Osseodensification (OD) is a innovative technique that aims at bone preservation utilizing the collection of autogenous bone with nonsubtractive drilling within the implant site via the compaction of cancellous bone, which has good viscoelastic and plastic deformation characteristics. Unlike traditional osteotomy, OD does not excavate bone but simultaneously compacts and autografts the particulate bone in an outward direction to create the osteotomy, thereby preserving vital bone tissue and increasing both quantity and density of the peri-implant bone.1 This is achieved using specialized densifying burs The Densah burs.
Osseodensification has been at the forefront of changes in surgical site preparation in implantology. This relatively new concept with specialized drills has been proposed to help through improved osteotomy preparation, bone densification, crestal sinus lift and also achieve bone expansion at different sites of varying bone densities. This procedure has also shown improvement in achieving better implant primary stability then conventional implant drills. Osseous densification significantly increased insertion and removal torques compared to standard drilling or extraction drilling.2 Primary stability of a dental implant is a fundamental factor for achieving successful osseointegration. Surgical procedure and bone quality are among the most common factors that affect primary stability. Maintaining sufficient bone density is essential to achieve the necessary bone-to-implant contact for obtaining a biomechanically stable implant.
The aim of this article is to provide clinicians a better understanding of OD and the approach used to optimize the technique. It also highlights positive clinical outcomes in cases where initial bone density and quantity have been compromised.
Use of osseodensification for crestal sinus augmentation in combination with bone putty, particulate bone or alone are the most commonly used techniques for these burs. The use of Densah burs in densifying mode can breach the sinus floor with autografting without causing any perforation. The simplified minimally invasive antral membrane elevation technique is based on the application of hydraulic pressure by a viscous bone graft that acts as an incompressible fluid to atraumatically elevate the schneiderian membrane. Increased implant stability is achieved due to osseous densification of the Residual Bone by Densah bur. Thus, the proposed technique could be recommended for sites with minimal residual height.3 With this technique an implant can be placed simultaneously.
Fig. 1

Fig. 2

Fig. 3
A CBCT is first used to measure the height from the ridge to the sinus floor. In cases where posterior residual alveolar ridge height is insufficient, and additional vertical depth is desired, drill to the depth determined within an approximate safety zone of 1.0 mm from the sinus floor using a pilot drill (in clockwise direction). Confirm pilot drill position with a radiograph. The appropriate osteotomy diameter is created with this technique using successive burs in reverse mode (counter-clockwise 800-1200 rpm with copious irrigation for lubrication and to minimize overheating). According to the manufacturer, up to 3 mm of additional bone height can be achieved simply with OD without the need for additional bone grafting material. If greater vertical height is desired the bone putty/particulate can then be introduced through the osteotomy and the OD burs used to propel the graft material apically beneath the sinus membrane in the absence of irrigation. Implant placement is then performed and tissues sutures closed. The increase in bone height is comparable to that obtained with lateral window procedures.4
Osseodensification may facilitate lateral ridge expansion. Although, OD will not create the tissue, it will optimize and preserve what already exists. This procedure requires ≥ 2 mm of trabecular-bone core and ≥ 1/1 trabecular:cortical bone ratio to achieve a predictable plastic expansion. The more cortical bone there is, the more trabecular core is needed to facilitate predictable expansion. The ideal minimum ridge is 4mm in width.5 This protocol is indicated to expand a ridge with a narrow crest and wider base. It is not indicated in resorbed ridge with a narrow base.
A CBCT is first used to assess the amount of trabecular bone available and to evaluate if the bone composition present is conducive to predictable plastic expansion. Following flap elevation, begin with a narrow pilot osteotomy. Follow with the narrowest Densah Bur set the drill motor to reverse mode (counter-clockwise) with copious irrigation. Run the bur into the osteotomy. When feeling the haptic feedback of the bur lift off pressure and reapply, repeatedly lift off and reapply pressure with a pumping motion until reaching the desired depth.
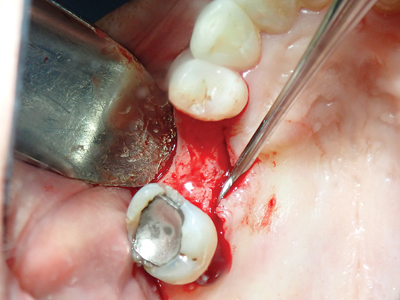
Fig. 4

