Introduction
Implant therapy has been shown to be predictable, effective and reliable for the replacement of missing teeth in edentulous and partially edentulous patients. Clinical evidence has demonstrated long-term (>10 years) survival rates up to 95% (Moraschini et al., 2015). Despite the high success and survival rates of dental implants, failures can and do occur. The cause of failures can be multifactorial and include biological, technical, esthetic, surgical, and prosthetic complications. There are certain factors and behaviours such as heavy smoking, bruxism, and history of periodontal disease which have been associated with higher rates of implant failure (Chrcanovic et al., 2014; Sgolastra and Petrucci, 2015; Zhou et al., 2016). Furthermore, implant site characteristics such as decreased quantity and/or quality of bone, infected sites, and anatomic locations such as the posterior maxilla have also been correlated to decreased implant survival (Manzano et al., 2016; Zhao et al., 2016). Technical factors involving placement techniques and protocols such as antibiotic use (or lack thereof), surgical experience of the operator, and increased numbers of implants placed at a single session have been associated with increased implant failure rates (Ata-Ali et al., 2014; Jemt, 2017a; Jemt, 2017b).
If an implant fails, all measures must be taken to determine the potential cause(s) of failure as this will significantly influence the formulation of a new treatment plan which must also address the specific needs and concerns of the patient. Several options exist for replacement of a failed implant. These include reimplantation therapy, a fixed partial denture, a removable partial denture, or no additional treatment with considerations given to maintaining the health of the edentulous space. Typically, reimplantation is the favored option as it allows for execution of the original prosthetic treatment plan. However, sites of previous implant failure might be less than ideal for implant placement owing to compromised bone quality and quantity. Dental implants placed in sites of previous failure have been shown to have lower success and survival rates than those of initial placement however there is much variation in the reported data. Machtei et al. (2008) reported a survival rate of 83.5% in a study that followed 79 replacement implants. Machtei et al. (2011) further demonstrated that implants replaced on the third attempt had a significantly lower survival rate of only 60%. However, Mardinger et al. (2012) found a survival rate of replacement implants at 93% with a third replacement in the same sites yielding a survival rate of up to 85%. Grossman and Levin (2007) reported an overall survival rate of 71% of implants in previously failed sites. In a recent systematic review by Zhou et al. (2016) that evaluated the feasibility of dental implant replacement in failed sites, it was shown that the mean survival rate for implant replacement was 88.84% and 74.19% for second and third replacements, respectively. Clearly, the evidence demonstrates decreased implant survival rates with subsequent reimplantation attempts however, the survival rates are still high enough so as not to discourage clinicians from reattempting implantation in previously failed sites.
This article presents 3 cases of initial implant failures with successful reimplantation therapy with long-term follow up.
Case #1
A 29-year-old female, with no contributory medical history and allergy to penicillin presented for orthodontic treatment wanting to correct the position of her teeth. Her dental history indicated that tooth 43 was impacted and extracted several years prior to her consult with our office.
Orthodontic Assessment: Skeletal Class 1 pattern with normal maxillo-mandibular relationship. Patient had an average vertical pattern with normal lower facial height. Dental Class 1 malocclusion with moderate upper anterior crowding. Missing 43, collapsed lower anterior segment. Lower midline shifted to the right by 3 mm with slightly increased overjet. Orthodontic treatment was undertaken with the use of fixed upper/lower straight wire appliance. Treatment was completed in 18 months and patient placed in retention. The upper and lower anterior teeth were up righted, midlines corrected, and sufficient space created to replace the 43 with an implant.
Pre-Treatment Implant Assessment: Stable periodontium, localized pocket depths of 4mm in the molar regions in all four quadrants. Evaluation of interdental space between 42 and 44 demonstrated an inter coronal width of 5mm and interradicular width of 7mm with a localized bony defect. (Fig. 1)
Fig. 1

Implant Surgery: A surgical guide was fabricated, and Stage 1 surgery was performed by an oral surgeon at an external office. In April 2002, a narrow platform Tiunite MK III Branemark 15mm in length was placed simultaneously with autogenous bone from the osteotomy site and bone graft substitute material. Shortly after, following mucosal dehiscence on the crestal and labial aspects of the ridge and repeated infection at the site indicating early failure, the implant was removed. In December 2002 a second narrow platform Branemark MKIII measuring 13mm in length was placed in the same site simultaneously along with autogenous bone material harvested from the maxillary tuberosity. Although the surgeon noted ‘excellent primary stability’ during surgery, this second implant was removed after the implant came loose a few weeks later. (Figs. 2,3)
Fig. 2

