The rise of the digital age has transformed orthodontics as we know it.1 Due to its increasing popularity, Clear Aligner Therapy (CAT) has become a mainstay of contemporary orthodontics.2 This trend is largely due to the growing demand among prospective patients for more esthetic alternatives to traditional brackets and wires, including those presenting with dentofacial deformities.3,4 Accordingly, the number of clear aligner cases involving Orthognathic Surgery (OGS) presenting to our dentofacial center has also increased.
Although early methods for the adaptation of CAT with OGS was slow in most surgical centers, recent improvements in preoperative orthodontic prescription preparation.5,6 Computer Aided Surgical Simulation (CASS) and intra-oral scanners,7 intraoperative techniques regarding fixation and positioning8 and pre-surgical orthodontic mechanical support have created a fluid and easy transition for most orthognathic cases.
The challenges in adopting this technology for OGS relate specifically to the intraoperative control of the occlusion and the postoperative elastic guidance that is required. This has been well established in the use of fixed appliances but requires intuitive strategies that will be demonstrated in this article using CAT. As procedures become further established, complex cases such as multisegmental LeFort osteotomies are actually easier to manipulate and control if CAT are used with full crown covered CAD/CAM formed surgical guides that are fabricated to aid in intraoperative positioning.9
The goal for this paper threefold: (1) discuss considerations for pre-surgical orthodontics using CAT; (2) discuss methods of fixation developed at our centers and the workflow involved for the orthodontist and surgeon; (3) discuss the use and management of aligner trays perioperatively and postoperatively in regard to care, maintenance and stability.
I. Diagnosis and Treatment Planning of Skeletally based Malocclusions with CAT:
The primary challenge with pre-surgical orthodontics using CAT is the inability of some technicians to understand the need for creating a decompensated occlusion during the treatment planning setup. Special Instructions should be detailed to the technicians that the diagnosis is of a skeletal malocclusion and deformity. It must be emphasized that the case requires surgical preparation and a higher level of attention.
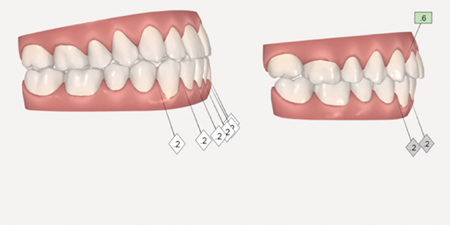
The default setup when using CAT systems is the creation of a Class I occlusion using dentoalveolar compensation, without consideration for the skeletal discrepancy. The example shown in figure 1 outlines a patient presenting with a Class III malocclusion due to maxillary retrognathia and transverse narrowing, requiring surgical intervention. Without specific guidance from the orthodontist, the technician will attempt to design a compensated occlusion with canines in Class I relation. The anterior view shows significant interproximal reduction (IPR) in the lower incisor region. (Fig. 1B) The lateral view shows a compromised setup involving dentoalveolar compensation through proclination and protraction of the maxillary incisors, retroclination of the mandibular incisors as well as the creation of space distal to the maxillary lateral incisors. (Fig. 2) In other words, the initial proposed setup was a nonsurgical correction with inadequate correction of midline and transverse discrepancies.
Fig. 1

A: Frontal view of pre-treatment occlusion; B: Frontal view of the
pre-surgical simulation.
Fig. 2

A: Pre-treatment; B: Post-treatment simulation.
The only way to address this problem is by bringing attention to specific items during the creation of the prescription and communicating this with the technician. Although the treatment planning process is continually being refined, the most critical elements are those that are commonly required for traditional orthognathic cases involving fixed appliances. (Table 1)
Table 1

