The efficacy of fluoride varnish in the prevention of dental caries, remineralization of tooth surfaces and treatment of dentin hypersensitivity is well supported by literature.
Varnishes allow for the delivery of high concentrations of fluoride in small amounts. Furthermore, the effectiveness, the relative safety, the uptake of this form of delivery combined with its ease of application offer significant advantages over other professionally-applied topical fluoride treatments like fluoride gels, foams, and mouthrinses.
The first fluoride varnish was marketed in 1964 under the trade name Duraphat. This new form of delivery for topical fluoride was created in order to have a fluoride vehicle that would ensure a longer contact time between the fluoride itself and the tooth surface in order for the treated areas to become more resistant.
Fluoride varnish is composed of a high concentration of sodium fluoride in a fast-drying alcohol and resin-based solution. Currently most varnishes on the market include 5% sodium fluoride (NaF) which equals to 2.26% fluoride by weight (or 22.6 mg fluoride/ml or 22,600 ppm fluoride). To ensure the varnish is sticky and adheres to the tooth surface, most products use a resin-based additive such as colophony (rosin derived from pine tree sap). The Contact Allergen Database defines colophony as a sticky, amber material distilled from the sap of pine trees that can be found in a wide variety of products including but not limited to, cosmetics, adhesives, cements, waxes, and fluoride varnishes. An hypersensitivity to rosin would appear as a localized contact dermatitis that would tend to occur at contact or 1 to 3 days later. Some clients treated with a colophony-based fluoride varnish could potentially develop an allergic response to pine. Acting as a vehicle for the fluoride agent, the resin also delays the bioavailability of the fluoride and does not allow the application of a truly fine coat of varnish on the client’s teeth. A major complaint from clients is that the film thickness is detectable, unpleasant and with pedo clients especially, it may be uncomfortable or an unwanted treatment option. Furthermore, the film could also be removed prematurely either voluntarily or involuntarily because of increased friction. It is also important to note that fluoride varnishes need the presence of saliva to either help with the precipitation of the fluoride, the dispersion of the fluoride and/or the crystallization process of the varnish on the teeth.
When looking at the efficacy of fluoride varnishes, Petersson, in 1997, demonstrated the significant caries reducing potential of fluoride varnishes which was also reiterated by many other researchers since then. Also, numerous in vivo and in vitro studies have shown that fluoride varnish is able to supply fluoride more efficiently to the enamel when compared to other topical fluoride agents, and is able to reduce considerably the incidence of dental caries. The Cochrane Review on the efficacy of fluoride varnishes published in 2013 concluded that young people treated with fluoride varnish experienced on average a 43% reduction in DMFT (decayed, missed, filled tooth surfaces), and in 10 trials looking at the effect of fluoride varnish on baby teeth, the evidence suggested a reduction on average of 37% in DMFT. Even if the level of evidence was rated as moderate because of the bias and the heterogeneity of the studies retained, the Cochrane review is the highest level of evidence we have on the efficacy of fluoride varnishes. Guidelines published by the American Dental Association recommends in-office application of fluoride varnish every three to six months for clients at moderate and high risk for dental caries.
As stated previously, most fluoride varnishes on the market have a concentration of 5% NaF. In 1988, SeppК investigated the effects of one sodium fluoride solution and a varnish with two different fluoride concentrations on enamel remineralization in vitro. It is important to understand that the effectiveness of a topical fluoride is primarily a function of the amount of fluoride uptake that can be achieved in demineralized areas. Fluoride uptake is affected by the concentration of fluoride in the agent, the contact time, and the ability of the product to induce the migration of the fluoride into the tooth structure. The results of this study suggested that the efficacy of the fluoride varnish was not proportional to the fluoride concentration (2.26% F varnish versus 1.13% F varnish, fluoride by weight which equates to 5% NaF and 2.5% NaF, respectively), but rather the number of applications. In this study, a 5% NaF varnish applied three times within a week was slightly more effective in enamel remineralization than a 2.5% NaF varnish, but no significant difference was found between one application of 5% NaF or one or three applications of 2.5% NaF varnish. The 0.1% NaF solution was the least effective when compared to the two different fluoride concentrations in the varnish form. Furthermore, enamel treated three times within a week with a 2.5% NaF varnish showed the greatest acid resistance when subjected to a 1-hour demineralization treatment. This study suggests that not fluoride concentration but number of applications may yield better enamel remineralization and protection, and that initial enamel fluoride saturation was fairly equivalent at both concentrations. SeppК et al, in 1994, did a similar trial using different concentrations of sodium fluoride in varnishes and assessed the caries preventive effect and found similar conclusions to the 1988 study; whereas the difference between a 1.1% F or a 2.3% F varnish was minimal on 274 children aged 12 to 14 years old who received 3 annual applications of either one concentration or the other, over a period of 3 years. Ahmed et al, in 2013, also concluded in an in vitro study that a concentration of 2.5% NaF is an optimal concentration of fluoride to obtain the saturation of tight and loose binding sites on hydroxyapatite discs. These studies suggest that a varnish with a concentration of 2.5% NaF is sufficient to achieve anti-caries protection without any risk for dental fluorosis, if this is a concern of the clinician, especially in young children.
