Robotic guidance has enhanced and improved various surgical specialties and is now available to implant dentistry for both partially and fully edentulous patients through the Yomi platform developed by Neocis Inc. (Miami FL)1,2 Accuracy of implant placement has been shown to have a direct correlation with the prosthetic results.3 The Yomi platform provides visual, audio and haptic guidance during both the osteotomy phase and the placement of the implant. (Haptic feedback – the robotic arm physically guides the location, angulation, and depth of the surgical instruments according to the pre-operative virtual plan while the dentist supports and activates the handpiece). This guidance improves accuracy in position and angulation while protecting critical nerve structures, minimizing risk of alveolar bone perforations and inadvertent sinus penetration.
Static stacked guides can provide accuracy,4,5 but robotic guidance offers additional benefits. The robotic guidance is based on a pre-operative CBCT and a digital treatment plan, but the clinician retains the ability to modify the plan intra-operatively. Additionally, the elimination of the physical, fabricated guide enhances intraoral visibility, surgical site access, and adequate irrigation. Finally, digitally-planned, robotically-executed implant placement encourages flapless surgery. Flapless surgery has been found to result in less bone loss, decreased patient pain, and thus, less need for analgesics.6
CASE REPORT
A 60-year-old male with a history of previous extractions presented with failed upper and lower dentures (Figs. 1a & 1b). The treatment plan called for complete reconstruction of the edentulous mandible with 6 implants. The case was originally scheduled to be completed with a stackable guided system (laboratory costs more than $7,000). After the guides were ordered, but before the case could proceed, the patient suffered a heart attack, postponing the procedure for 6 months. At that time, the guide no longer fit the patient, and the manufacturer would neither guarantee accuracy nor provide the STL planning files to make changes; this resulted in a complete loss of the earlier efforts. It was then decided to opt for robotic placement.
Fig. 1a

Fig. 1b

The new treatment plan consisted of six implants at the areas of teeth 36, 34, 32, 42, 44 and 46 using flapless MIS protocol with local anesthesia and oral sedation only (now preferred due to the cardiac event).
The Yomi robotic system consists of a planning station, the robotic guidance arm and the patient tracker arm. It fits easily in a standard dental operatory. (Fig. 2) A CBCT scan is taken either prior to, or on the day of, surgery. The treatment plan is developed with this data. (Fig. 3) The software offers three-dimensional (3D) treatment planning, including identification of nerve and blood vessel structures, and may be modified during the procedure. Scanning and planning at the patient’s initial consult keeps implant inventory requirements to a minimum.
Fig. 2

Fig. 3

An edentulous bone-mounted splint was then attached using five self-tapping, monocortical bone screws (Stryker, 2.0 x 18mm, Kalamazoo MI) without any tissue reflection. (Fig. 4a) This splint was placed with local anesthesia in the buccal and lingual. A fiducial array containing radiopaque spheres was then rigidly attached to the splint, (Fig. 4b) and another CBCT scan was taken. The fiducial array was removed from the splint and replaced by the patient tracker arm. (Fig. 4c) The tracker arm registers the patient frame of reference and the robot to the treatment plan, allowing dynamic, real-time tracking of patient movement. The weight of the tracker is compensated such that, in effect, it is weightless to the patient.
Fig. 4a

Fig. 4b

Fig. 4c

All the osteotomies were flapless, without guides or extended drill sleeves. (Fig. 5) The Yomi robotic control guided the location, angulation and depth of each osteotomy. In addition to this physical haptic guidance, the system also provided visual guidance and audible feedback throughout the procedure (Fig. 6). The physical guidance was critical as the bony ridge had a very narrow crest, and the anterior mandible was narrow. The haptic robotic arm minimized risk of skiving. Typically, bone reduction and leveling is used to reduce skiving, but cannot be done without flap surgery. Robotic surgery minimizes risk of skiving and permits flapless procedures. The Yomi eliminates the use of elongated drills necessary for stacked guides.
Fig. 5

Fig. 6

Following the osteotomies, all implants were placed under similar robotic guidance, controlling location, angulation, and depth. (Fig. 7). Six implants were placed: 36: 5.8x9mm; 34: 3.0x12mm; 32: 3.0x12mm; 42: 3.0x12mm; 44: 3.9x12mm; 46: 3.8x9mm. During the planning phase, the Yomi software warned that the bone at site 46 was insufficient (based on the Hounsfield units from the CBCT scan). The osteotomy and implant proceeded as planned despite this alert. During placement of the site 46 abutment, the implant spun out. The implant was removed, replanned, redrilled mesially, and reimplanted.
Fig. 7

Robotic dental ergonomics are very beneficial to the clinician. The robotic arm end effector is virtually weightless in the operator’s hand, allowing the forearm, elbow, wrist and neck to remain relaxed. Three-dimensional visualization also obviates the need to assume awkward body positions for intraoral visual access.
Following implantation, the bone-mounted splint was removed. The post-operative intraoral view clearly shows that even considering the slight bony reduction needed for 6 abutments, only very conservative envelope incisions were required to access the crest. (Figs. 8a & 8b) The post-operative scan shows the position of the final position of the implants (Fig. 9b) relative to the original treatment plan. (Fig. 9a)
Fig. 8a
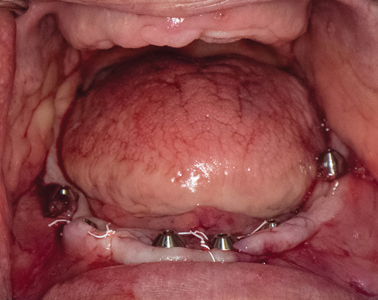
Fig. 8b

