On October 12th 2019, the Oral and Maxillofacial Surgery program at the University of Toronto’s Faculty of Dentistry embarked on its first mission to Addis Ababa University in Ethiopia. The goal of this mission was not only to provide direct care to patients in need, but also to provide an opportunity for the education of local surgical residents. Through this two-week long initiative, a variety of complex cases were treated, and unique local challenges were encountered providing great insight into what local surgeons face daily. The authors that participated in the endeavor were joined by both Dr. Dan Haas (Dean of the faculty of Dentistry at University of Toronto) and Dr. Peter Adamson (Director of Face the Future Foundation; Professor of Otolaryngology – Head and Neck Surgery, University of Toronto) (Image 1).
Image 1

The Addis Ababa University (AAU) has a newly formed OMFS program, first under direction of Dr Girma and now with the talents of Dr Demerew. Its first residents are set to complete their training in the Spring of 2020 (Image 2,3). Despite its novelty, Dr. Demerew has effectively secured operating room time for its residents, having a resident training structure and ensuring responsibilities like those found in a North American institution.
Image 2

Image 3

This mission was possible thanks to the organization and support of many individuals and was only possible through collaboration with the Toronto Addis Ababa Academic Collaborative (TAAAC) and Face the Future Foundation (FFF). With this being the University of Toronto OMFS’s first mission to Addis, a tremendous amount of organization and support was required in order to lay the groundwork and secure the necessary resources for this mission. Communications and connections were established early with both Dr. Adamson, the President of the FFF, and Dr. Wondwossen, the former Dean of the faculty of Dentistry at Addis Ababa University. Simultaneously, collaboration began with TAAAC and the OMFS team AAU under the direction of Dr. Demerew
and Dr Fasikawit the current Dean of the AAU Dental faculty. From a planning standpoint, there was a seamless development and execution due to the combined experiences of TAAAC with its knowledge of Ethiopian protocol and FFF with its knowledge of international surgical missions.
TAAAC became affiliated with the University of Toronto in 2003 and began as a psychiatric resident training program, focused on training Ethiopian residents in Ethiopia. With local training, TAAAC aimed to retain the brightest and most well-trained individuals in Ethiopia so that they could provide care to their communities and train the next generation of health practitioners. Thanks to the hard work of Dr. Clare Pain and Marci Rose as well as the administration from the Addis Ababa University, the TAAAC has helped train clinicians for many years and these practitioners can now be found providing patient care throughout the country. During the early stages of developing TAAAC, the local residents’ drive and desire to learn was noted by both Dr. Pane and Ms. Rose. Over the past 17 years, TAAAC has since expanded to include training missions in over 20 departments. There are faculty from the University of Toronto in Addis Ababa at almost all points in the year. With combined backing from Face the Future and TAAAC, OMFS is the newest department to be integrated into the care and training program! Dr. Pain and Marci Rose’s local knowledge, organization, and advice was invaluable in ensuring the mission had support from local practitioners.
A special mention must be made to Dr. Peter Adamson, and the Face the Future Foundation. The FFF is a non-profit medical humanitarian and educational foundation founded in 1996 by Dr. Peter Adamson. The organization has focused on surgical and medical care in developing nations across the globe, providing direct patient care to those in need, as well as assisting in the education of local residents as their core goals. Through firsthand experience from previous missions, Dr. Adamson noted the demand for Oral and Maxillofacial Surgical expertise in this patient population and was instrumental in facilitating this mission. Dr. Adamson’s visited Addis Ababa a year prior to the mission, liased with Drs. Girma and Demerew and helped to ensure that adequate operating room time was available to facilitate clinical care and training. Through the work of his foundation, as well as the generous funding provided, the University of Toronto OMFS department was able to make this trip a reality.
Dr. Demerew, the Program Director at AAU, must be credited for his hard work in organizing and managing our stay and activities (Image 4). Despite challenges in resource allocation, Drs. Demerew and Girma worked to ensure that the operating rooms were functional and auxillary staff were as prepared as possible throughout the mission. Additionally, Drs. Demerew and Girma kindly provided transportation for the majority of our trip and were gracious hosts, welcoming us for meals on numerous occasions throughout the trip. Dr Girma should also be commended for his presence and the calm voice of reason given the many clinical and surgical challenges we faced. We look forward to continuing our relationship with these two surgical educators and friends.
Image 4

