Introduction:
The purpose of this case report is to illustrate the potential of utilizing digital technology to minimize surgical invasion and increase precision in management of compromised sites in the esthetic zone.
Article
In modern-day implant dentistry, the ability to achieve a harmonious integration of the implant restoration is no longer optional but to a commonly expected from our patients. This objective becomes even more demanding in patients with a high smile line and poor remaining alveolar bone structure, where bone augmentation procedures or almost any surgical intervention becomes visible when the patient smiles. Clinical situations where there is lack of tooth development or early tooth loss pose a challenge for the treating clinician. Particularly in cases of tooth agenesis, failure of the tooth bud to form can render the alveolar ridge topography inadequate for implant placement and demand more extensive bone augmentation procedures for adequate site development. These conditions are further complicated by sub-optimal spacing for the implant fixtures and obviously the final prosthetics. There are different treatment options for treatment of congenitally missing lateral incisors including but not limited to orthodontics, resin bonded bridges, removable of fixed partial dentures. However; in patients with a high smile line, esthetics becomes one of the major objectives to be fulfilled regardless of the treatment modality selected. This present case report aims to illustrate a minimally invasive, esthetically driven surgical approach for implant rehabilitation and guided bone augmentation in the esthetic zone.
Case Report:
A 41 year-old medically healthy female presented to our clinic complaining of food stagnation and mobility related to her maxillary anterior prosthesis. Following bridge removal, clinical and CBCT evaluations, 11 and 21 were deemed hopeless due to the severe coronal decay and compromise of the remaining alveolar bone support resulting from the long-standing peri-apical infections present. The patient additionally complained of unsatisfactory esthetics and tooth mis-proportions in her existing bridge which can be mainly be attributed to the lack of adequate restorative space resulting from the congenital absence of her maxillary lateral incisors and transposition of the maxillary canines. The patient declined undergoing any orthodontic treatment and a decision was made to address her esthetic concerns utilizing a prosthetic approach.
The inherent anatomy of the alveolar topography in the anterior zone, post-extraction ridge dimension alterations are more pronounced than in posterior segments. Tomographic studies have demonstrated that the average buccal bone thickness is less than 1 mm in 90% of anterior teeth. (Braut, Bornstein, Belser, & Buser, 2011). This is compounded by the fact that the buccal plate (bundle bone) stems from the periodontal ligament of the tooth and inevitably undergoes remodeling once the tooth is extracted. (M. Araujo, Linder, Wennström, & Lindhe, 2008; Araújo, Sukekava, Wennström, & Lindhe, 2006) demonstrated a 40% reduction in ridge width following tooth extractions in dogs. Similar findings in more recent literature (buser 2017) demonstrate the degree of ridge alterations following extraction of anterior dentition. The sequale of alveolar ridge remodeling if not addressed can often result in significant post-extraction ridge defect. Such conditions often require more invasive procedures to restore adequate ridge volume for both implant placement and/or pontic sites development to satisfy the biologic, functional and esthetic demands of the case. Subsequently, efforts to preserve existing ridge topography and tissue volume should be made at the time of tooth extraction. If residual deficiencies are still present, they can then be managed in a less invasive manner.
Fig. 1

Fig. 2

Extraction of 11 and 21:
Tooth extraction in such highly demanding cases must be performed in a minimally traumatic fashion. Avoiding flap elevation or papillary reflection is critical for maintaining the blood supply to the surrounding bone and preserving the soft tissue architecture. Although more restrictive in access, flapless procedures have been proven to yield esthetically superior results and enhanced soft tissue response around dental implants in the esthetic zone. The teeth are elevated with micro-luxating elevators and care is taken to avoid excessive pressure on the buccal plates during delivery of the roots. Following removal of 11 and 21, the sites were debrided thoroughly utilizing manual curettes and piezo ultrasonic instrumentation. Typically, the choice of grafting material for these cases is usually an allograft bone material with particle sizes between 250 and 500 microns. The key in soft tissue volume preservation of this case was that the graft was packed into the socket (bone zone) and extended to the level of the gingival margin (tissue zone). This dual zone fashion will ultimately lead to residual bone graft particles being encapsulated in the soft tissues, essentially acting as a filler for the peri-implant gingival tissues.
Fig. 3

