Medical History Of The Pediatric Patient
Obtaining accurate histories for children during their primary assessment requires obtainment of information from third parties such as parents, designated powers of attorney or other health care providers. Highly relevant information includes:
• Underlying bleeding disorders
• Congenital cardiac disease and history of their repair
• Family history of significance; eg: bleeding disorders, malignant hyperthermia
• Latex allergy
• Food allergies, use of epipen
• Spina bifida occulta
• Down Syndrome
• Premature childbirth, any complications during delivery
• Autism spectrum disorder
• Asthma
• Seizure disorder,
• Previous exposure to general anesthesia and history of complications
Indications for covering children with antibiotics for prophylaxis against infective endocarditis, as with adult patients, remain unchanged from the guidelines published by the American Heart Association (AHA) IN 2007, and include the following: previous infective endocarditis, history of cardiac valve repair, select patients with congenital cardiac disease, and cardiac transplant recipients.1 If a child patient has undergone previous repair of a congenital cardiac defect, it is prudent for the dentist to consult with the patient’s cardiologist regarding insight as to the presence of residual shunts or defects that may require antibiotic coverage.1
While many dental offices are now latex free, or “latex safe”, one must consider the multiple possible portals of latex exposure that could exist in the office setting, including: emergency airways, nitrous oxide masks, oxygen masks, gloves, bandages, mouth prop covers, rubber dam, and alginate mixing bowls (Fig. 1). The incidence of latex allergy in patients with spina bifida is severely high such that all patients with this condition require treatment in a latex-free environment, and oral surgical procedures are often performed in the hospital setting. Patients with a history of certain food allergies, including strawberry, kiwi, bananas, chestnuts, avocado and tomato should be questioned specifically about past reactions to latex, as approximately 50% of patients with latex allergy have a history of another type of allergy.
Figure 1

Diligent attention to all potential sources of latex exposure are essential to ensuring safe delivery of dental care to patients with potential latex allergy.
Figure 2

An anesthetic technique is selected to allow for the safe and comfortable provision of the planned surgical procedure with optimal patient
compliance.
Behaviour Management
The provision of oral surgery in children usually requires consideration of some form of sedation or general anesthesia. Particularly in younger children, cooperation with administration of local anesthesia and the safe provision of oral surgical procedures can be a significant challenge.
Nitrous oxide/oxygen conscious sedation can, in select instances, be a useful adjunct; however, this technique requires a moderate degree of patient cooperation to be successful. Oral midazolam has also been shown to be safe and effective for conscious sedation in the pediatric outpatient population.2 One must be cognizant of the possibility of dysphoria as a side effect of oral benzodiazepine administration, which may render the child unable to undergo the planned procedure in the absence of a general anesthetic.
General anesthesia is often beneficial for the child patient who requires oral surgery, particularly in the presence of underlying anxiety (Fig. 2). Pre-surgical consultation allows both the child and his or her parents to develop rapport with the surgeon and become comfortable in an unfamiliar office. Early morning appointments are ideal for younger children to minimize the length of NPO time during awake hours. Administration of a “needle-free” anesthetic via mask induction with an inhalational anesthetic agent can greatly expedite the delivery of care for many children. While the goal in selecting a particular anaesthetic technique is to be able to successfully complete a given procedure with cooperation, consideration should be given to the length of the planned procedure, the nature of the intended surgery, and the need for lack of patient movement to allow for safe completion. It is essential that the choice of anesthetic or sedation technique is well within the training and comfort level of both the dental provider and the attending staff. Consideration may be given to delegating administration of anesthesia to separate providers in the pediatric population. In certain instances of medical compromise, provision of care in the hospital setting is ideal, particularly with a history of underlying bleeding disorder, residual cardiac defect, severe latex allergy (ie, spina bifida), muscular dystrophy or a known family history of malignant hyperthermia.3
Local Anesthesia
While it is essential to establish effective local anesthesia in children, it is important to remember the increased potential for local anesthetic overdose and toxicity. Duration of the selected anesthetic is also of importance; the shortest acting anesthetic consistent with the provision of ideal intra-operative and post-operative comfort should be utilized, remembering the potential for children to inflict self-induced biting trauma to anesthetized lips and tongues. The risk of local anesthetic toxicity can be reduced by weighing children prior to surgery, selecting an anesthetic with a high safety range, i.e., a low concentration that allows for a larger volume of anesthetic administration, and aspiration prior to nerve block injection,
Radiography
Imaging of teeth that are planned for extraction, whether the teeth are erupted, unerupted or impacted, must reveal the full anatomy of the tooth, and any regional anatomy of importance. In the presence of ankylosed primary teeth, it is essential that the bone apical to the tooth is imaged, and that it is known whether a permanent succedaneous tooth is present or absent. Localization of unerupted teeth can be greatly expedited with cone beam CT imaging prior to surgery, which enables the surgeon to know with precision how to approach teeth such as impacted supernumeraries. Furthermore, this imaging can reveal or rule out the existence of resorption of adjacent tooth roots, and reduce the risk of iatrogenic damage to adjacent teeth. Minimization of radiation dose is a paramount requirement; the choice of radiographic technique must be made fully cognizant of this, but also consistent with the imaging required for accurate diagnosis and surgical planning (Figs. 3-5).
Figure 3

