Keywords:
Palatal constriction
Maxillary constriction
Segmented Lefort 1 osteotomy
Maxillary expansion
Palatal expansion stability
INTRODUCTION:
Insufficient transverse palatal dimension is a major component of several types of malocclusion.1 This skeletal anomaly is rarely isolated. Most of the time it is in association with a problem of vertical maxillary excess, a mandibular retrognathism or, more rarely, a mandibular prognathism, a retrusive chin and a labial incompetence. It is frequently described as the “Long face syndrome” (Figs. 1A & 1B)
Fig. 1A

Fig. 1B

Fig. 1C

Fig. 1D

Fig. 1E

Fig. 1F

Fig. 1G

Fig. 1H

Fig. 1I

Traditional orthodontic treatment with orthognathic surgery has become the standard procedure for correcting these anomalies in adults.2-4 Unfortunately, presurgical orthodontic treatment, with a continuous wire, to correct dental arch alignment can be inappropriate for patients with severe malocclusion and a narrow palate. Orthodontic expansion of the maxillary dental arch in conjunction with an insufficient maxillary width of the skeleton must unavoidably lead to displacement of the dental roots out of the medulla into the labial and buccal cortex. This abnormal position of the dental roots in the alveolar bone, frequently observed during the orthognathic surgery, is considered by the author as a possible strong contributor for the relapse noticed when one does a multi-piece Lefort 1 osteotomy with palatal expansion.5
Segmentation of the maxilla for a palatal expansion with a three-piece Lefort 1 osteotomy has been used extensively for patients with an insufficient transverse palatal dimension but that segmentation is usually done just prior to the orthognathic surgery, once the typical arch coordination has been performed by the orthodontist .
To keep the dental roots in a better position in the alveolar process, the author uses a concept of presurgical maxillary segmented orthodontics (PMSO). The presurgical orthodontic alignment by segments is done right at the beginning of the treatment with the objective of keeping a better and more physiologic position of the roots in the alveolar process.
This retrospective longitudinal study is about this concept and shows the results of 15 patients, suffering a palatal constriction, treated with this approach.
MATERIALS AND METHODS
In this retrospective longitudinal study, patients with a palatal constriction were included (at least 3.1 mm in the cuspid and/or second molar region). All these patients had at least one posterior crossbite before the orthodontics. They all presented the “Long face syndrome”. Patients with other syndromes and cleft palates were excluded.
Due to the retrospective nature of this study, it was granted an exemption in writing by the “Centre intégré de santé et de services sociaux de l’Outaouais” institutional review board. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
A continuous series of fifteen patients treated by the author, with an insufficiency of their palatal transverse dimension, were recruited for this retrospective longitudinal study. It spanned a 4-year period between 2014 and 2018. Of these patients 10 were female and 5 were male.
For all patients a presurgical orthodontic treatment with a segmented orthodontic wire on the maxilla and a continuous wire on the mandible was performed. These maxillary segmentations of the orthodontic wire were done between the lateral incisor and canine on both sides. Then a 3-piece Lefort 1 osteotomy with a bilateral sagittal split osteotomy of the mandible and a genioplasty were accomplished. The Lefort 1 osteotomy was done without the use of an osteotome in the pterygomaxillary region as described by Precious et al.6,7
The palate was cut with a U-shaped osteotomy making sure not to damage the palatal tissue. Then the interdental regions (between lateral incisor and cuspid) were osteotomized with a bur cutting only the labial cortex. Thereafter, once the maxilla was down fractured, the palatal bone of these areas was also osteotomized with a bur. No bur or chisel was used between the dental roots. The split in these sites was obtained simply by creating a fracture of the bone between each root. Then the expansion of the lateral segments was obtained manually. The segments were positioned in a prefabricated splint and stabilised with wires.
The maxilla was repositioned and rigidly fixed with two miniplates on each side. Postoperatively, moderately strong elastics for intermaxillary stabilisation were used in intermittence between the meals. After seven weeks, the intermaxillary stabilisation was kept only during the night and patients were allowed to chew food. The splint was kept in place and removed after 11 weeks. Thereafter, patients were referred to the orthodontist to complete the treatment.
All patients consented to radiographs, dental impressions for plaster models and bite registration. Palatal width dimensions, in the canine and second molar regions, were collected in three phases of treatment: TPD1: transverse palatal dimension of the preoperative study model at the end of the presurgical maxillary segmented orthodontic alignment, TPD2: transverse palatal dimension as planned on the modified preoperative study model for the orthognathic surgery and fabrication of the surgical splint (corresponding to the immediate post-op expansion), TPD3: transverse palatal dimension of the follow-up study model. To make the measurements of the palatal width dimensions on the different models, the author first determined a landmark that could be easily identified on each of the three models of the same patient, like the tip of a particular cuspid. These landmarks were different for each patients but gave a good and precise evaluation of the palatal width for each of them, in the cuspid or second molar area, for the three phases of treatment previously described.
The average period between the surgery and the taking of post-op plaster models was 29 months (10-56 months). All measurements were registered with an electronic calliper and noted with a 0.1 mm precision.
RESULTS
Table I shows for each of these patients (in the canine and second molar regions): Age at surgery, follow-up period (months), TPD1, TPD2, surgical expansion, TPD3, relapse of the transverse width and percentage of this relapse.
Table I: Transverse palatal dimensions, expansions and relapses