Fig. 5

As the bur diameter increases, the bone may gradually expand to the final diameter. Trisi P et al., in his animal study concluded that OD technique helps in bone expansion so that wider diameter implants could be inserted in narrow ridge without creating bone dehiscence or fenestration.6 This expansion may allow for total implant length placement in autogenous bone without thread exposure. Following implant placement it is important to assess the buccal bone thickness to determine if sufficient bone is present or if augmentation is required. The tissues are then sutured closed Osseodensification burs can be used for immediate implant placement. Begin with atraumatic tooth extraction with minimal or no flap reflection. Following socket degranulation and irrigation use the pilot drill in clockwise mode to achieve implant trajectory. Choose implant diameter based on the tooth or its socket apical diameter. Implant needs to be slightly wider than the tooth apex. This will allow the implant stability to be mainly provided by the apical portion of the socket. Choose a Densah Bur to be the last preparation bur based on its diameter relative to the tooth or its socket apical diameter. The final bur needs to be ≥ to the apical diameter of the tooth or its socket. After the pilot osteotomy, change the drill motor to reverse mode (counter-clockwise with copious irrigation). To prep the site, start with the narrowest OD bur, in reverse mode, until reaching the desired depth (begin by introducing the running bur into the osteotomy.) When feeling the haptic feedback of the bur pushing up out of the osteotomy, lift off and reapply pressure with a pumping motion until reaching the desired depth. Use wider and wider burs until reaching the designated sized osteotomy. As the bur diameter increases, the apical bone will slowly expand to accommodate the designated implant diameter. Place the implant into the osteotomy and fill the gap distance with well hydrated allograft.
Osseodensification can be used for molar septum expansion for implant placement. Section molar roots at the furcation without compromising the integrity of the septum. Perform atraumatic mesial and distal root extraction. Degranulate the socket and irrigate to expose the septum area. Use the pilot drill in the clockwise mode to a depth that is 1mm deeper than the planned implant length. Use the subsequent OD burs (in counter-clockwise mode with copious irrigation) in small increments to increase bone plasticity and to gradually expand the osteotomy. Place the implant to depth and fill the gap distance with bone grafting material if needed.
Discussion
Advantages of Osseodensification Compaction autografting/condensation:
Bone debris is redistributed up the flutes of the bur and is pressed into the trabecular walls of the osteotomy. The autografting supplements the basic bone compression, and the condensation effect acts to further densify the inner walls of the osteotomy.6
Fig. 6