Impacted left canine. Localization of the tooth cannot be confined on two-dimensional imaging.
Figure 4

Cone beam CT of the impacted canine in Figure 3. Cross sectional view reveals the canine to be in labioversion; in addition, a compound odontome is diagnosed as contributing to the failure of the canine to erupt.
Figure 5

Cone beam CT cross sectional view of an impacted mandibular supernumerary premolar, positioned within the middle of the alveolus and in close proximity to the mental neurovascular bundle.
Ankylosis Of Primary Teeth
Ankylosis in the primary dentition is an asymptomatic and not uncommon phenomenon. The etiology of ankylosis has not been determined. The periodontal ligament is lost, with subsequent fusion of cementum and bone. Ankylosis results in restricted growth and development of the alveolar process associated with the ankylosed unit. In the initial phase, the ankylosed tooth can be referred to as “spot welded” to the bone. The ankylosed interface progressively increases with time. The concept of “submerging” teeth is somewhat misleading; in essence, ankylosis halts the vertical development of the alveolus. The adjacent portions of the alveolus housing non-ankylosed teeth continues to exhibit normal vertical and horizontal growth, which by default causes the ankylosed tooth/bone unit to appear submerged. The magnitude of the osseous defect increases the longer the tooth remains ankylosed. The incidence of ankylosis appears to be unrelated to the presence or absence of a succedaneous bicuspid tooth. Diagnostic criteria for ankylosis includes relative submergence of the ankylosed tooth as described above, a hypertympanic tone of the ankylosed tooth on percussion, and loss of the periodontal ligament space on radiography. In more severe cases there may be tipping of adjacent teeth, with loss of mesio-distal spacing (Fig. 6). In cases where primary molar ankylosis occurs in the presence of congenitally absent premolars, a vertical and horizontal osseous defect exists as a consequence of the ankylosis that is pertinent to the eventual placement of dental implants. In addition, relative submergence of an ankylosed tooth exerts an inhibitory effect on eruption of neighbouring teeth (Fig. 7).5 Surgical removal of the ankylosed tooth is indicated at the earliest opportunity to minimize the resultant osseous defect and disruption of the occlusal plane.
Figure 6

Severe ankylosis of a mandibular primary second molar. Note the loss of PDL space, relative submergence of the tooth and loss of interdental space.
Figure 7