When addressing intra-arch issues, level and alignment as well as spacing and crowding should be resolved for both arches prior to surgery. All spaces should be closed except those planned for future prosthetic or implant restorations. The management of crowding should be planned prior to prescription creation through proper diagnosis, treatment planning and cephalometric analysis. Primary methods for alleviation of crowding include IPR, proclination or extraction. When premolar extractions are warranted, the specific ones for the differing malocclusions should be removed. In general, for surgical corrections of Class II malocclusions, the upper second premolars and the lower first premolars are suggested in cases of moderate to severe crowding. Similarly, for surgical corrections of Class III malocclusions, the upper first premolars and the lower second premolars are suggested in cases of moderate to severe crowding.
The anterior-posterior relationship and the accompanying overjet should be worsened or at minimum, remain unchanged prior to surgery. Class III skeletal bases would require decompensatory mechanics, such as proclination of mandibular incisors to increase the negative overjet. Similarly, Class II cases would require an increase in positive overjet to maximize the effectiveness of the surgery, often through proclination of the maxillary incisors or uprighting of the mandibular incisors.
With regard to the vertical dimension and overbite, it is important to avoid over extrusion or intrusion of teeth prior to surgery, in order to avoid post-surgical orthodontic relapse. This is particularly true with anterior open bites where orthodontic closure of the open bite will result in a deceptive occlusal position at the time of surgical correction. This position is prone to relapse as the bite may open again after orthodontic appliances are removed.10,11 Bite ramps are surface projections built directly into the aligner trays and often required for deep bite cases.12 Unlike traditional bite turbos, which are bonded to the dentition, the removable nature of bite ramps allow them to be used prior to surgery without concern of interference with the surgical setup.
In the transverse dimension, posterior cross bites should not be corrected if the transverse discrepancy is significant enough to warrant segmental maxillary surgery. Likewise, midline discrepancies should be left uncorrected in the pre-surgical phase. The exception is in single jaw osteotomies. In these cases, if the non-operated jaw has a midline discrepancy that is not severe enough to warrant surgery), then traditional means of midline correction can be performed.
Lastly, attachments may be used by the orthodontist to optimize force delivery for achieving the tooth movements described above.13,14 They are made out of small composite shims bonded to the surface of the teeth.15 Attachments may be easily removed prior to surgery as new ones will be typically placed for the refinement aligners following surgery.
Following proper sequence and direction, the previous case can now be corrected using the steps above. The creation of a decompensated occlusion results in a more ideal environment for surgical correction. The facial esthetic improvements are more pronounced. The final occlusion is more stable as the teeth are in their proper positions. Midline and transverse discrepancies are also better treated. This particular case required 3 revisions with the technician prior to finally obtaining a pre-surgical setup with decompensation. (Fig. 3)
Fig. 3
B: Immediate postoperative setup. Surgical guides are prepared using the scanned models.
II. Intraoperative Management of osteotomies on Patients with CAT.
Perhaps the single most obvious reason why CAT and OGS are perceived with low compatibility is due to the intraoperative difficulty to localize, mobilize, position and fixate the dentoalveolar complex and dental arches. In absence of orthodontic brackets with surgical lugs, the ability to apply temporary maxillo-mandibular fixation (MMF) is difficult.8 The application of Erich arch bars or the fixation screws is also not a preferred or recommended technique due to damage to the gingiva and difficulty of oral hygiene maintenance. (Fig. 4A,B)
Fig. 4A

Fig. 4B

The available options for temporary MMF include:
- Application Erich arch bars and Ivy loops. (Fig. 4A)
- Application of screw retained arch bars. (Fig. 4B)
- Clear Aligner Orthognathic Splint (CAOS) (Fig. 4C)
- Insertion of temporary orthodontic anchor devices (TADs). (Fig. 4D)
- Insertion of Maxillomandibular fixation (MMF) screws. (Fig. 4E)
- Modification of orthodontic appliances bonded to all or specific teeth. (see case report)
- Bonding various prefabricated buttons to all or specific teeth.
- Bonding of full fixed orthodontic appliances one month prior to surgery.
Fig. 4C
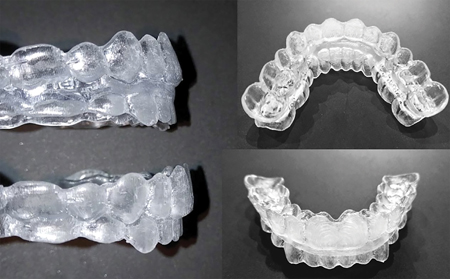
Fig. 4D