TPD1: transverse palatal dimension of the preoperative study model at the end of the presurgical maxillary segmented orthodontic alignment. TPD2: transverse palatal dimension as planned on the modified preoperative study model for the orthognathic surgery and fabrication of the surgical splint (corresponding to the immediate post-op expansion). TPD3: transverse palatal dimension of the follow-up study model.
The mean age of the patients was 30 years old (17-42 years old). The follow-up plaster model impressions have been taken between 10 and 56 months after the surgery with an average period of 29 months.
The final expansion obtained in the canine region has been between 3.1 and 8.7 mm with an average of 5.55 mm. In the molar region it has been between 0 and 9.1 mm with an average of 3.95 mm.
The percentage of relapse of the expansion has been 6.7% in the canine region for a mean expansion of 5.55 mm and 3.8% in the second molar region for a mean expansion of 3.95 mm.
It is worth specifying that case #6, with a cuspid expansion of 8.7mm, showed only 16.1% relapse. Also case #12, with a second molar expansion of 9.1mm, showed only 14% relapse.
DISCUSSION
Insufficient transverse palatal dimension is a frequent component of patients requiring orthognathic surgery.1
Orthodontic rapid palatal expansion is widely used with children to correct the transverse palatal constriction but doesn’t work when the sutures have fused at the end of growth which typically occurs in girls at a mean age of 11 years and in boys at a mean age of 13 years.8,9
Traditional orthodontic treatment, using a maxillary continuous wire, with orthognathic surgery has become the standard procedure for correcting these anomalies in adults.2-4 Proffit and Turvey in 1996 published research about a hierarchy of stability in orthognathic surgery. Transverse palatal expansion of the maxilla would be the most unstable orthognathic procedure. The greatest relapse is seen in the second molar region with an average of 50% loss of surgical expansion, 1 year post surgery. More than 2 mm of relapse was lost on average for a mean expansion of 2 mm in the canine region and 5.8 mm in the second molar region.10 In 2015 Brandtner et al. published a study showing a relapse of about 60% of the surgically expanded transverse width which was on average enlarged by 2.7 mm.5 In 2011 Kretschmer et al. evaluated 87 patients undergoing bimaxillary osteotomies with 3-piece Lefort 1 osteotomy. The mean expansion of the entire sample was 2.13 mm at the skeletal base, 1.11 mm in the premolar region, and 1.99 mm in the molar region. Mean relapses of 9% at the skeletal base, 68% in the premolar region, and 60% in the molar region were observed. They concluded that surgical expansion of the maxilla provides stable results at the maxillary skeletal base but high relapse rates in the dentoalveolar area. Preoperative orthodontic expansion was considered one of the main sources of transverse relapse.11 There is no doubt that preoperative orthodontic treatment with correct dental arch alignment is challenging for patients with severe malocclusion and a narrow palate. Orthodontic expansion of the maxillary dental arch, with a continuous wire, in conjunction with an insufficient maxillary width of the skeleton must lead unavoidably to displacement of the roots out of the maxillary bone into the labial and buccal cortex. Then, with such an orthodontic preparation, when one does a multi-piece Lefort 1 osteotomy with palatal expansion, the abnormal position of the dental roots in the alveolar process is probably a strong contributor to explain the well-known relapse.