Ankylosis of maxillary and mandibular primary molars; inhibition of eruption of adjacent teeth with severe occlusal plane disruption.
Infections
Odontogenic infections are fairly common in children, and exhibit signifiant clinical and bacterial variability. As children can develop rapid systemic involvement of infection, early management is crucial. Resistant anaerobic bacterial strains are becoming increasingly prevalent, as is seen with adult infections as well. The ethology of pediatric infections includes both odontogenic and non-odontogenic sources. Since the advent of Haemophilus influenzae type B (HiB) vaccine, its contribution to facial cellulitis of unknown origin has virtually vanished. There is now a growing prevalence of facial cellulitis due to Streptococcus pneumoniae, which is increasingly resistant to penicillin.6 There has been a lower risk of meningitis associated with facial infections related to S. pneumoniae compared with the previous experience with H. influenzae; however, the incidence of bacteremia is higher. Risk factors for S. pneumoniae include a recent history of upper respiratory tract infection or otitis media. Most cases of facial infection continue to be caused by mixed microbiological flora. Children have relatively porous jaw bone with large, open marrow spaces, and this can allow for rapid spread of infection into fascial spaces within under 24 hours. The classic presentation of facial cellulitis is that of an indurated, brawny swelling (Fig. 8). The optimal treatment is prompt incision and drainage, and immediate extraction of an odontogenic source, when possible, consistent with the adage to “never let the sun set on pus”. Immediate extraction of the offending tooth may be considered curative in the absence of systemic signs and symptoms, minimal soft tissue swelling, and the absence of contiguous fascial space involvement and trismus; however, this can be challenging due to reduced efficacy of local anesthesia in the presence of inflammation, poor patient cooperation and trismus. Prompt hospital admission must be considered in pediatric patients requiring systemic management for fever, diminishing level of consciousness, signs of dehydration or potential loss of airway. The common systemic complications of infections in children are sepsis and dehydration, which may develop quickly after the development of a toothache and local swelling. Oral antibiotics are indicated when there is minimal swelling, and the patient exhibits adequate oral intake. Referral for more involved therapy should always be made when the initial presentation includes decreased oral intake, with the potential for dehydration, and temperature elevation. Prompt referral should also be made in cases where there is a progressive worsening of symptoms despite initial treatment. Intravenous antibiotics and hospital admission are required in all cases presenting with swelling, and potential loss, of the airway, periorbital swelling, cervical space involvement, decreased level of activity and decreased oral intake.
Figure 8

Facial cellulitis with periorbital involvement.
Figure 9

Large dentigerous cyst associated with impacted tooth 48. This lesion was asymptomatic on presentation. Note the posterior displacement of the causative third molar due to the lesion, bringing it in closer proximity to the mandibular canal.
Third Molars
Impaction of third molars remains a common finding in the adolescent patient. As the rate of physical development and maturation is increasing in the pediatric patient, so too is the rate of dental development. Patients will often present with accelerated root development of the mandibular third molars relative to their chronologic age. Panoramic radiographic examination to evaluate the presence, position and stage of development of the third molars should be considered by the age of 15. While not all third molars require surgical management, a systematic review of prospective studies has evaluated the cumulative long-term risks of retaining asymptomatic third molars and the likelihood of requiring their eventual removal, in comparison with the relatively low risk of early preventive removal. A 3% annual risk of requiring removal of previously asymptomatic third molars, with a cumulative risk of 64% of requiring extraction up to 18 years following primary assessment has been shown.7 Given the documented high incidence of problems associated with third molars over time, it is recommended that patients with third molar impactions should be evaluated by someone experienced and expert in third molar management.8 The presence of untreated, retained impacted teeth, and third molars in particular, is known to carry a risk of inducing pericoronal and fascial space infection, predisposition to odontogenic cystic pathology and damage or resorption of adjacent teeth and periodontium (Fig. 9). When it becomes apparent that third molars will not have adequate space for eruption, consideration should be given to recommending third molar removal. Patients with dental crowding requiring premolar extractions generally lack sufficient arch space to facilitate successful third molar eruption. Third molar surgery is more difficult and carries increased risk as patients age; therefore given the desire to achieve therapeutic goals, obtain positive outcomes, and avoid known risks and complications, a decision should be made before the middle of the patient’s third decade to remove or continue to observe third molars, with the knowledge that future treatment may be necessary based on the clinical situation8. Patients should also be informed of the greater difficulty and increased rate of complications associated with third molar removal as they age.7 When impacted third molars are removed after the age of 26, there is a greater potential for impaired bone regeneration at the distal aspect of the mandibular second molars, potentially requiring grafting.9 If third molars are planned for removal, surgery is ideally performed prior to completion of mandibular root development (Fig. 10). In general terms, this can result in a decreased risk of post-surgical hypoesthesia or paresthesia in the areas of distribution of the inferior alveolar and lingual nerves (Fig. 9). In instances where root development is complete, and the risk of inferior alveolar or lingual nerve injury is judged to be elevated, consideration is given to cone beam CT imaging and possibly coronectomy in an effort to minimize these risks (Figs. 11 & 12).
Figure 10

