the cutaneous layer, either in an anterior or posterior mandibular position.
Fig. 1A
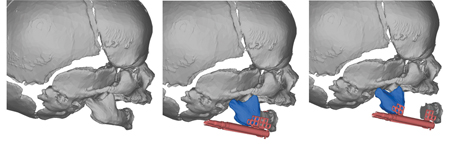
Fig. 1B
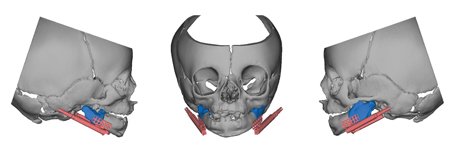
Fig. 2A
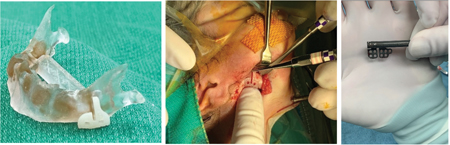
Fig. 2B
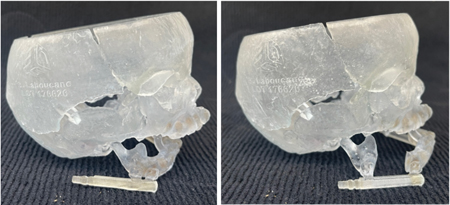
Postoperatively, following a latency phase of 3-4 days, the distractor is activated and the forces are applied to the fibro-vascular bridge gradually at a rate of 2-3mm per day until sufficient mandibular advancement is achieved. This position is decided both from the planning and clinically, based on the patient’s chin position and alveolar ridge relationship. Following the distraction phase, the activation arms are removed and the consolidation phase begins, usually lasting 3-4 months. Once the bone is consolidated and bony microcolumns have formed between the segments, an intra-operative CT scan is taken to ensure adequate consolidation, and the subcutaneous/submucosal distraction device is removed through the same extra-oral incision.
Case 1:
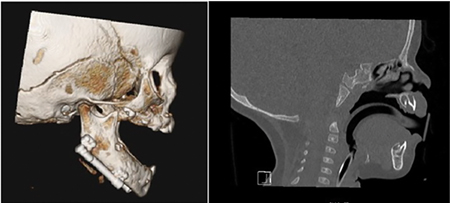
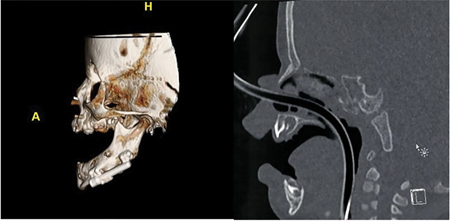
An 8-week-old male PRS patient with the clinical signs of a hypoplastic mandible including the typical “bird- face” presentation and severe airway obstruction and associated hypoxia. (Fig. 3A) The patient presents with poor mandibular position and retruded tongue position with severely compromised airway. The surgical procedure for placement and removal of the appliance is demonstrated in Fig. 3B. CT scans were taken both pre-operatively (Fig. 3C) and post-operatively (Fig. 3D) where new bone formation can be seen between the bony segments. On the pre-operative scan, the patient presents with a very short mandible from symphysis to mandibular angle, and a significant radiographic overjet. Radiographically, due to insufficient mandibular space, the tongue is forced into the oropharyngeal airspace. Post-operatively, we see a significant mandibular advancement with a more harmonious relationship to the maxilla and excellent new bone formation. The tongue is afforded a more anterior position and a notable increase in the oropharyngeal airspace is seen. The surgery has changed the lateral facial profile of the infant from convex to mesognathic. (Fig. 3A) The patient was extubated uneventfully, no post-operative complications occurred; healing was uneventful.
Fig. 3A

Fig. 3B
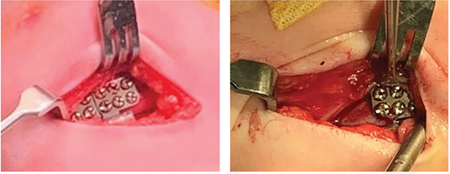
Fig. 3C

Fig. 3D
Case 2:
A 6-week-old male neonate with PRS is shown in Fig. 4 who demonstrates a significant anterior mandibular advancement post-MDO, both clinically and radiographically. A significantly improved retroglossal airway is also seen. In this case, the activation pins are position in an anterior position for easier access for distractor pin activation.
Fig. 4A
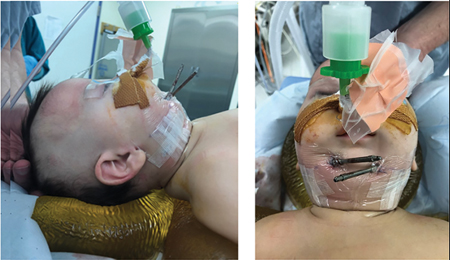
Fig. 4B

Fig. 4C
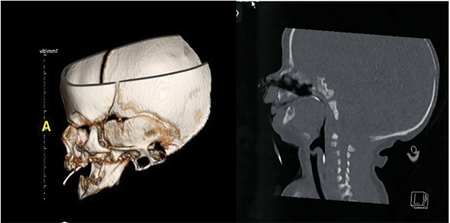
Fig. 4D
Case 3:
This case demonstrates progress records of neonate male. This 3-month-old patient presented with recurring hypoxia and a severely retrognathic mandible. MDO was completed and the patient was followed for growth and development. Follow-up at 6-year-old demonstrated sustainable airway and good mandibular growth and dental development. Figs. 5A, 5B & 5C demonstrated the initial presurgical clinical and radiographic findings and follow up at 6 years old.
Fig. 5A