Fig. 4

Fig. 5
Closure over the sockets:
During conventional tooth extraction procedures, spontaneous healing and epithelialization of the extraction site orifice usually occurs over a period of 3-5 weeks. However, when ridge preservation procedures are employed, the bone graft is left exposed to the oral cavity and is subjected to external contaminants and risk of early dislodgment. Therefore, a physical barrier may be beneficial for the simple purpose of protection and containment of the bone graft particles during the early phases of healing. The choice of a physical barrier may be prosthetic or a biologic material/tissue. In this case, a non-cross linked collagen barrier (colla-plug) was placed over the grafted site and the provisional bridge was relined with a highly polishable composite material to seal over the extraction site orifices. No sutures were utilized for this case due to the flapless nature of the procedure and prosthetic seal provided by the ovate pontics of the provisional bridge. It is important to note that a tooth-bourne provisional is preferred whenever possible to avoid excessive trauma and mobility during the early healing of the grafted site. Should a removable partial denture be utilized, care must be taken to avoid excessive pressure or buccal flange extension over the healing sockets. However; regardless of the material of choice for the provisional, the surface of the material should be highly polished and clean to allow an environment conducive to healing without excessive soft tissue irritation and plaque retention. If an implant is placed immediately in a fresh extraction socket with adequate stability, an implant-supported provisional or custom healing abutment may also be utilized to capture the pre-existing soft tissue contours. By performing early soft tissue preservation at the time of extraction, the clinician is able to expedite subsequent restorative procedures needed for soft tissue contouring and consequently decrease additional visits for the patient.
Following 5 months of healing, the patient expressed a strong desire to have the extracted teeth replaced with dental implants. Evaluation of the post-graft CBCT revealed an apical bone width deficiency, despite the ridge preservation efforts employed. The extent of the deficiency precluded the possibility of implant placement in a restoratively-driven position without additional bone grafting. However; despite its predictability in horizontal bone gain, conventional ridge augmentation procedures can often result in excessive scarring and soft tissue distortion that could potentially jeoparadize the final esthetic outcome of the case. Therefore an alternative was sought to address this localized deficiency in a limited fashion, utilizing a tunnel approach with incisions that were placed apical to the patient’s smile line.
Fig. 6
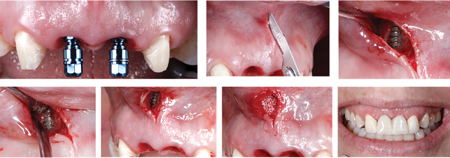
Fig. 7

Guided bone augmentation and implant placement
Guided surgery can offer the advantage of increased accuracy in implant placement, especially in cases where bone availability is sub-optimal or spacing is critical. Once the proposed implant positions were finalized based on the CBCT scan, a surgical guide was fabricated to accurately translate the proposed 3-D implant position to the patient’s mouth. The digital workflow additionally allowed the fabrication of an implant supported provisional restoration to be inserted the day of surgery. This high precision in pre-surgical planning offers both the clinician and patient increased predictability in approaching such cases. In this case, utilization of guided implant surgery was expanded to accurately pre-plan the extent and approach for the bone augmentation surgery.
Surgical Phase:
Prior to local anesthesia, the patient’s lip line is evaluated to assess the design and location of the future incision. The incision is performed to extend at least 3-4 mm away from the border of the anticipated defect. The surgery is extended sufficiently to facilitate visualization and instrumentation through the limited access. Following which, micro-surgical tunneling instruments are utilized to create a sub-periosteal tunnel access to the defect. One of the main advantages of this technique is the stability of the blood clot during the initial healing phases as no flaps have been reflected. Therefore, extension of the tunnel should be performed only to accommodate for the augmentation volume and excessive reflection should be avoided. A collagen membrane was then trimmed to cover 3-4 mm surrounding the dehiscence defect and surrounding defect. Following introduction of the membrane into the site, an allograft bone material hydrated in growth factors was added to cover the exposed implant surface. The use of finger pressure can be applied from the outer surface of the flap to mold the bone graft to the desired contour. Closure over the tunnel augmentation is simplified as no periosteal releasing incisions are necessary to obtain primary closure. The area was then sutured with micro-sutures 6-0 prolene (hu-friedy) with a fine micro-surgical needle.
Immediate implant provisionalization of both implants was then performed to maintain the soft tissue scallop around the healing implants and help shape the maturing tissues during the healing
period. Adjustments to the provisional sub-gingival contours are then performed following implant integration to optimize the gingival zeniths of both centrals and replicate the desired inciso-gingival length of the teeth based on the pre-operative diagnostic plan. During the healing period, flapless piezo-assisted crown lengthening was performed on all maxillary bicuspids to further harmonize the gingival margins between the canines and adjacent dentition.
Final delivery of the case was done followed 6 months of healing post-implant placement with a combination of feldspathic porcelain veneers on the maxillary bicuspids bi-laterally, full coverage crowns on 13 and 23 and implant supported crowns on 11 and 21.
Fig. 8

Fig. 9

Conclusion
Pre-surgical planning for implant placement in the esthetic zone is critical for functional and esthetic success. Diagnostic wax-ups, accurate records and 3-D imaging are fundamental components for clinicians to assess the site and determine the feasibility for implant placement. This case reports illustrates how the addition of digital planning and guided surgical execution to our conventional procedures can now offer our patients solutions with limited surgical extent and subsequent morbidity, while offering them a high level of esthetics and comfort.
Oral Health welcomes this original article.
About the Author
 Dr. Sherif Said completed his post-doctoral training in periodontics at Boston University in 2016, with a special focus on growth factors and peri-implant tissue development. To maintain his teaching and research interests, Dr. Said currently maintains a clinical assistant professor position in the post-doctoral periodontology department at Boston University as well as private practice in Toronto. Dr. Said lectures both locally and in the United States and is maintaining both positions in private practice and academia in the fields of Periodontics & Implant Reconstructive Dentistry. Dr. Said has published peer reviewed articles and book chapters on the topics of anterior implant aesthetics.
Dr. Sherif Said completed his post-doctoral training in periodontics at Boston University in 2016, with a special focus on growth factors and peri-implant tissue development. To maintain his teaching and research interests, Dr. Said currently maintains a clinical assistant professor position in the post-doctoral periodontology department at Boston University as well as private practice in Toronto. Dr. Said lectures both locally and in the United States and is maintaining both positions in private practice and academia in the fields of Periodontics & Implant Reconstructive Dentistry. Dr. Said has published peer reviewed articles and book chapters on the topics of anterior implant aesthetics.