Impaction of third molars with incomplete root development; ideal timing for prophylactic removal.
Figure 11

19-year-old female, advanced third molar root development with close proximity to the mandibular canals.
Figure 12
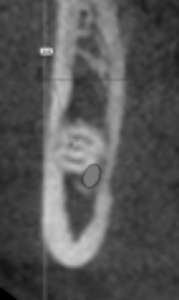
Cone beam CT cross sectional view of left mandibular third molar of the patient in Figure 11, confirming intimate proximity of the third molar root to the mandibular canal. The risk of inferior alveolar nerve injury is increased in this case relative to the risk had surgery been performed earlier.
Exposure Of Impacted Teeth
Management of impacted canines and incisors, whether maxillary or mandibular, is an interdisciplinary treatment that requires coordination and communication between the treating orthodontist and oral and maxillofacial surgeon. The availability of cone beam CT imaging is often beneficial in providing definitive localization of the tooth prior to exposure surgery, minimizing the risk to adjacent teeth, and to rule out resorption of adjacent roots. Exposure of palatally impacted teeth can often be performed with an “open window” approach, allowing the tooth to descend through the surgically created window, whereby bonding of the orthodontic attachment can be performed either at the time of surgery or secondarily (Fig. 13). Exposures of teeth that are positioned labially in the arch are best managed with apical repositioning of the pedicled flap to maintain an optimal cuff of keratinized gingiva following orthodontically guided eruption (Figs. 14 & 15). In cases where the impacted tooth is positioned very high and labial in the arch, it is necessary to close the flap in primary fashion, and for the tooth to be guided into occlusion without full exposure. In other situations, extraction of the impacted tooth may be indicated if the prognosis for orthodontically guided eruption following exposure surgery appears to be poor (Fig. 16).
Figure 13

Surgical exposure of palatally right maxillary canine.
Figure 14

Impacted left maxillary central incisor, exposed with apical flap repositioning.
Figure 15

Orthodondtically guided tooth 21 following surgical exposure with apical flap repositioning; note maintenance of healthy keratinized gingival tissue.
Figure 16

Impacted mandibular canine; position not amenable to exposure and orthodontically assisted eruption.
Supernumerary Teeth
Children may present with supernumerary permanent teeth in the maxilla, mandible or both. The maxillary mesiodens is the most common supernumerary tooth to develop. Removal of supernumeraries is often indicated to facilitate orthodontic repositioning of malposed incisors, and to eliminate the risks of cyst development and resorption of adjacent roots (Fig. 17). In cases where the mesiodens is developing in close proximity to developing incisor roots, it may be prudent to defer surgery until incisor root development is complete (Figs. 18 & 19). Patients may present with either single or multiple supernumeraries that can impede normal dental development. The presence of a large number of supernumerary teeth can be pathognomonic of cleidocranial dysplasia (Fig. 20).
Figure 17

Impacted right mandibular super-numerary premolar, with resorption of the root of tooth 45.
Figure 18

Inverted mesiodens in close proximity to tooth 21 with incomplete root development; premature for removal.
Figure 19

Mesiodens from Figure 18; root development of 21 close to completion, removal of mesiodens unlikely to damage adjacent root.
Figure 20

