Abstract
Manual tooth preparation has not changed over the past few decades. However, new dental materials, minimal invasive dentistry techniques and new digital technologies can improve dental preparations to reduce common errors in clinical practice that are essential for the correct delivery of any restoration. The aim of this article is to present the basic principles of FIRSTFIT™ Technology with the advantages it has over traditional crown and bridge preparations. It describes the step by step procedure to prepare minimally invasive crowns and bridges in one appointment.
Introduction
Developments in routine dental practice, including prosthodontic treatments, are often driven by the introduction of new dental materials and processing technologies. Dental prostheses such as crowns, fixed partial dentures (FPDs), and removable dental prostheses are fabricated from a variety of dental materials using a range of dental laboratory processes (T. Miyazaki et al. 2013).
Traditional manual dental preparation is a complex clinical operation that is inefficient and difficult to control, leading to difficulties in dental training, clinical diagnosis, and treatment (Dai et al, 2016). The basic form of a preparation has not changed substantially over the years, despite the new materials that have their own demands with regard to the details of the preparation’s geometry (Podhorsky A, et al 2015; Wyatt C, 2007).
During the past decade, new materials such as glass ceramics, poly-crystalline alumina, and zirconia-based ceramics have been successfully introduced into the clinic, along with new processing technology, i.e. computer-assisted fabrication systems [dental computer-assisted design/computer-assisted manufacturing (CAD/CAM)](T. Miyazaki et al. 2013).
The recent trend in restorative dentistry is the fabrication of prostheses with esthetic and functional requirements on one hand and preservation of sound tooth structure on the other (Doh, 2009). Dentists have a wide variety of options when selecting a material to fabricate a single-unit crown. The dentist’s choice and recommendation to the patient can depend on various factors such as tooth location, esthetics, patient desires, masticatory factors, and patient finances (Makhija, 2016). FIRST FIT technology appears to improve on the classical tooth preparation model for crowns and bridges.
The significant advance is to allow the clinician to prepare crowns and bridges in a predictably and efficiently by using preparations guides; the marginal seating is substantially improved in comparison to traditional preparations due to the elimination of common preparation errors (spiked finish lines, lipped margins) (Renne W et al, 2012).
The aim of this article is to describe the FIRST FIT technology and procedure in achieving a crown or bridge in one single appointment, without temporization (Fig. 1).
Fig. 1
FIRST FIT technology and procedure.

Description of the Technology
FIRST FIT technology was developed by Dr. Cyrus Tahmasebi based on the minimally invasive dentistry philosophy. It is an innovative method to prepare crowns and bridges using existing technologies.
Indications are: caries-damaged, fractured, endodontically-treated, discolored and poorly restored molars and premolars. If there are gingival caries, deep fractures (below the CEJ), misalgnments, and previously cemented crowns, then this technology is not indicated.
The main objectives of FIRST FIT are to provide function, esthetics, convenience, and comfort to the patient while meeting operator objectives: predictability, accuracy, function and convenience, quickly and predictably.
Common concerns in crown design and preparation: under- and over-preparation, inaccurate impressions, the need for the provisionalizations process, and changes in gingival tissue health between preparation and cementation. The traditional procedures of manual manufacturing are affected by error sources that are not controllable (Atzeni, 2012; Yoon, 2014; Tiu et al 2015). FIRST FIT technology minimizes these errors utilizing digital preparation design, step-by-step computer-guided dental preparation, no need for temporaries, and an excellent fit. It is a fast and easy method involving minimum chair time, dramatically improving practice productivity.
Description of the Procedure
The diagnosis appointment includes reviewing the indications and contraindications. A radiograph is essential to reveal adverse periodontal or endodontic conditions.
Traditional PVS or scanned digital impressions and a bite registration are taken and sent to the FIRST FIT laboratory, along with shade and characterization information.
Digital aid design (CAD) and custom software select the most ideal tooth preparation with better control over thickness, insertion pathway and marginal fit (Ng, 2014; Yoon, 2014). Tooth preparation design must satisfy esthetics, mechanics, the preparation process, service life, and other considerations (Dai, 2016). Once the design of the preparation is complete, the 3D guides are computer-designed and printed (Fig. 2).
Fig. 2
3D guides, computer-designed and printed.

Preparation guides create the FIRSTFIT precision as there is no possibility of preparing the tooth outside the designed limits. For a single crown, three guides are needed: buccal (Figs. 3-4), lingual (Fig. 5), and occlusal (Fig. 6); for a bridge, one guide can be used to prepare both interproximal boxes. Earlier versions of this technology needed five guides for a crown and two guides for a bridge (I Valerio, 2014). A duplicate set of guides is provided in case the original is damaged. The guides are custom-made for each patient.
Fig. 3
Buccal guide positioned on model.