Fig. 4E

Currently the preferred methods at our center are: 1) The use of CAOS trays, 2) Placement of orthodontic TADs and 3) Placement of orthodontic brackets. The use of CAOS trays has been developed by the author (MC) in conjunction with virtual planning manufacturers to fit the full crowns of all the teeth in the arches and “snap” the arch in place. This appliance is a CAD/CAM designed acrylic splint analogous to two clear aligners luted together, aiding in the final positioning of the segments and fixation of the maxilla. (Fig. 4C) Removal of pre-surgical clear aligner attachments is recommended in order to allow for full seating of the CAOS tray. The two primary objectives of the CAOS trays are to position the osteotomized mandible or maxilla and to provide temporary MMF without the use of brackets or wires.
Another recommended approach is the insertion of at least 8 orthodontic TADs, distributed equally per arch and bilaterally. (Fig. 4D) In our experience, the larger MMF screws may create traumatic mucosal irritations over a 2-3-week period. (Fig. 4E) These are bulky and uncomfortable for patients to maintain over the long-term. The smaller orthodontic TADs have a better profile, are easier to clean and rarely create mucosal irritations. In addition, if the TADs fail or loosen during the peri-operative period, they are very easy to replace under local anesthetic. These TADs not only aid in perioperative fixation but also postoperatively as attachments for elastics.
Lastly, the bonding of orthodontic brackets is a quick and simple method for achieving temporary MMF. A minimum of 6 orthodontic brackets should be bonded at the cemento-enamel junction (CEJ) of the central incisors and canines and first molars in each arch. In our experience, orthodontic brackets placed at their ideal facial positions are more prone to breakage through shearing and do not have the bond strength to retain a 25-gauge inter-arch wire. This effect is minimized when the brackets or buttons are placed as apically as possible. Another advantage is the possibility to immediately wear the aligner tray postoperatively through creating cutouts at the area of the brackets. Elastics may also be attached through the small hooks on the brackets.
A challenging scenario when using CAT is associated with ligation of the maxilla during multisegmental LeFort osteotomies. Due to the lack of traditional orthodontic brackets, the segments can be especially difficult to fixate. For these cases, the use of a CAOS tray is the recommended, as the full cusp coverage is very helpful in seating maxillary segments by engaging the undercuts of the dentition. For cases that require additional rigidity or post-operative elastic management, the placement of orthodontic TADs or MMF screws may be used concomitantly with the CAOS tray. The preferred method is for the surgeon to incorporate a mandible first approach to double jaw cases, as it avoids the necessity of a two-in-one splint. (Fig. 5)
Fig. 5

Regardless of the method employed to attain temporary MMF, the application of rigid internal fixation remains the same. The key element is to ensure and maintain no movement of the bony
segments. The protocol used at our center is to bend 4 perfectly passive 2 mm thick L plates using a total of 16 screws for the maxilla. The mandible is fixed with 3 position screws or plates depending on the amount of advancement.
III. Postoperative Management of Patients with CAT.
Immediately following the completion of OGS, postoperative oral maintenance can be a challenging aspect for the patient to manage. This is primarily due to the difficulty in removal of the aligner trays at this time as well as upkeep of adequate oral hygiene.
Post-surgical elastics are often required to uphold and support the corrected occlusion. They may be attached through orthodontic TADs, bonded buttons or directly to the notches on the aligner tray. Bonded buttons are typically placed on the gingival aspect of the clinical crown and will require relief cutouts on the aligner tray. Notches made directly to the aligner tray should have attachments for additional aligner retention. Various configurations of elastics may be used, depending on the pre-surgical malocclusion, such as class II, class III or box elastics. (Fig. 6) In cases where post-surgical settling of the buccal segment is required, trays may also be cut posteriorly.
Fig. 6A