Cleidocranial dysplasia: large numbers of supernumerary teeth impeding eruption of the normal permanent dentition. Surgical treatment is complex, and often necessitates multiple surgeries involving removal of supernumeraries and exposure and bonding of permanent teeth.
Congenital Absence Of Teeth
The management of the patient with congenitally missing teeth presents a unique challenge for the dental clinician, often requiring multidisciplinary care to effect an optimal treatment outcome.
The mandibular second premolar teeth are the teeth most commonly found to be absent. In cases with agenesis of the maxillary lateral incisor, it is more common for the malformation to affect these teeth bilaterally than unilaterally. Absence of maxillary first and second premolars, and mandibular second premolars, has a greater tendency to be unilateral than bilateral. Most afflicted patients present with only one or two missing teeth. Congenital tooth absence may be associated with several conditions, or can occur as an isolated finding. Patients may present with relatively few missing teeth (hypodontia), or a large number of teeth (oligodontia). Oligodontia is believed to have a genetic predisposition, but is also known to occur sporadically.5 The condition is also known to present as a component of other syndromes, including cleft lip and palate (CLCP), Down syndrome (trisomy 21), and the ectodermal dysplasias. A clinical suspicion of congenital absence of permanent teeth should be raised by failure of primary teeth to exfoliate in a timely fashion. Screening two-dimensional radiography, consisting of a full mouth series or panoramic radiograph, should be performed at an age consistent with the pediatric patient’s stage of dental development. Noted absence of the maxillary lateral incisors, and/or mandibular or maxillary premolar teeth, are indications for diagnostic imaging. In addition, the presence of submerging ankylosed primary molars, should raise the clinician’s awareness of the need for radiography, although ankylosed teeth may present with or without an underlying absence of the succedaneous permanent teeth. Most patients with congenital tooth absence require orthodontic therapy to appropriately align the dental arches, and to ideally diverge roots of teeth adjacent to edentulous spaces to allow for safe placement of dental implants (Figs. 21 & 22).
Figure 21

Non-syndromal oligodontia with retained primary teeth.
Figure 22

Oligodontia treated with dental implant therapy.
In Ontario, the Ministry of Health and Long Term Care (MOHLTC) provides funding for children with CLCP, syndromes with a craniofacial component including Down syndrome, Gorlin syndrome and ectodermal dysplasia, as well as non-syndromal oligodontia. The provincial guideline to be eligible for funding for the treatment of oligodontia is the congenital absence of six permanent teeth, not including the third molars. Patients need to be assessed for eligibility and registered with this program before their 18th birthday. Referrals can be made to Holland Bloorview Kids Rehabilitation Hospital for eligibility assessment of children who present with these criteria.
Dental Implants For Replacement Of Congenitally Missing Teeth
While most patients with oligodontia or hypodontia are diagnosed at a relatively early age, placement of dental implants cannot commence until it is absolutely certain that skeletal growth is complete. This can be a significant challenge in male patents that may exhibit late mandibular growth well in the early stages of their third decade of life. Performing surgery on a growing patient will, in almost all instances, result in inhibition of alveolar development, as the implant unit becomes an ankylosed tooth with all of the growth sequelae that were described in that section; the clinical manifestation of this is a submerging implant supported crown. In female patients, growth cessation, in general, is complete around 17 to 18 years of age; in males, one would assume that late growth is possible up to 20 years of age and beyond. A growth analysis consisting of serial lateral cephalometric analyses, performed at six-month intervals, is a useful tool in objectively determining an appropriate timeframe to initiate surgical therapy.
In most instances of congenital tooth absence, the surgeon can anticipate a variable degree of alveolar hypoplasia, and bone grafting is typically required (Figs. 23 & 24). The pathophysiology of this form of bone deficiency differs from bone resorption secondary to premature tooth loss, infection or trauma; in this scenario, the alveolar bone does not establish its full and normal volume due to lack of stimulation from failure of the permanent tooth to develop and erupt. Patients with oligodontia frequently require bone graft procedures to ensure adequate bone to support implants. The severity of alveolar hypoplasia may be greater in patients with ectodermal dysplasia or cleft lip and palate.
Figure 23

Non-syndromal oligodontia; note the severe alveolar hypoplasia, with bone deficiency at both the buccal and lingual aspects, in the second premolar sites.
Figure 24