The concept of PMSO is quite simple. In the course of the presurgical orthodontic alignment, it is mandatory to keep the roots of all the maxillary teeth right in the medulla of the alveolar process between the cortexes. To do so, the orthodontist must work with a segmented orthodontic wire in the maxilla right at the beginning of the treatment. If this wire is segmented, in the areas between the lateral incisor and cuspid on both sides of the maxilla, one avoids any transverse orthodontic force on these teeth. Cuspid to second molar on each side get themselves a mid-position in their alveolar process because the left and right sides of the maxilla are not interconnected. The mandibular dental arch must be aligned as usual, using a non-segmented orthodontic wire.
During the period of the presurgical maxillary segmented orthodontic alignment, without any expansion force, the teeth of the lateral segments of the maxilla must move themselves to a mid-position in the alveolar process. As seen on a series of clinical views of a patient treated with this concept, (Fig. 1) the cuspids and premolars often get posterior and palatal to the lateral incisors. (Figs. 1E & 1F) At that stage of treatment, the lateral alveolar processes on both sides of the maxilla are still narrow and this dental positioning is totally normal and desirable to keep dental roots between both cortexes. Such a position of the teeth on the maxillary dental arch is, de facto, a good clinical demonstration of the absence of dentoalveolar expansion.
The osteotomy, between the lateral incisor and the cuspid, is rarely a problem if one uses the surgical technique previously described. Once these osteotomies are completed, one proceeds with the expansion of the lateral segments. Because these osteotomies are oblique, the expansion of the segments is more a “sliding movement” rather than a pure separation. (Fig. 2)
Fig. 2
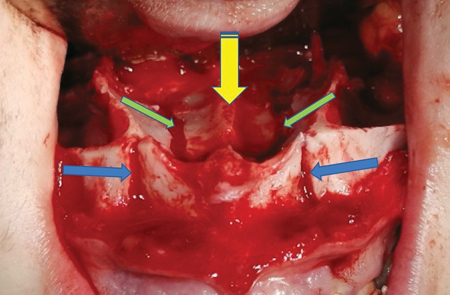
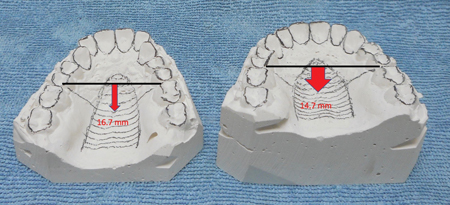
With such a technique using a U-shaped osteotomy, the palatal expansion is obtained by separation in two sites. A likely lower displacement of the mid-part of the palate would also contributes to the expansion of the palate. (Fig. 2) That is why the palatal shape of these patients goes from ogival (Fig. 3 left) to normal. (Fig. 3 right)
Fig. 3
CONCLUSION
This retrospective longitudinal study, concerning PMSO with orthognathic surgery, has shown a high stability level for the expansion of the maxilla. The 6.7% relapse observed in the canine region for a mean expansion of 5.55 mm, and 3.8% in the second molar region for a mean expansion 3.95 mm, suggest much better results than traditional orthodontics, using a maxillary continuous wire, with orthognathic surgery.
For the author, PMSO with orthognathic surgery appears to be appropriate to deal with most cases of insufficient transverse palatal dimension and the many stigmas of the “Long face syndrome”. The author thinks that it is also a logical and convenient way of treating an insufficient transverse palatal dimension, and the associated deformities, with only one surgery.
Obviously, a larger series of cases treated this way, with similar results, would give more support to this concept.