(U of T OMFS Faculty), Dr. Demerew Dejene, Dr. Marco Caminiti, Dr. Michael Laschuk in front of St. Peter Specialized Hospital main entrance.
The two-week mission was divided into an initial two days of patient screening, with the remainder of the time reserved for surgical procedures. A total of 45 patients were screened, of which 16 patients were surgical candidates that received treatment at St Peters Specialized Hospital (Image 5) in the Northern Entoto District in Addis Ababa. Some patients presented with problems similar to those found in a North American clinic, such as craniofacial syndromes (Image 6A&B), benign and malignant pathologies of the maxillofacial region, and cleft lips (Image 7). Unique, region specific diseases/maxillofacial pathology encountered and managed included post traumatic deformity secondary to hyena bite (Images 8,9), a late stage lymphatic malformation restricting orbital movement (Image 10), facial nerve paralysis secondary to untreated Bell’s palsy requiring reanimation, TMJ ankylosis of children secondary to untreated simple fractures where no physiotherapy was performed, kerosene burns requiring regional flap rotations to correct scar contracture as well as other uncommon presentations in our health care system. Our surgical patient population ranged in age from 6 months to 28 years and included 9 females and 7 males. The surgeries consisted mostly of tumor resections, TMJ reconstructions with costochondral replacement, cleft lips, maxillectomy, mandibulectomy, regional flaps for fistulectomy, release of burn/scar contracture and numerous other procedures. There were no complications intra- or postoperatively in this specific population. Blood loss throughout was well controlled and no patients required transfusion, and all were discharged home safely.
Image 5

Image 6A

Image 6B

Image 7

Image 8

Image 9

Image 10

The St. Peters Specialized hospital was constructed in 2017. Many of the programs are in their infancy of development. Surgical equipment commonly used in North America was not often available. Equipment such as gas or electric powered saws and drills are in very limited supply or unavailable making any hard tissue surgery which requires osteotomies, extremely challenging. While many surgeons trained in the recent past may not be familiar with equipment such as the Gigli saw and hand powered drills, these instruments in combination with traditional osteotomes, were the primary equipment available for bony surgery performing bony surgery.
Patients in Addis are required to purchase their own supplies, including IV fluids, gauze, gloves, fixation, and tracheostomy tubes. Unfortunately, purchasing is often performed off-site without standardized in hospital pharmacies or vendors for the required materials. Reconstructive options were somewhat limited. One patient who required a segmental resection for a mandibular ameloblastoma was able to source stainless steel fixation prior to her surgery (Image 10,11). Other patients who lacked the financial means required alternative reconstructive options, and/or are unable to have bony reconstruction. As one can imagine, the lack of standardization of patients/laypeople in purchasing medical equipment creates challenges. One patient planned for bilateral TMJ ankylosis release purchased a size 7 tracheostomy tube (normal for a 40yo adult) but had previously received 2 prior tracheotomies. Fortunately, as this was the only trach tube available in the hospital, the trach tube was able to be fit into position, despite difficulty in fitting the oversized cannula. In the same patient case, two ribs were harvested. With no proper instrumentation available (no drill, no saws), the ankylotic bone mass had to be whittled away by hand. With no plates and screws available, the rib was fixated to the ramus using stainless steel wires. When the contralateral osteotomy was completed, it was discovered that the hospital supply of wires was depleted, and electrical wire had to be utilized to apply the rib to the ramus. As a result of these challenges we focused much of our care on soft tissue reconstruction. Procedures such as cleft lips repairs, the release of unrepaired burn contractures and regional pedicled flap reconstruction could be managed within reason utilizing the instruments available.
Image 11A

