Our gut and oral cavity are home to the largest and second largest microbiomes, respectively, in the human body. Together, these microbiomes are intrinsically linked to our overall health in a complex relationship. While the presence of certain oral bacteria contribute to periodontal disease and tooth decay, these same bacteria may travel through our digestive track and alter the gut microbiome. Moreover, if our oral health is related to our gut health, and our gut health is related to overall health, it follows that it is important to maintain a healthy balance of microbiomes. Prebiotics may be an effective strategy to help to support the growth of our health-promoting bacteria in both the gut and oral microbiome.
What are prebiotics?
Prebiotics – naturally present in specific foods – can promote the growth of healthy bacteria in our bodies. Specifically, a prebiotic is a substrate that is selectively utilized by host microorganisms to confer a health benefit. Prebiotics resist hydrolysis by the enzymes that aid in digestion in the stomach and small intestine and continue to pass through to the colon. Here, they are fermented and increase the number of desirable bacteria in our microbiome. Many prebiotics are also considered to be a dietary fibre. Though not all fibres are a prebiotic – insoluble fibre (the type that adds bulk to your stool) is generally poorly fermented by our gut bacteria so it is not considered to be a true prebiotic. The most studied prebiotics are also types of soluble fibre and include inulin, galactooligosaccharides and fructooligosaccharides. Soluble fibre differs from insoluble fibre as it forms a gel with water that can trap certain food components and slows the digestion rate. On the other hand, insoluble fibre adds bulk to the stool and helps to move food more quickly through the stomach and intestine. Resistant starch and ß-glucan are also fibres that can be fermented by our gut bacteria. Many prebiotics exist making it hard to define them all, let alone remember their names. A good rule of thumb is that if its soluble fibre, it is a prebiotic. Lastly, prebiotics that are not a type of fibre have been more recently been identified. This includes polyphenols that are abundant in fruits and tea, and long-chain omega-3 fatty acids (EPA and DHA) that are present in fish. Examples of foods that contain prebiotics are shown in Table 1.
Table 1

Prebiotics and the oral microbiome
The original definition of prebiotics specified that they needed to modulate the composition of microbiome in the gut. However, this definition did not include prebiotics that were successful in modulating other microbiomes such as that in the vagina, skin or oral cavity.1 In fact, a prebiotic can target any microbiome in the body. More research is needed on this topic, but prebiotics may modify the oral microbiome if they are able to selectively stimulate the growth of bacteria that are associated with oral health.
Certain compounds have met the criterion to be considered a prebiotic. In vitro studies have demonstrated oral prebiotic candidates. Met-Pro, succinic acid, and N-acetyl-D-mannosamine were compounds that significantly increased the proportion of beneficial species and lowered the proportion of pathogenic species.2 While the literature is promising, these novel prebiotics are not found in foods at appreciable amounts. Futhermore, xylitol and arabinose may be able to stimulate the growth of certain lactobacilli, and these bacteria have an inhibitory effect against S. mutans, P. gingivalis and C. albicans; pathogens associated with dental caries, periodontal disease, and candidiasis, respectively.3 In the future, these prebiotic compounds may be manufactured into gums, lozenges, toothpastes, mouth rinses or chews. The key to creating oral prebiotics will be the ability of the prebiotic to remain in the oral cavity for a period of time to provide an opportunity for fermentation. Xylitol gum is already an available product on the market. It is thought that prevention of caries may happen when xylitol intake is 5 to 7 g per day, in multiple doses throughout the day.4 This can be achieved by chewing 2 tabs of gum made from xylitol, after breakfast, lunch and dinner. Of note is that more is not better as a higher than recommended intake of sugar alcohols can cause bloating, gas and diarrhea if consumed in excess.
How else do prebiotics relate to oral health?
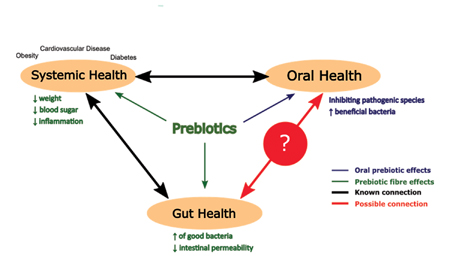
Though the concept of oral prebiotics needs more research, we can consider the ways prebiotics can help our oral health in an indirect way. For example, pathogens associated with periodontal disease may be capable of altering the gut microbiome. Specifically, P.ginigvalis, a pathogen implicated in periodontal disease, was found to provoke dysbiosis of the gut microbiome.5 Dysbiosis is a term used to describe when there is an imbalance in the microbial communities and this imbalance is often associated with disease. Gut dysbiosis has been observed in individuals suffering from chronic inflammatory conditions, including obesity, metabolic disorders and cardiovascular disease.6 Administration of prebiotics have been shown to counteract alterations in the gut microbiome which was correlated with improvements in energy intake, insulin resistance, satiety hormones, cholesterol and triglycerides, thus improving metabolic health.7 There is evidence that periodontal disease is also associated with shifts in the gut microbiome. In one study, individuals with periodontal diseases present a less diverse gut microbiome than individuals with periodontal health.8 Since periodontal disease is another chronic inflammatory disease associated with gut dysbiosis, could prebiotics also improve this condition? This begs the question; can changes in our gut microbiome improve our oral health?