With that information in hand, why not rethink your product selection to include a fluoride varnish that offers great benefits for the clinician and the client at-risk for dental caries or erosion? The unique formulation of Fluorimax™ includes a 2.5% NaF (11,300 ppm F) concentration that has been proven to be effective in enamel remineralization and protection of the dentition against acid erosion, and have shown to provide superior fluoride uptake when compared to traditional colophony-based varnishes (Figure 1). Furthermore, Fluorimax™ is a hypoallergenic solution that does not use colophony but a colorless dewaxed food-grade shellac to which they added hydroxyapatite, that will act as the driver of the fluoride. It provides the clinician assurance of no potential allergic reaction, and the ease of use, because of its liquid form, allows for an increased bioavailability of the fluoride and a low film thickness. With this fluoride varnish, the clinician can apply a very thin coat that flows easily into the interproximal areas, dries quickly and leaves a smooth clear coat on the client’s teeth. With its superior fluoride release and fluoride intake (Figure 2), this new varnish may revolutionize the way we choose our professionally-applied topical anticariogenic agents.
Figure 1

Better Fluoride Release (Availability) (EFU as % of total theoretical fluoride release in formula)
FluoriMax delivers 58% more fluoride uptake than 3M Vanish.
Source: Final Report: Enamel Fluoride Uptake Study Number 28 FDA, Method #40, Therametric Technologies, Inc., 2015.
Figure 2
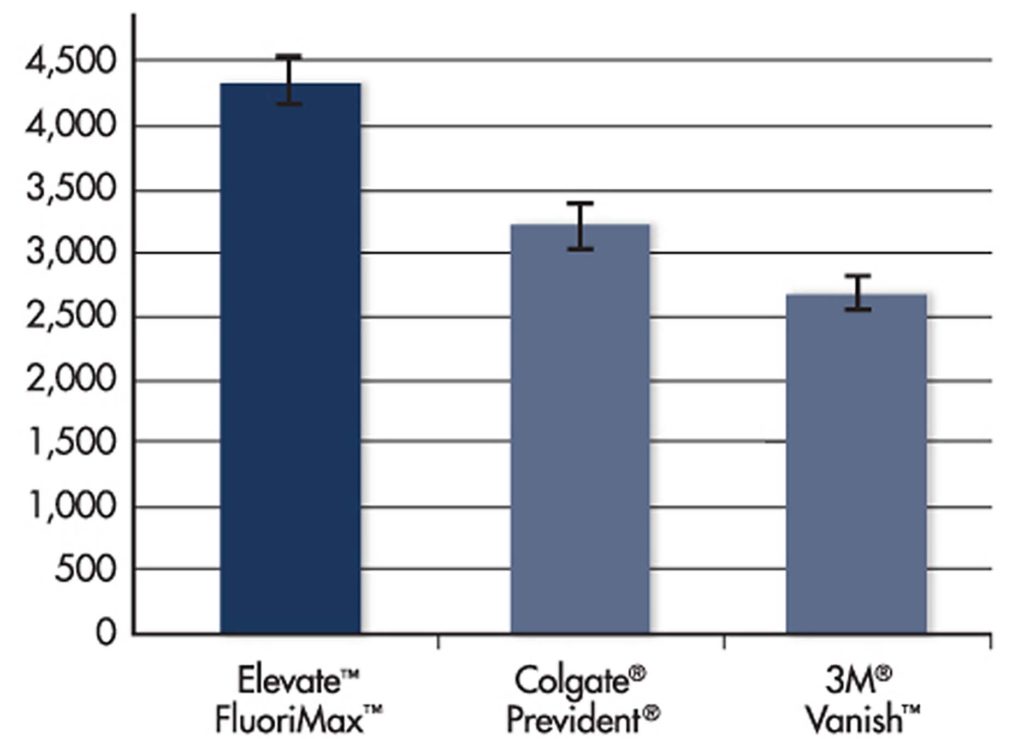
Better Fluoride Uptake (Absorption) (PPM, μg de F /g varnish)
With FluoriMax™, approximately 40% of the fluoride goes to the teeth.