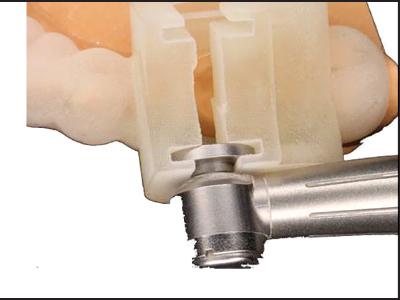
Fig. 4
Guided preparation of buccal surface.

Fig. 5
Lingual guide positioned on model.

Fig. 6
Occlusal guide positioned on model with handpiece.
The clinician is provided with the specific new bur which must be used for the preparation; it provides the precise finish line, shoulder, and axial wall angulations. A stone model is provided for the clinician who prefers to practice first and to confirm the intraoral preparation.
The crown or bridge are typically manufactured in zirconia (Y-TZP), in a 5-axis milling machine (Alghazzawi, 2016). Cementation follows the International Academy of Adhesive Dentistry (IAAD) protocols as described below:
1. Sandblast connectors with 50μ silica covered aluminium oxide particles.
2. Apply a primer or adhesive containing MDP (MDP adhesives must be light-cured).
3. Cement with warmed resin (at connectors, designed 0.5mm short, cover with resin)
4. Light cure for 40 seconds each from vestibular, lingual, and occlusal.
5. Avoid occlusal contacts, particularly in lateral movements.
Discussion
Traditionally, the clinician manually grinds the tooth to final preparation. Limited space in the patient’s mouth and operator visual bias can complicate manual control. To complicate
matters, all axial undercuts must be eliminated and the required degree of convergence achieved. These problems lead to decreased preparation accuracy and efficiency, and can seriously affect the quality of the fixed restoration (Dai et al, 2016; Tiu et al, 2015).
The prosthetic restoration of small edentulous spans poses a dilemma when the adjacent teeth do not require crowns. It is difficult to justify extensive reduction of the adjacent teeth to support a conventional fixed partial denture. A single-tooth implant is an alternative for willing patients with adequate bone (Wyatt, 2007). For patients where implants are not feasible, or where retention of the prosthesis can be achieved with minimal preparation of the abutment teeth, resin bonded fixed partial dentures (RBFPD) have offered a favorable option for restoring missing teeth. RBFPDs have undergone tremendous changes in terms of materials and designs since the 1970s (Arora, 2014, Doh 2009, Chen 2011).
Various bridge designs with varying claims for enhancing retention and resistance form have been proposed (Chen, 2011). The standard approach includes wings and occlusal rests on the abutments; other concepts include proximal slices, grooves, and extended occlusal coverage (Arora, 2014). Current RBFPD design, however, does not provide an adequate restorative lifespan (mean survival rate is 73.4% at 4.5 years). The most common failure mode was fiber-resin matrix interface delamination (Chen, 2011, Shi 2009).
Studies have indicated considerable tensile stress within the composite veneer, focusing at the pontic bottom and at the substructure interfaces near the abutments. Masticatory load can initiate fractures or chipping. The large discrepancies between the respective orientations of the maximum principal stress and fiber direction are responsable for the low efficiency in the box-shaped design (Shi, 2009). The FIRST FIT bridge retention is provided by two components: chemical retention of the zirconia with the MDP cement, and mechanical retention offered by the digitally designed axial wings closely adapted to the box walls. These proximal grooves significantly improve retention and resistance in RBFPDs as measured by dislodgment (Wyatt, 2007). If a bridge does fail for any reason, it can be readily restored. FIRST FIT bridges can be used as a long-term provisionals for patients waiting for implants.
Success in providing a dental patient with a quality dental prosthesis depends on multiple factors: the dentist, the laboratory technician and their relationship (Bin-Shuwaish, 2017). FIRST FIT technology decreases the laboratory steps, and there is less likelihood of error as long as the impressions, bite registration, and shade selection are aceptable.
FIRST FIT preparation requires a customized high-speed handpiece that is designed to engage grooves on the guide. The guides fit over the existing teeth without any patient discomfort. The provided tungsten carbide offers a smoother preparation Surface and less enamel fracturing. FIRST FIT technology does not depend on practitioners skills (Christensen, 2007; Yoon 2014); in fact, it guarantees that every tooth preparation has the appropriate convergence and no undercuts.
A missing first molar required replacement (Fig. 7). The patient refused an implant procedure, and the health of the two abutments contraindicated a full-preparation 3-unit bridge. After impressions and the fabrication of the single guide, the conservative preparation on the two abutments is shown (Fig. 8). The entire procedure with the provided preparation bur took only moments. The pre-fabricated FIRST FIT bridge (Fig. 9) was cemented into place (Fig. 10). The buccal appearance of the conservatively replaced restored tooth is consistent with aceptable esthetics (Fig. 11).
Fig. 7
Missing first molar.