Special thanks to Mr. Steven Dunn and Dr. Johanne Saucier for their help with the writing of this paper. Oral Health welcomes this original article.
References
- Suri L, Taneja P: Surgically assisted rapid palatal expansion: A litterature review. Am J Orthodont Dentofac Orthoped 133:290-302, 2008.
- De Lir Ade L, de Moura WL, Oliveira Ruellas AC, et al.: Long-term skeletal and profile stability after surgical-orthodontic treatment of Class II and Class III malocclusion. J craniomaxillofac Surg 41(4):296-302, 2013.
- Csaszar GR, Niederdellmann H: Reliability of bimaxillary surgical planning with the 3-D orthognathic surgery simulator. Int J Adult Orthod Orthognath Surg 15(1):51-58, 2000.
- De Haan IF, Ciesielski R, Nitsche T, et al.: Evaluation of relapse after orthodontic therapy combined with orthognathic surgery in the treatment of skeletal Class III. J Orofac Orthop 74(5):362-369, 2013.
- Brandtner C, Hachleitner J, Rippel C, et al. : Long-term skeletal and dental stability after orthognathic surgery of the maxillo-mandibular complex in Class II patients with transverse discrepencies. J Craniomaxillofac Surg 43:1516-1521, 2015.
- Precious DS, Ricard D: Modification de l’osteotomie de Lefort I: Disjonction pterygo-maxillaire par bascule inférieure du maxillaire superieur. Rev Stomatol Chir Maxillo-fac 89(5):288-292, 1988.
- Precious DS, Morrison A, Ricard D: Pterygomaxillary separation without the use of an osteotome. J Oral Maxillofac Surg 49(1): 98-9, 1991.
- Menon S, Manerikar R, Sinha R: Surgical management of transverse maxillary deficiency in adults. J Maxillofac Oral Surg 9: 241, 2010.
- Angelieri F, Franchi L, Gonçalvez JR, et al.: Midpalatal suture maturation: classification method for individual assesment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop 144:759, 2013.
- Proffit W, Turvey TA, Phillips C: Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodont Orthognath Surg 11: 191-204, 1996.
- Kretschmer WB, Baciut G, Baciut M, et al.: Transverse stability of 3-piece Lefort 1 osteotomies. J Oral Maxillofac Surg 69(3):861-9, 2011.
About the Author
 Dr. Daniel Ricard is an oral and maxillofacial surgeon. He is in private practice in Gatineau (Québec). Dr. Ricard studied dentistry at “Université de Montréal”, completed a multidisciplinary program in dentistry at “McGill University” and next a program in oral and maxillofacial surgery at “Université Laval”, in 1987. Then he went for a fellowship in orthognathic surgery with Professor Jean Delaire in Nantes (France) and Professor David Precious at “Dalhousie University”. Dr. Ricard is Fellow of the RCDC and has been examiner for the fellowship exam for 15 years. Dr. Ricard has lectured nationally and internationally. Contact: dr.danielricard@gmail.com.
Dr. Daniel Ricard is an oral and maxillofacial surgeon. He is in private practice in Gatineau (Québec). Dr. Ricard studied dentistry at “Université de Montréal”, completed a multidisciplinary program in dentistry at “McGill University” and next a program in oral and maxillofacial surgery at “Université Laval”, in 1987. Then he went for a fellowship in orthognathic surgery with Professor Jean Delaire in Nantes (France) and Professor David Precious at “Dalhousie University”. Dr. Ricard is Fellow of the RCDC and has been examiner for the fellowship exam for 15 years. Dr. Ricard has lectured nationally and internationally. Contact: dr.danielricard@gmail.com.