Non-syndromal oligodontia with congenital absence of maxillary lateral incisors; significant underlying alveolar hypoplasia necessitating bone augmentation.
Dental implant supported habilitation of children with Trisomy 21 can be complicated by class II skeletal malocclusion, macroglossia with potentially severe tongue thrusting, as well as immune deficiency related to defects of polymorphonuclear leukocytes that are associated with the syndrome. Provision of deep sedation or general anesthesia for children with Down Syndrome is commonly challenging due to the presence of macroglossia, the potential for underlying obstructive sleep apnea, and the possibility of difficult airway management. Patients with this condition are also at risk for underlying atlanto-axial instability, and the cervical spine requires radiologic clearance pre-operatiavely.
The ectodermal dysplasias (ED) are a complex constellation of clinical findings. Severe oligodontia is highly prevalent. It has been estimated that 15% of patients missing eight or more permanent teeth have an underlying syndrome such as ED.5 ED is a syndrome characterized by malformations of tissues that are of ectodermal embryonic origin, including teeth, skin, nails, hair, and sweat glands. In the absence of classic features of hypohidrotic ED, it can be difficult to distinguish non-syndromal oligodontia from oligodontia associated with ED. This often requires medical clinical evaluation and genetic testing to obtain an accurate diagnosis. Dental implant therapy in patients with ED is highly complex due to the high number of missing teeth, lack of orthodontic anchorage, and the severe degree of alveolar hypoplasia (Figs. 25 & 26). In addidtion, many patients with hypohidrotic variants of ED carry methicillin resistant Staphylococcus aureus (MRSA) in the nares, with the consequence of inreased risk for bone graft and implant failure, and future peri-implantitis.
Figure 25

Ectodermal dysplasia; clinical appearance with retained primary teeth, severe oligodontia.
Figure 26

Implant habilitation in a patient with ectodermal dysplasia following bone augmentation with iliac crest grafts.
Conclusion
A wide range of clinical entities that may be encountered in the pediatric population has been reviewed. The importance of early recognition, accurate diagnosis and appropriate and timely treatment has been emphasized. The provision of oral surgical care to children requires that the clinician be trained and experienced in the recognition and significance of the dental, skeletal and physiologic differences that are essential to the provision of safe and successful treatment outcomes. OH
Oral Health welcomes this original article.
References
- Nishimura RA, Otto CM et. al: 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines
- Hulland SA, Freilich MM, Sandor GK. Nitrous Oxide-Oxygen Or Oral Midazolam For Pediatric Outpatient Sedation. Surg Oral Med Oral Pathol Oral Radiol Endod. 2002 Jun;93(6):643-6.
- Park MS, Sigal ML. The role of hospital-based dentistry in providing treatment for persons with developmental delay. J Can Dent Assoc. 2008 May;74(4):353-7
- Jastak, Yagiela, Donaldson: Local Anesthesia of the Oral Cavity: Saunders, 1995. Print.
- Carmichael RP, Sandor GS. Dental Implants in the Management of Nonsyndromal Oligodontia. Atlas Oral Maxillofacial Surg Clin N Am 16 (2008) 11- 31
- Kaban LB, Troulis MJ. Paediatric Oral and Maxillofacial Surgery: Saunders, 2004. Print. Barron RP, Freilich MM, Sandor GKB: Extraction Timing in Paediatric Odontogenic Infections (Ont Dent, Oct 2001, 15-18)
- Bouloux GF, Busily KF, BEirne OR, Chuang SK, Todson TB. What is the risk of future extraction of asymptomatic third molars? A systematic review. J Oral Maxillofac Surg. 2015 May;73(5): 806-11.
- Management of Impacted Teeth. American Association of Oral and Maxillofacial Surgeons White Paper, 2014.
- Dodson TB. Is there a role for reconstructive techniques to prevent periodontal defects after third molar surgery? J Oral Maxillofac Surg. 2005 Jul;63(7):891-6.
 Dr. Marshall Freilich is Coordinator of Oral and Maxillofacial Surgery at Holland Bloorview Kids Rehabilitation Hospital, and staff Oral and Maxillofacial Surgeon at Humber River Hospital and Baycrest Hospital. He maintains a private practice dedicated to surgical care for children and adults in Toronto, Ontario.
Dr. Marshall Freilich is Coordinator of Oral and Maxillofacial Surgery at Holland Bloorview Kids Rehabilitation Hospital, and staff Oral and Maxillofacial Surgeon at Humber River Hospital and Baycrest Hospital. He maintains a private practice dedicated to surgical care for children and adults in Toronto, Ontario.