Fig. 8
Conservative bridge preparation.
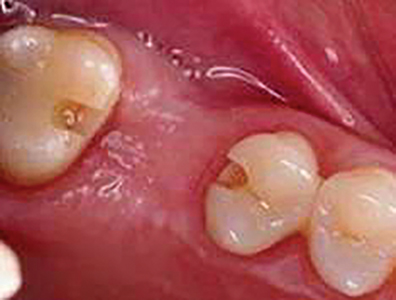
Fig. 9
Custom-made FIRST FIT bridge.

Fig. 10
FIRST FIT bridge cemented.

Fig. 11
Missing first molar restored to form and function.

Temporization is not required, reducing the risk of enamel fractures and microfractures (Frakenberger, 2011), and eliminating temporary faileures. The restoration is cemented immediately after preparation, thus it requires neither dentin sealing (Abu-Nawareg, 2015) nor preventive treatment to reduce postcementation hypersensitivity (Gupta, 2013, Hu 2010).
Three-dimensional modeling technology for customized tooth preparation is a key intermediate step in digitally preparing a full crown. However, the literature on the use of digital modeling technology for tooth preparation is sparse (Dai et al, 2016).
Traditional PVS and polyether impressions may be used, but scanned impressions are preferable. Tordiglione et al concluded that a full digital workflow enables the fabrication of clinically reliable restorations. Dai et al affirmed that digital modeling allows tooth preparation without undercuts to be predesigned, satisfying the parameters for precise adaptation.
FIRST FIT crowns and bridges are typically made of Zirconia which has high strength and toughness. There are many options for digital scanning and milling. This trend coincides with the shift in restorative material choice from metal to porcelain to all-zirconia, paralleling patient esthetic demands and the high cost of fabrication of metal-based crowns (Makhija, 2016).
Careful abutment selection, tooth preparation, crown material selection, and bonding technique are critical for clinical success (Wyatt, 2007). Conservative preparation leaves more enamel structure, contributing to a greater retention value when bonding with resin cements (Doh, 2009).
Further advances in tooth preparation include laser ablation. Short pulse laser cutting of dental hard tissue is more precise when digitally guided. These innovations will eventually permit automated digital tooth preparation (Dai, 2016). However, FIRST FIT technology is available and affordable now.
Conclusions
1. FIRST FIT technology represents an option for minimally invasive crown and bridge preparation
2. The digital design and preparations guides lead to a conservative, rapid and accurate preparation of crowns and bridges
3. With FIRST FIT technology, no temporaries are needed.
4. A zirconia crown or bridge can be prepared and delivered in one appointment. OH
Oral Health welcomes this original article.
Conflict of Interest Statement
The FIRST FIT crown and bridge that the author presented were provided by VIAX Dental Technologies.
Acknowledgments
The author wishes to thank to VIAX DENTAL LAB in Costa Rica for the technical support. Special thank to Dr. Delfin Barquero MSc of DaVinci’s Dental Care for his collaborative information in the cementation protocol.
References
1. Atzeni E et al. (2012) Proposal of an innovative benchmark for accuracy evaluation of dental crown manufacturing. Computers in Biology and Medicine 42: 548–555
2. Frakenberger R, et al. (2011) Chairside vs. labside ceramic inlays: Effect of temporary restoration and adhesive luting on enamel cracks and marginal integrity. Dental Materials 27: 892–898
3. Ng J, Ruse D, Wyatt C. (2014) A comparison of the marginal fit of crowns fabricated with digital and conventional methods. J Prosthet Dent 112(3):555-60
4. Renne W, McGill ST, Forshee KV, DeFee MR, Mennito AS. (2012) Predicting marginal fit of CAD/CAM crowns based on the presence or absence of common preparation errors. J Prosthet Dent 108(5): 310–315
5. Miyazaki T, Nakamura T, Matsumura H, Ban S, Kobayashi T. (2013). Current status of zirconia restoration. Journal of Prosthodontic Research 57: 236–261
6. Tordiglione, L., De Franco, M., & Bosetti, G. (2016). The Prosthetic Workflow in the Digital Era. International Journal of Dentistry, 2016, 9823025. http://doi.org/10.1155/2016/9823025
7. Wyatt C. Resin-Bonded Fixed Partial Dentures: What’s New? (2007) www.cda-adc.ca/jcda/vol-73/issue-10/933.html
8. Valerio I. FIRSTFIT ™: un sistema innovador de coronas y puentes en una sola cita, reporte de dos casos. Rev Cient Odontol (10) 2: 28-32, 2014