Obesity and type 2 diabetes are well established risk factors of periodontal disease.9 These diseases are associated with chronic inflammation. Prebiotics can be helpful in the treatment plan of the diseases by targeting our gut microbiome to improve insulin resistance, preventing “leaky gut” and/or assisting with weight loss – all of which ultimately minimize the inflammatory response. As such, prebiotics may indirectly reduce the risk of periodontal disease by modifying risk factors: obesity, diabetes and chronic inflammation.
Figure 1 shows the relationship between our systemic, gut and oral health. Although it is unclear if changing our gut microbiome can influence our oral health, we know that our systemic conditions, such as obesity and diabetes, can have a negative impact on our oral health. Also, poor oral health is associated with systemic diseases such as cardiovascular disease, by triggering an inflammatory response.10 Prebiotics can alter our gut microbiome in a beneficial way that affects our systemic health, and by that, we may also support our oral health.
Fig. 1
Do prebiotics benefit oral health?
Since there are many different prebiotics, and the mechanism of action may vary, below are some general ways in which prebiotics may benefit oral health:
1. Prebiotics help prevent “leaky gut” and resultant inflammation
“Leaky gut” is a term used describe increased intestinal permeability where harmful substances are able to pass through the compromised intestinal wall and travel to other parts of the body. P.gingivalis has been shown to alter the gut microbiome and promote a “leaky gut” and these changes were attributed to an increased amount of toxins in the blood.5 These toxins promote inflammation by putting the body in a pro-inflammatory state. Bacteria produce short-chain fatty acids during fermentation of prebiotics and these products can help to improve intestinal barrier function and prevent harmful bacteria from crossing into the bloodstream and initiating this inflammatory response.11
2. Promote weight loss
Gut-secreted hormones related to satiety may be affected by prebiotic intake. Oligofructose, also known as fructooligosaccharides, has been shown to increase concentrations of GLP-1 and PYY. These hormones are regulators of appetite control and suppress energy intake. When participants were asked to consume 16 g of oligofructose a day for 13 days, energy intake significantly decreased.12 Decreasing energy intake will often lead to weight loss if energy intake is less than energy expenditure. Maintaining a healthy weight can reduce the risk for periodontal disease, as excessive fat tissue can secrete adipokines that increase systemic inflammation.9
3. Regulate blood glucose levels
Type 2 diabetes is a risk factor for periodontal disease.9,13 The risk of periodontal disease is even greater in patients with uncontrolled blood glucose levels. The relationship is bidirectional, as periodontal disease can also negatively impact blood glucose levels. Modifying the gut microbiome through prebiotics may help with insulin control. In one study, women with Type 2 diabetes taking a prebiotic (10 g of inulin/day) for 2 months showed significant decreases in fasting blood glucose and 3-month blood glucose levels.14 Regulation of blood glucose levels can help to either manage or reduce the risk of diabetes and further periodontal complications.
How do I increase my intake of prebiotics?
Because many types of prebiotics are also a type of fibre, increasing intakes of prebiotics can also help to reach recommended intake of fibre (or vice versa). In Canada, the recommended dietary intakes for fibre are 25 g for women and 38 g for men between the ages of 19-50 years old though actual intakes of fibre are often below this recommended level. The actual mean intakes were found to be markedly below these targets for Canadians; 19 g for men and 16 g for women.15 So what foods would need to be consumed to reach an intake of 25 or 38 g of fibre? Some examples are shown below:
- 1 serving of oatmeal (4 g of fibre)
- 1 tablespoon chia seeds (5 g of fibre)
- ½ cup raspberries (4 g of fibre)
- 1 cup of cooked broccoli (4 g of fibre)
- 1 cup of quinoa, (6 g of fibre)
- ¼ cup almonds (4 g of fibre)
- ½ cup lentils (8 g of fibre)
Canada’s new food guide targets the fibre gap, by encouraging the consumption of more plant-based proteins, fruits and vegetables, and whole-grains.16 Ideally, half of each meal should be made up of fruits and vegetables and whole-grains should occupy another quarter. The rest of the plate may be comprised of plant-based proteins, such legumes and lentils, as these foods have both substantial amounts of protein and fibre, making them efficient foods on an energy basis.