Fig. 7

Increases bone density:
The Densah burs have been shown to allow bone preservation and condensation through compaction autografting during osteotomy preparation, increasing the peri-implant bone density (BV%), and the implant mechanical stability.2
A study conducted by Huwais S and Meyer EG confirmed the hypothesis that the OD technique increases primary stability, bone mineral density and the percentage of bone at the implant surface. They also concluded that, by reserving bulk bone, healing process would be accelerated due to bone matrix, cells and biochemicals maintained and autografted along the osteotomy surface site.2
Residual ridge expansion: Narrow ridges have been shown to expand in width along with OD thus facilitating the placement of larger diameter implants and also avoiding of fenestration and dehiscence defect.6 The Densah bur technology facilitates ridge expansion with maintained alveolar ridge integrity and also allows for complete implant length placement in autogenous bone with adequate primary stability. Despite compromised bone anatomy, OD preserved bone bulk and promoted a shorter waiting period to the restoration.7
Increased primary implant Stability:
Huwais and Meyer (2017) showed clearly that osseodensification significantly increased insertion and removal torques compared to standard drilling and extraction drilling. No significant differences in ISQ readings or temperature increases were demonstrated among the three groups, confirming the safety of osseodensification. It was concluded that by preserving bone, using osseodensification, the healing process was accelerated and primary implant stability was increased while in situ autograft bone was maintained along the surface of the osteotomy site.
Osseodensification technique has demonstrated to be able to increase the BV% around dental implants inserted in low-density bone in respect to conventional implant drilling techniques, which may play a role in enhancing implant stability and reduce micromotion.6
Contraindications of Osseodensification
Case selection for using OD burs in counter-clockwise mode is important as the procedure is not recommended in dense bone (D1, D2). Furthermore, it is most important to not undersize the implant osteotomy with the use of OD as this could result in bone necrosis and implant failure.8 In OD over-compression may unintentionally cause bone necrosis.9
OD does not work with cortical bone as cortical bone is a non-dynamic tissue which lacks plasticity. Densification of xenografts should be avoided because they behave biomechanically different than the bone tissue, as they have only inorganic content and they just provide the bulk without any viscoelasticity.10
Incorrect use of this technology may lead to implant failure that would otherwise not have occurred with the use of standard conventional burs. Clinicians are cautioned that there is an upper limit to how much bone can be compressed/densified.8
Conclusion
Osseodensification represents a novel implant osteotomy technique that has been shown to preserve bone volume through the compaction of cancellous bone due to bones viscoelasticity and plastic deformation properties. The use of OD burs offers the ability to obtain improved primary stability in cases where it previously may not have been obtainable or poor. This method has been shown to be effective for a variety of clinical indications when utilized in low-density bone. In the current article multiple clinical applications were discussed however no doubt greater applications exist for these versatile burs.
Oral Health welcomes this original article.
Declaration: The author declares that there is no conflict of interest with the product mentioned.
References
- Pai UY, Rodrigues SJ, Talreja KS, Mundathaje M. Osseodensification- A novel approach in implant dentistry. J Indian Prosthodont Soc. 2018 Jul-Sep; 18(3):196-200.
- Huwais S., Meyer E., Osseodensification A novel approach in implant o preparation to increase primary stability, bone mineral density and bone to implant contact. Int J Oral Maxillofac Implant. 2017: 32(1):27-36.
- Baron Tarun Kumar; Venkatraman Narayan (2017) Minimally invasive crestal approach sinus floor elevation using Densah burs and Hydraulic lift utilizing putty graft in cartridge delivery. Clin Oral Impl Rex, 28: 203-203.
- Nilesh Salgar Osseodensified Crestal Sinus Window Augmentation: An Alternative Procedure to the Lateral Window Technique J Oral Implantol (2021) 47 (1): 45–55.
- Stepan Jarikian , Mohamad Hassan Jaafo , Zuhair Al-Nerabieah Clinical Evaluation of Two Techniques for Narrow Alveolar Ridge Expansion: Clinical Study. Int J Dentistry Oral Sci. 2021;8(1): 1047-1052.
- Trisi P, Berardini M, Falco A, Vulpiani MP. New osseodensification implant site preparation method to increase bone density in low-density bone: in vivo evaluation in sheep. Implant Dent. 2016;25.
- Huwais S. Enhancing implant stability with osseodensification: A two year follow up. Implant Pract. 2015;8:28–34.
- Pikos MA, Miron RJ.. To Drill or to Densify? Clinical Indications for the Use of Osseodensification Compend Contin Educ Dent. 2019 May;40(5):276-281
- Wang L, Wu Y, Perez KC, et al. Effects of condensation on peri-implant bone density and remodeling. J Dent Res. 2017;96(4):413-420.
- Kanathila H, Pangi A, An Insight into the Concept of Osseodensification-Enhancing the Implant Stability and Success. July 2018. Journal of Clinical and Diagnostic Research.(7): ZE01-ZE03.
About the Author
 Dr. Melissa Goodman is in private practice in Toronto, limited to periodontics and implant surgery. She is on staff in the Department of Dental and Maxillofacial Sciences at Sunnybrook Health Sciences Centre. Dr. Goodman is a Fellow of the Royal College of Dentists of Canada in Periodontology. She obtained her DDS from the University of Toronto in 2006, and subsequently completed a general practice residency at Sunnybrook Health Sciences Centre. Dr. Goodman completed her specialty training in Periodontology at New York University in 2010. She can be reached at drgoodmanperio@gmail.com or through Instagram @drgoodmanperio.
Dr. Melissa Goodman is in private practice in Toronto, limited to periodontics and implant surgery. She is on staff in the Department of Dental and Maxillofacial Sciences at Sunnybrook Health Sciences Centre. Dr. Goodman is a Fellow of the Royal College of Dentists of Canada in Periodontology. She obtained her DDS from the University of Toronto in 2006, and subsequently completed a general practice residency at Sunnybrook Health Sciences Centre. Dr. Goodman completed her specialty training in Periodontology at New York University in 2010. She can be reached at drgoodmanperio@gmail.com or through Instagram @drgoodmanperio.