Fig. 9a
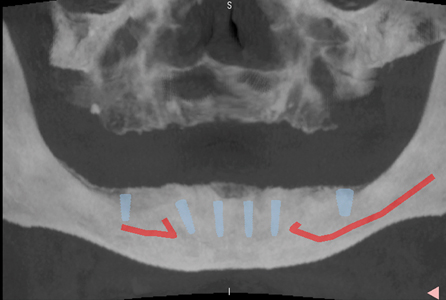
Fig. 9b

The post-operative CBCT scan was taken to assess the accuracy of implant placement. This technique uses a standardized 3D voxel-based registration of the superimposed volumetric images of the implant plan and the post-op scan. Deviations were measured between each planned and actual implant locations according to the International Team for Implantology (TTI) consensus report. Accuracy data is reported in terms of the following metrics:
- Global angular deviation in degrees (α) – the 3D angle between the central axis of the planned and actual implants.
- Signed depth deviation in mm (sd) – the difference in the coronal depth of the planned and actual implants along the long axis of the planned
implant. Positive values indicate the actual placement is “proud” of the plan. - Global coronal deviation in mm (c) – the 3D distance between the coronal centers of the planned and actual implant positions.
- Global apical deviation in mm (a) – the 3D distance between the apical centers of the planned and actual implant positions.
Table 1 shows the average implant deviations of 5 of the 6 implants for this case. The implant at site 46 was not evaluated as this implant position was changed due to poor bone quality at the intended site. The global angular deviation averaged 1.12 ± 1.26° with 95% confidence limits of 0.01° and 2.23°. The signed depth deviation averaged 0.13 ± 0.39mm proud. The crown and the apex of the final placed implants showed an average deviation from the plan of 1.19 ± 0.52mm and 1.22 ± 0.67mm, respectively.
Table 1
DISCUSSION
Advances in 3D digital dentistry have facilitated the progression of dental implant surgery to robotic guidance, providing significant value to both patient and clinician. This predictable treatment of a fully edentulous case demonstrates that dental robotics can be readily implemented into the general dentistry practice. With robotic 3D visualization and haptic guidance, accurate full arch procedures can be minimally invasive, even when the bony crests are thin. The ergonomics of robotic treatment are less biomechanically stressful on the clinician.
Oral Health welcomes this original article.
References
S. Rawal, D. E. Tillery, and P. Brewer, “Robotic-Assisted Prosthetically Driven Planning and Immediate Placement of a Dental Implant,” Compend. Contin. Educ. Dent. Jamesburg NJ 1995, vol. 41, no. 1, Art. no. 1, Jan. 2020.
S. L. Bolding and U. N. Reebye, “Accuracy of haptic robotic guidance of dental implant surgery for completely edentulous arches,” J. Prosthet. Dent., vol. 0, no. 0, Mar. 2021, doi: 10.1016/j.prosdent.2020.12.048.
T. Kosinski, “Proper Preparation for Prosthetically Driven Implants: CBCT Diagnosing and Surgical Protocol,” Dent. Today, vol. 36, no. 6, pp. 56-59, Dec. 2017.
A. Tahmaseb, V. Wu, D. Wismeijer, W. Coucke, and C. Evans, “The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis,” Clin. Oral Implants Res., vol. 29 Suppl 16, pp. 416-435, Oct. 2018, doi: 10.1111/clr.13346.
J. D’haese, T. Van De Velde, L. Elaut, and H. De Bruyn, “A prospective study on the accuracy of mucosally supported stereolithographic surgical guides in fully edentulous maxillae,” Clin. Implant Dent. Relat. Res., vol. 14, no. 2, Art. no. 2, Apr. 2012, doi: 10.1111/j.1708-8208.2009.00255.x.
T. K. Divakar, S. Gidean Arularasan, M. Baskaran, I. Packiaraj, and N. Dhineksh Kumar, “Clinical Evaluation of Placement of Implant by Flapless Technique Over Conventional
Flap Technique,” J. Maxillofac. Oral Surg., vol. 19, no. 1, pp. 74-84, Mar. 2020, doi: 10.1007/s12663-019-
01218-9.
About the Author
 Dr. Griffin received his doctorate in dental surgery from UT-Memphis and did his residency in conscious sedation at the University of Alabama at Birmingham. Dr. Griffin has extensive specialized training in implant fixture placement and advanced bone grafting procedures and also has his ACLS certification and oral and intravenous sedation certification.
Dr. Griffin received his doctorate in dental surgery from UT-Memphis and did his residency in conscious sedation at the University of Alabama at Birmingham. Dr. Griffin has extensive specialized training in implant fixture placement and advanced bone grafting procedures and also has his ACLS certification and oral and intravenous sedation certification.
RELATED ARTICLE: Robotically-Guided Dental Implant Placement: Extending Surgical Expertise