Fig. 5B
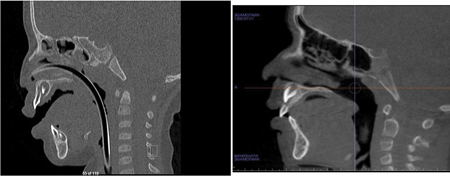
Fig. 5C

Case 4 and Case 5:
Figure 6 demonstrates again, two cases, 5-week-old female and 5-week-old male, with history of severe hypoxia requiring MDO. Both patients had noticeable improvement of mandibular position and resolution of OSA with the utilization of MDO.
Fig. 6A

Fig. 6B

Mandibular distraction osteogenesis is an effective surgical management for severe mandibular hypoplasia and obstructive airway. It relies on the principles of osteodistraction to incrementally lengthen the distance between segments of bone and encourage bone growth. MDO has had a major impact on craniofacial deformities, and is a life-changing procedure, both for neonates and young children.
Children with glossoptosis due to mandibular hypoplasia and a small oropharyngeal airway are likely to suffer from breathing problems, and consequently hypoxia and hypercarbia, growth delays, cognitive developmental issues, behavioral, neurological, concentration complications, difficulty thriving and performing, childhood obesity, and cardiopulmonary problems. MDO effectively and safely relieves the airway obstruction caused by glossoptosis,11 thereby improving long-term health outcomes. MDO has the advantage of increasing the boney growth’s post-operative stability by encouraging the growth of soft tissue as well.12 It allows for extensive bone lengthening and eliminates the need for bone grafting and obviates the need for tracheostomy.13
MDO can produce a significant and sustained anterior mandibular position and airway improvement, thus resolving OSA. As advancements continue to be made in the surgical appliances, more refinements in treatment can be achieved. Future designs of internal MDO appliances include ones capable of multi-vector osteodistraction and in patient-specific distractors. Despite the risks of the surgery, the outcome of MDO is life-altering for many children with severe OSA and significantly improves quality of life for patients and their families.
Oral Health welcomes this original article.
References
- Gangopadhyay N, Mendonca DA, Woo AS. Pierre Robin Sequence. Seminar of Plastic Surgery 2012;26(2):76-82.
- Flores RL. Neonatal mandibular distraction osteogenesis. Seminar Plastic Surgery 2014; 28(4):199-206
- De Bastiani G, Aldegheri R, Renzi-Brivio L, Trivella G. Limb lengthening by callus distraction (callostasis). Journal of Pediatric Orthopedics 1987;7(2):129-134.
- Breugem CC, Logjes RJH, Nolte JW, Flores RL. Advantages and disadvantages of mandibular distraction in Robin sequence. Seminars in Fetal and neonatal Medicine. 2021; 26(6): 101283.
- Brugem CC, Logjies RJH, Mermans JH, Paes EC, Muradin MSM, Don Griot JP. Assessment of health-related quality of life in robin sequence: a comparison of mandibular distraction osteogenesis and tongue-lip adhesion. Plastic Reconstruction Surgery 2019;143(5):1456-65.
- Sedaghat AR, Ching L, Anderson W, Ishman SL, Mcginley BM, Roosberg MI, Redett RJ. Characterization of Obstructive Sleep Apnea before and after tongue-lip Adhesion in Children with Micrognathia. The Cleft Palate Craniofacial Journal. 2012; 49(1):21-26.
- Verlinden CRA, Van de Vifeiken SECM, Jansma EP, Becking GRJ, Swennen J. Complications of mandibular distraction osteo- genesis for congenital deformities: a systematic review of the literature and proposal of a new classification for complications. Inter- national Journal of Oral Maxillofacial Surgery 2015; 44:37-43.
- Zhang RS, Hoppe IC, Taylor JA, Bartlett SP. Surgical management, and outcomes of Pierre Robin Sequence: a comparison of mandibular distraction osteogenesis and tongue-lip adhesion. Plastic Reconstruction Surgery 2018: 142(2):480-50.
- Resnick CM, Calabrese CE, Sahdev R, Padwa BL. Is Tongue-Lip Adhesion or Mandibular Distraction More Effective in Reliev- ing Obstructive Apnea in Infants with Robin Sequence? Journal of Oral Maxillofacial Surgery. 2019;77(3):591-600.
- Morrison KA, Collares MV, Flores RL. Robin Sequence Neonatal Mandibular Distraction. Clinical Plastic Surgery 2021;48: 363-373.
- Ren CX, Gao ZW, Li YF, Liu Y, Ye B, Zhu S. The effects of clinical factors on airway outcomes of mandibular distraction osteo- genesis in children with Pierre Robin sequence. International journal of Oral and Maxillofacial Surgery 2017; 46:805-810.
- Karun V, Agarwal N, Singh V. Distraction osteogenesis for correction of mandibular abnormalities. National Journal of Maxillofacial Surgery 2013;4(2): 206-213.
- El-Bialy TH, Razdolsky Y, Kravitz ND, Dessner S, Elgazzar RF. Long-term results of bilateral mandibular distraction osteogenesis using an intraoral tooth-borne device in adult Class II patients. International Journal of Oral Maxillofacial Surgery 2013;42(11):1446-1453.
About the Authors

Kevin E. Lung is a registered specialist in Oral and Maxillofacial Surgery who has practiced in Edmonton, Alberta with the group at Kingsway Oral and Maxillofacial Surgery in Edmonton, Alberta. He is the Lead, Pediatric Oral & Maxillofacial Surgery at the Stollery Children’s / University Hospital.

Matthew Fay is a registered specialist in Oral and Maxillofacial Surgery in Edmonton, Alberta, Canada who practices with the Kingsway Oral & Maxillofacial Surgery group.

Jason Adam is a Third Year Dental Student at the University of Alberta, with a prior Bachelor’s degree in Immunology Honours. He is currently serving as the President of the school’s Dentistry Students’ Association (DSA).