Source: Final Report: Enamel Fluoride Uptake Study Number 28 FDA, Method #40, Therametric Technologies, Inc., 2015.
Fluorimax™ is a new option – an easy to use fluoride varnish without colophony, that flows well, adheres firmly to tooth surfaces, dries quickly, requires only a small amount of product to cover the entire dentition thus reducing the risk of ingestion of too much fluoride and any side effects associated with this behaviour, and is effective and safe to use with clients of all age groups.
In conclusion, dental professionals are responsible to keep abreast of the latest evidence that will guide how they customize their clients’ treatment plan. Fluoride varnish is a very important option to recommend for caries and sensitivity management in your practice. It has a proven record! Are you using it to its full potential?
DISCLOSURE
Sylvie Martel is an independent dental hygienist consultant and key opinion leader for a number of leading dental corporations and has received financial compensation from Oral Science for writing this article.
REFERENCES
- ADA Council on Scientific Affairs, Topical fluoride for caries prevention: A systematic review and evidence-based recommendations, 2013, ADA Center for Evidence-based dentistry.
https://ebd.ada.org/~/media/EBD/Files/Topical_fluoride_for_caries_prevention_2013_update.ashx - Ahmed I, Coleman SS, Carey CM, Fluoride release and uptake into hydroxyapatite from experimental dental varnish, March 2013. Paper presented at IADR 2014.
- Azarpazooh A, Main PA, Fluoride Varnish in the Prevention of Dental Caries in Children and Adolescents: A Systematic Review, J Can Dent Assoc 2008;74 (1), 73-79.
https://www.cda-adc.ca/jcda/vol-74/issue-1/73.pdf - Chu CH, Lo E, Uses of sodium fluoride varnish in dental practice. Ann R Australas Coll Dent Surg., 2008 Jun; 19:58-61.
- Contact Allergen Database on Colophony: www.contactallergy.com accessed on February 06, 2017.
- Final report: Enamel fluoride uptake study number 28 FDA, Method #40, Therametric Technologies Inc., 2015.
- Hoang-Dao BT, Hoang-Tu H, Tran-Thi NH,
Koubi G, Camps J, About I, Clinical efficacy of a natural resin fluoride varnish (Shellac F) in reducing dentin hypersensitivity, J Oral Rehabil 2009 Feb;36(2):124-131. - Marinho VCC, Worthington HV, Walsh T, Clarkson JE, Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No.: CD002279.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002279.pub2/pdf/standard - Petersson LG, On topical application of fluorides and its inhibiting effect on caries, Odontol Revy Suppl. 1975;34:1-36.
- Seppä L, Effects of sodium fluoride concentrations on enamel remineralization in vitro. Scand J Dent Res 1988;96:304-309.
- Seppä L, Pöllänen L, Hausen H, Caries preventive effect of fluoride varnish applications with different fluoride concentrations. Caries Research 1994;28:64-67.
- Stookey GK, Caries prevention, J Dent Educ., 1998 oct;62(10):803-811.
- Weyant RJ, Tracy SL, Anselmo T, et al. Topical fluoride for caries prevention. Executive summary of the updated clinical recommendations and supporting systematic review. J Am Dent Assoc. 2013; 144: 1279-1291.
 Sylvie is a seasoned international speaker, entrepreneur and educator. She works in close collaboration with the corporate sector as a lecturer, key opinion leader, trainer, writer and education specialist. She is the dental hygiene advisor for the National Dental Hygiene Certification Board of Canada, she sits on the board of the Commission on Dental Accreditation of Canada, and works as a consultant for certain dental hygiene regulatory bodies in Canada.
Sylvie is a seasoned international speaker, entrepreneur and educator. She works in close collaboration with the corporate sector as a lecturer, key opinion leader, trainer, writer and education specialist. She is the dental hygiene advisor for the National Dental Hygiene Certification Board of Canada, she sits on the board of the Commission on Dental Accreditation of Canada, and works as a consultant for certain dental hygiene regulatory bodies in Canada.