Although there is currently no guidelines on prebiotic intake in Canada, the European Union has an accepted health claim for prebiotics that consumption of 12 g of “native chicory inulin” a day “contributes to maintenance of normal defecation by increasing stool frequency.”17 While prebiotics fibres are found naturally in foods (Table 1), they can be used as fat or sugar replacements and are added to various processed foods such as baked goods, cereals, cereal bars, ice cream and desserts. However, just because a product is formulated with prebiotics, does not mean it is healthy. Consuming whole foods is encouraged over highly processed foods as whole foods contain many other healthy components such as vitamins and minerals. Processed foods often contain unnecessary amounts of added sugar, salt and fat. This is further justified by a systematic review with a meta-analysis that showed that consuming 5 or more servings of fruits and vegetables per day may prevent tooth loss and the progression of periodontal diseases.18 In other words, think twice about choosing a granola bar rather than an apple.
Some individuals may choose to use a supplement rather than foods to increase prebiotic intake. Though, consuming a large amount of prebiotics in a supplement may lead to gastrointestinal side effects such as bloating, gas and cramping. Bacteria produce gas when they metabolize these food components, along with their helpful short-chain fatty acids. However, these side effects will subside as regular consumption of prebiotics can shift microbiota metabolism toward low gas producing pathways.19 Starting with the consumption of a small supplement dose and gradually increasing the level after a few weeks can help to mitigate these side-effects. Ensuring adequate consumption of fluids is also imperative to avoid constipation as fibre traps water with it as it travels through the digestive system.
Key points for dental health professionals & patients:
- Encourage patients to eat a diet rich in prebiotics by following Canada’s Food Guide (https://food-guide.canada.ca/en/) that encourages the consumption of proteins, particularly plant-based (1/4 of your plate), whole grains (1/4 of your plate) and fruits and vegetables (1/2 of your plate).
- Increase consumption of prebiotics from whole foods such as fruits, vegetables and whole grains. Whole foods are also rich in amino acids, vitamins, minerals, fatty acids and other nutrients. Processed foods often contain unhealthy amounts of sugar, sodium and fat.
- Polyphenols (particularly abundant in berries and tea) and omega-3 fatty acids (specifically EPA and DHA, found in fish oil) are not fibre but have been shown to have prebiotic properties and may also have anti-inflammatory effects. So be sure to consume foods containing these components.
- Prebiotic supplements are available over-the counter and can be used to ensure a recommended intake of fibre if it is too challenging to consume these levels via food.
- When starting to take a prebiotic fibre supplement, slowly increase the dose per day to reduce the chance of gastrointestinal distress. Alternatively, split the dosage up into multiple dosages and consume at different times during the day.
- Make sure to increase water consumption with increased fibre consumption.
Bottom Line
Increasing your intake of prebiotic fibre – whether it be by following Canada’s Food Guide to increase the intake of the foods mentioned and/or by taking a supplement – will help to support overall health and may reduce your risk for periodontal disease and oral caries.
Oral Health welcomes this original article.
References
- Gibson, G. R., et al. (2017). Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nature Reviews Gastroenterology & Hepatology, 14(8), 491–502. https://doi.org/10.1038/nrgastro.2017.75
- Slomka, V., Herrero, E., Boon, N., Bernaerts, K., Trivedi, H., Daep, C., Quirynen, M., & Teughels, W. (2018). Oral prebiotics and the influence of environmental conditions in vitro. Journal of Periodontology, 89(6), 708–717. https://doi.org/10.1002/JPER.17-0437
- Kojima, Y., Ohshima, T., Seneviratne, C. J., & Maeda, N. (2016). Combining prebiotics and probiotics to develop novel synbiotics that suppress oral pathogens. Journal of Oral Biosciences, 58(1), 27–32.