Refinement aligners are recommended in the postoperative phase in order to accommodate any adjustments necessary following surgery, as well as to improve tray fitting. Intra-oral scanning may be performed after the 2nd week, with the goal of delivering the refinement aligners by the 4th week. Refinement aligners are mandatory for segmental maxillary surgery case due to inherent changes in the arch form. In these cases, intra-oral scans should be done by the surgeon during the 2-week follow up appointment and clinical virtual planning performed by the orthodontist and surgeon with the final aligners delivered to the orthodontist.
Case Report
A 25-year-old healthy male patient presented with a Class III malocclusion of skeletal and dentoalveolar etiology for orthodontic treatment. Extraorally, the patient had a prognathic facial type with a concave profile. Intraoral exam revealed a slightly constricted maxillary arch with mild crowding and a moderately crowded mandibular arch with excess negative overjet. (Fig. 7) A non-extraction treatment plan with a surgery-early approach using CAT was selected in conjunction with orthognathic surgery to advance the maxilla, rotate the occlusal plane and set back the mandible.
Fig. 7A

Fig. 7B

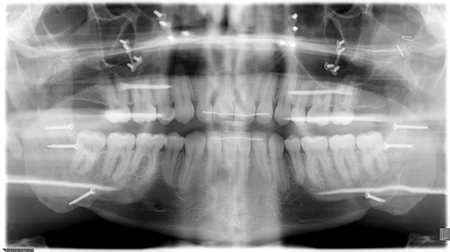
The Pre-surgical Set of aligners consisted of only 10 stages in total. Crowding in the lower anterior region was alleviated by proclination of the lower incisors. (Fig. 8) The pre-surgical phase was completed in approximately 3 months. Following decompensation, the method of temporary MMF used was with the aid of the CAOS splint and 4 TADS. The planned movements were a setback of the mandible of 4.5 mm and slight asymmetry correction followed by a 4 mm advancement and 3 mm impaction of the maxilla. The patient had all CAT attachments removed one month prior to surgery and 4 passive aligners were delivered. These were to be worn for one month pre- and one month post-surgery. During the first two weeks following surgery, the patient was kept on corrective elastics to maintain the occlusion, using the same TADs as points of attachment. (Fig. 9) Following an uneventful post-operative course, the patient returned to clinic on week 2 and was scanned for the Refinement Set of aligners. The virtual treatment plan was performed in coordination with the surgeon and the orthodontist, resulting in 20 additional aligners delivered to the patient by approximately the fourth week. The final occlusion was achieved after 11 months, with complete correction of the anterior-posterior and transverse deficiencies and satisfaction of the patient. The total treatment time was
16 months. (Fig. 10)
Fig. 8A

Fig. 8B

Fig. 8C

Fig. 9A

Fig. 9B

Fig. 9C

Fig. 9D

Fig. 9E
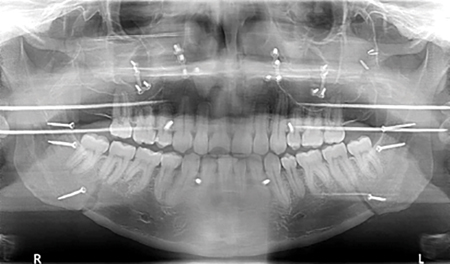
Fig. 10A

Fig. 10B

Fig. 10C
Conclusion
Clear aligner therapy in conjunction with orthognathic surgery can be an effective treatment for orthodontic patients presenting with skeletal discrepancies. This article outlines the treatment recommendations for both the Orthodontist and Oral and Maxillofacial Surgeon. Preoperatively, it is critical that the virtual setup is designed with proper decompensation. Intraoperatively, preparations for methods of maxilla-mandibular fixation must be considered. Postoperatively, refinement scans are recommended for finishing the case. Initially seen as a challenging and problematic strategy to manage patients with dentofacial deformities, clear aligner technology does provide for certain benefits (Table 2) in surgical cases that can be taken advantage of and should not deter practitioners from using them.
Table 2