Image 11B
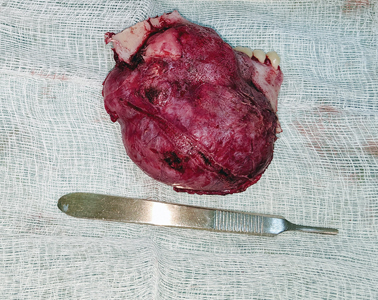
Image 11C

The ward care given the condition of the hospital (no running water, no dietary/nutrition attention, limited intravenous medications and 8 shared beds to a room without ventilation) was not what we experience in our hospitals, but it is the system that is accepted in this area. Due to high numbers of patients to nurses, family support was essential to help with wound care and post-operative recovery. When recalling our experiences with post-operative care, one patient stood out (Image 8). She did not speak the local language and was shunned from her tribe because of her deformity (kerosene burn at a young age). She travelled roughly 700 km on her own to seek care, staying outside of the hospital for nights prior to her surgical date. Post-operatively on the surgical ward, it was because of other patients’ families that she received some food and attention. It is the sense of community that is created in this hospital environment that brings these people together to help. They each recognized that the care in the hospital is unavailable and as a result they work together to help improve the situation.
There were many teaching opportunities available thanks to the organization through TAAAC, Dr. Haas and Dr. Adamson. The OMFS team was able to provide lectures to the local dental school focusing of trauma management. Most teaching took place in the operating room and at the patient’s bedside with the AAU OMFS residents always in tow, showing enthusiasm and a desire to learn. As any surgeon will report, these informal interactions are critical educational experiences in the progress towards developing competency. The residents kindly acknowledged our efforts to teach, and like their professors they gracious and invaluable hosts.
This article will hopefully shed some light on the educational opportunities that the OMFS community can provide for these resilient people and enthusiastic trainees. We plan to return for further engagements to Addis Ababa. Over the next few collaborations, we hope to establish diagnostic screening via videoconference prior to our arrival in order to facilitate treatment planning and operating room scheduling. With this strategy, we hope to be more efficient, and more equipped upon arrival with procedures planned for a portion of the mission. Given the resource limitations, specifically for bony surgery, we hope to arrange for an improved armamentarium including: drills, saws, osteotomes, rigid fixation plates, screws and reconstruction plates. We acknowledge the challenges in bringing and caring for new equipment at St. Peters Hospital and hope to work with the local hospital administrators to try to improve local purchasing and materials acquisition for the OMFS department at AAU. We have approached several companies to help with donation but most of the needs are met through corporate and personal donations (see Face the Future Foundation website). The country and hospital system suffer from a materials and personnel management deficiency that can only be overcome by an increase in education, surgical exposure, expertise, mentoring and importantly material support.
Finally, but formidably, the association with Face the Future Foundation (Dr. Adamson), TAAAC and Dr. Pain and Marci Rose was invaluable. The established TAAAC network and the connections they have secured with likeminded individuals at the AAU and with Dr Dawit (chief executive director, college of health sciences of Addis Ababa university) were critical to this mission’s success. Dr. Adamson’s experience in mission surgery, teaching in multiple foreign countries and working through resource limitations were apparent. Additionally, Dr. Adamson’s work to establish operating room resources and a link with the St. Peters Specialized hospital as well as Face the Future’s Norma Spall, who worked to co-ordinate travel and logistics for the trip were critical in our ability to focus on clinical care and teaching. Future endeavors to this region are planned with thanks in great part to the continued support and care from Face the Future and TAAAC. We express our immense gratitude to all these leaders.
Oral Health welcomes this original article.
Acknowledgements: Face the Future™ Foundation: https://www.facethefuturefoundation.ca/
The Toronto Addis Ababa Academic Collaboration (TAAAC) assists Ethiopians in identifying and implementing solutions to some of their nation’s most pressing challenges through training and education. taaac.com
https://taaac.com/toronto-addis-ababa-academic-collaboration
About the Author
 Dr. Michael Laschuk is a PGY4 Chief Resident in OMFS at the University of Toronto.
Dr. Michael Laschuk is a PGY4 Chief Resident in OMFS at the University of Toronto.
 Dr. Karl Cuddy is an Assistant Professor and Director of Education in the OMFS program at the University of Toronto.
Dr. Karl Cuddy is an Assistant Professor and Director of Education in the OMFS program at the University of Toronto.
 *Dr Marco Caminiti is an Assistant Professor, Head and Program Director of OMFS at the University of Toronto.
*Dr Marco Caminiti is an Assistant Professor, Head and Program Director of OMFS at the University of Toronto.
* Corresponding Author 124 Edward Street, Suite 145, Toronto, Ontario M5G1G6. www.omfsurgeryuoft.ca
To view more articles from the 2020 Oral Surgery issue of Oral Health, please click here.