- Nayak, P. A., Nayak, U. A., & Khandelwal, V. (2014). The effect of xylitol on dental caries and oral flora. Clinical, cosmetic and investigational dentistry, 6, 89–94. https://doi.org/10.2147/CCIDE.S55761
- Nakajima, M., Arimatsu, K., Kato, T., Matsuda, Y., Minagawa, T., Takahashi, N., Ohno, H., & Yamazaki, K. (2015). Oral administration of P. gingivalis induces dysbiosis of gut microbiota and impaired barrier function leading to dissemination of enterobacteria to the liver. PloS one, 10(7), e0134234. https://doi.org/10.1371/journal.pone.0134234
- Carding, S., Verbeke, K., Vipond, D. T., Corfe, B. M., & Owen, L. J. (2015). Dysbiosis of the gut microbiota in disease. Microbial Ecology in Health and Disease, 26, 26191. https://doi.org/10.3402/mehd.v26.26191
- Parnell, J. A., & Reimer, R. A. (2012). Prebiotic fiber modulation of the gut microbiota improves risk factors for obesity and the metabolic syndrome. Gut Microbes, 3(1), 29–34. https://doi.org/10.4161/gmic.19246
- Lourenço, T., Spencer, S. J., Alm, E. J., & Colombo, A. (2018). Defining the gut microbiota in individuals with periodontal diseases: an exploratory study. Journal of Oral Microbiology, 10(1), 1487741. https://doi.org/10.1080/20002297.2018.1487741
- Levine, R. S. (2013). Obesity, diabetes and periodontitis – a triangular relationship? British Dental Journal, 215(1), 35–39. https://doi.org/10.1038/sj.bdj.2013.627
- Kane S. F. (2017). The effects of oral health on systemic health. General dentistry, 65(6), 30–34.
- Cani, P. D., Possemiers, S., Van de Wiele, T., Guiot, Y., Everard, A., Rottier, O., … Delzenne, N. M. (2009). Changes in gut microbiota control inflammation in obese mice through a mechanism involving GLP-2-driven improvement of gut permeability. Gut, 58(8), 1091 LP-1103. https://doi.org/10.1136/gut.2008.165886
- Verhoef, S. P., Meyer, D., & Westerterp, K. R. (2011). Effects of oligofructose on appetite profile, glucagon-like peptide 1 and peptide YY3-36 concentrations and energy intake. British Journal of Nutrition, 106(11), 1757–1762. https://doi.org/10.1017/S0007114511002194
- Preshaw, P. M., Alba, A. L., Herrera, D., Jepsen, S., Konstantinidis, A., Makrilakis, K., & Taylor, R. (2012). Periodontitis and diabetes: a two-way relationship. Diabetologia, 55(1), 21–31. https://doi.org/10.1007/s00125-011-2342-y
- Gargari, B.P., Dehghan, P., Aliasgharzadeh, A., & Jafarabadi, M.A. (2013). Effects of high performance inulin supplementation on glycemic control and antioxidant status in women with type 2 diabetes. Diabetes & Metabolism Journal, 37, 140 – 148.
- Bélanger, M., Poirier, M., Jbilou, J., & Scarborough, P. (2014). Modelling the impact of compliance with dietary recommendations on cancer and cardiovascular disease mortality in Canada. Public Health, 128(3), 222–230. https://doi.org/10.1016/j.puhe.2013.11.003
- Health Canada. (2019). Canada’s Food Guide. Available at: https://food-guide.canada.ca/en/.
- EFSA Panel on Dietetic Products. (2015). Scientific Opinion on the substantiation of a health claim related to “native chicory inulin” and maintenance of normal defecation by increasing stool frequency pursuant to Article 13.5 of Regulation (EC) No 1924/2006. EFSA Journal, 13(1), 3951. https://doi.org/10.2903/j.efsa.2015.3951
- Skoczek-Rubi´nska, A., Bajerska, J., & Menclewicz, K. (2018). Effects of fruit and vegetables intake in periodontal diseases: A systematic review. Dental and Medical Problems, 55(4), 431–439. https://doi.org/10.17219/dmp/99072
- Mego, M., Accarino, A., Tzortzis, G., Vulevic, J., Gibson, G., Guarner, F., & Azpiroz, F. (2017). Colonic gas homeostasis: Mechanisms of adaptation following HOST-G904 galactooligosaccharide use in humans. Neurogastroenterology and Motility, 29(9), 10.1111/nmo.13080. https://doi.org/10.1111/nmo.13080
About the Author
 Carly Zanatta holds a BSc in food science from the University of Guelph and her current thesis research expands on her knowledge of foods as she is investigating the relationship between prebiotic intake and periodontal health. Carly is a MSc candidate in Applied Health Sciences at Brock University.
Carly Zanatta holds a BSc in food science from the University of Guelph and her current thesis research expands on her knowledge of foods as she is investigating the relationship between prebiotic intake and periodontal health. Carly is a MSc candidate in Applied Health Sciences at Brock University.
 Wendy Ward is a Professor and Canada Research Chair in the Department of Kinesiology in the Faculty of Applied Health Sciences at Brock University. Her research team investigates how diet supports a healthy skeleton as well as healing after periodontal procedures within preclinical and clinical studies.
Wendy Ward is a Professor and Canada Research Chair in the Department of Kinesiology in the Faculty of Applied Health Sciences at Brock University. Her research team investigates how diet supports a healthy skeleton as well as healing after periodontal procedures within preclinical and clinical studies.