Oral Health welcomes this original article.
Acknowledgement: The authors would like to thank Dr. Sky Naslenas for providing the orthodontic treatment in the case presented.
References
- Keim RG. The Evolution of Invisalign. J Clin Orthod 2017;51(2):69-70.
- Weir T. Clear aligners in orthodontic treatment. Aust Dent J 2017;62 Suppl 1:58-62.
- Ziuchkovski JP, Fields HW, Johnston WM, Lindsey DT. Assessment of perceived orthodontic appliance attractiveness. Am J Orthod Dentofacial Orthop 2008;133(4 Suppl):S68-78.
- Rosvall MD, Fields HW, Ziuchkovski J, Rosenstiel SF, Johnston WM. Attractiveness, acceptability, and value of orthodontic appliances. Am J Orthod Dentofacial Orthop 2009;135(3):276 e1-12; discussion 76-7.
- Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod 2015;85(5):881-9.
- Rossini G. Controlling orthodontic tooth movement with clear aligners. Journal of Aligner Orthodontics 2017;1(1):7-20.
- Swennen GR, Mollemans W, Schutyser F. Three-dimensional treatment planning of orthognathic surgery in the era of virtual imaging. J Oral Maxillofac Surg 2009;67(10):2080-92.
- Taub DI, Palermo V. Orthognathic surgery for the Invisalign patient. Seminars in Orthodontics 2017;23:99-102.
- Caminiti M, Lou T. Clear Aligner Orthognathic Splints. Journal of Oral and Maxillofacial Surgery.
- Huang GJ. Long-term stability of anterior open-bitetherapy: A review. Paper presented at; 2002.
- Solano-Hernández B, Antonarakis GS, Scolozzi P, Kiliaridis S. Combined orthodontic and orthognathic surgical treatment for the correction of skeletal anterior open-bite malocclusion: a systematic review on vertical stability. Journal of Oral and Maxillofacial Surgery 2013;71(1):98-109.
- Khosravi R, Cohanim B, Hujoel P, et al. Management of overbite with the Invisalign appliance. Am J Orthod Dentofacial Orthop 2017;151(4):691-99 e2.
- Simon M, Keilig L, Schwarze J, Jung BA, Bourauel C. Forces and moments generated by removable thermoplastic aligners: incisor torque, premolar derotation, and molar distalization. Am J Orthod Dentofacial Orthop 2014;145(6):728-36.
- Schupp W, Haubrich J. Aligner Orthodontics: Diagnostics, Biomechanics, Planning and Treatment: Quintessence Publishing; 2016.
- Tuncay OC. The invisalign system. London [u.a.]: Quintessence Publ.; 2006.
About the Authors
 Dr. Marco Caminiti Head and Program Director, Assistant Professor: Oral and Maxillofacial Surgery,Surgical Director; Center for Corrective Jaw Surgery, University of Toronto, M5G 1G6.
Dr. Marco Caminiti Head and Program Director, Assistant Professor: Oral and Maxillofacial Surgery,Surgical Director; Center for Corrective Jaw Surgery, University of Toronto, M5G 1G6.
 Dr. Tiantong Lou Clinical Instructor, University of Toronto. STO Orthodontists, 300 Borough Dr., Suite 36A, Scarborough, Ontario M1P 4P5.
Dr. Tiantong Lou Clinical Instructor, University of Toronto. STO Orthodontists, 300 Borough Dr., Suite 36A, Scarborough, Ontario M1P 4P5.