9. Arora V, Sharma M.C, Dwivedic R. (2014) Comparative evaluation of retentive properties of acid etched resin bonded fixed partial dentures. Med J Armed Forces India 70 (1): 53-57
10. Doh, R.-M., & Lee, K.-W. (2009). Dislodgement resistance of modified resin-bonded fixed partial dentures utilizing tooth undercuts: an in vitro study. The Journal of Advanced Prosthodontics, 1(2), 85–90
11. Soon S, Cheong C, Preisser J. Jr., Jun S, Chang BM, Wright RF. Measurement of total occlusal convergence of 3 different tooth preparations in 4 different planes by dental students (2014) Journal of Prosthetic Dentistry 112 ( 2): 285–292
12. Chen Y, Li H, Fok A. (2011) In vitro validation of a shape-optimized fiber-reinforced dental bridge. Dental Materials 27 : 1229–1237
13. Shi L, Fok A. (2009) Structural optimization of the fibre-reinforced composite substructure in a three-unit dental bridge. Dental Materials 25: 791–801
14. Bin-Shuwaish MS (2006) Compliance of dental laboratory technicians with dentists’ instructions for fabrication of a PFM crown, The Saudi Journal for Dental Research, http://dx.doi.org/10.1016/j.sjdr.2016.06.001 (article in press)
15. Makhija S.K et al. 2016. Dentist material selection for single-unit crowns: Findings from the National Dental Practice-Based Research Network. Journal of Dentistry 55: 40–47
16. Dai N, Zhong Y, Liu H, Yuan F, Sun Y. (2016) Digital modeling technology for full dental crown tooth preparation. Computers in Biology and Medicine 71: 190–197
17. Christensen GJ. (2007). Frequently encountered errors in tooth preparations for crowns.Journal of the American Dental Association 138 (10): 1373-1375
18. Tiu J, Al-Amleh B, Waddell JN, Duncan WJ. (2015) Clinical tooth preparations and associated measuring methods: A systematic review. J Prosthetic Dentistry 113 (3): 175-184
19. Abu-Nawareg, M. M., Zidan, A. Z., Zhou, J., Agee, K., Chiba, A., Tagami, J., & Pashley, D. H. (2015). Adhesive sealing of dentin surfaces in vitro: A review. American Journal of Dentistry, 28(6), 321–332.
20. Gupta N, Reddy UN, Vasundahar PL, Ramarao KS, Varma KP, Vinod V. (2013) Effectiveness of desensitizing agents in relieving the pre- and postcementation sensitivity for full coverage restorations: a clinical evaluation. J Contemp Dent Pract. 14 (5):858-65.
21. Hu J, Zhu Q. (2010). Effect of immediate dentin sealing on preventive treatment for posrtcementation hypersensitivity. Int J Prosthodont 23(1): 49-52
22. Alghazzawi TF (2016). Advancements in CAD/CAM technology: Options for practical implementation. Journal of Prosthodontic Research 60: 72–84
About the Author
 Dr Irene Valerio has practiced at Clinica Biblica Hospital, San José Costa Rica, 2007-2016. She earned her Masters in Operative Dentistry in 2008 and has been Professor at the Dental School of the Universidad de Costa Rica since 2014. Dr Valerio is an active volunteer in several charitable organizations and a consult-ant/external investigator for various dental companies.
Dr Irene Valerio has practiced at Clinica Biblica Hospital, San José Costa Rica, 2007-2016. She earned her Masters in Operative Dentistry in 2008 and has been Professor at the Dental School of the Universidad de Costa Rica since 2014. Dr Valerio is an active volunteer in several charitable organizations and a consult-ant/external investigator for various dental companies.
 Dr. Cyrus Tahmasebi is an international lecturer and trains dentists in the most advanced technologies associated with cosmetic dentistry as well as minimally invasive techniques. He is a Guest Lecturer at USC Dental School and serves on the Board of Directors, San Diego Dental Society. Dr. Tahmasebi is the Chief Scientific Officer and President of VIAX
Dr. Cyrus Tahmasebi is an international lecturer and trains dentists in the most advanced technologies associated with cosmetic dentistry as well as minimally invasive techniques. He is a Guest Lecturer at USC Dental School and serves on the Board of Directors, San Diego Dental Society. Dr. Tahmasebi is the Chief Scientific Officer and President of VIAX
technologies.
RELATED ARTICLE: Aesthetic Crown and Bridge Restorations Using a Fully Digital Workflow