Fig. 3

Re-treatment Assessment: After two repeated surgical failures, the options for replacement were discussed. These included a Maryland bridge, removable denture, tooth supported fixed bridge and re treatment with an implant supported fixed prosthesis. Site 43 demonstrated a significant bony defect and bone loss distal to 42. The patient was keen to replace the missing 43 with a fixed prosthesis. Having discussed the risks and disadvantages of the tooth supported fixed bridge including the risk of damage to the adjacent teeth, loss of attachment relative to 42 rendering it a poor abutment, possible loss of pulp vitality and the difficulty associated with cleaning the intaglio surface of the long pontic, the patient was keen to proceed for a second opinion regarding replacement of 43 with an implant supported crown.
In June 2003 a surgical stent incorporating a guide cylinder was fabricated after a diagnostic wax up and a third Implant (3i Osseotite Micro mini-implant 3.25x13mm) was placed in the 43 site. in October 2003, after verifying integration of the implant, the patient was ready to commence the prosthetic phase of the treatment. (Fig. 4)
Fig. 4

Prosthetic Procedures: were commenced and completed in March 2004. A custom abutment was inserted and torqued to 20Ncm. The access to the implant sealed with a cotton pellet and composite resin. A porcelain bonded to metal crown tried in. The fit of the crown on the abutment was verified to be passive, inter-proximal contacts verified to be positive and the crown was cemented with temp bond. All excess cement was removed, and occlusion checked to ensure no contact in centric and eccentric movements. (Figs. 5,6,7)
Fig. 5

Fig. 6

Fig. 7

Follow up: To date, the patient has been seen regularly for follow up since crown insertion. In 2014, when occlusion with the opposing tooth was noted as positive with shim stock, the occlusal contact was reduced, and the patient was advised that we would continue to monitor the occlusal contact and its effects if any on the underlying bone. (Figs. 8,9)
Fig. 8

Fig. 9

Case #2
A 70-year-old female patient presented in August of 2017 with a missing 23 with wanting to replace the tooth with an implant supported fixed prosthesis. Her dental history revealed that tooth 23 was previously extracted in February 2017 while she was living in the USA. She reported no complications with healing after extraction. Previous history of socket preservation or grafting was unknown. Her medical history was non-contributory, she was a non-smoker and reported a history of a left hip replacement approximately 10 years ago.
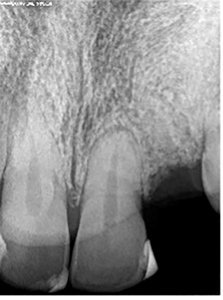
Pre-Treatment Assessment: indicated an extensively restored dentition, a stable periodontium with good healing of the 23-extraction site, adequate buccal (B), palatal (P), mesial (M) and distal (D) bone and adequate interocclusal clearance. The periapical radiograph showed good bone height and adequate interradicular distance between 22 and 24. (Figs. 1,2) After this initial assessment and discussion of treatment options, the patient elected to replace the missing 23 with an implant supported fixed restoration, the prognosis of which was assessed to be favorable. The surgical and prosthetic protocols were discussed, and informed consent was obtained after a discussion of treatment alternatives and cost. Impressions were made with Alginate material (Jeltrate® Chroma) using a stock tray and a surgical guide fabricated.
Fig. 1

Fig. 2

Implant Surgery: was performed in September 2017. Local anesthesia was achieved with 1.8 cc Lidocaine (Lido) 2% 1:100K Epinephrine (Epi) for buccal and palatal infiltration(B/P) and UltracaineR 4% 1:200K Epi. A full thickness flap was raised on the buccal and palatal surfaces with conservative papilla sparing incisions on the buccal. The osteotomy was prepared for a Straumann® Bone Level SLA® 3.3×10 mm NC implant fixture. Good primary stability was achieved, a cover screw was placed, and the implant was submerged for protected healing. Saline irrigation was done throughout the surgery and the site was closed with resorbable 5-0 chromic gut sutures. Hemostasis was achieved and the patient was dismissed after reviewing post operative care instructions. (Fig. 3) A prescription was given for Amoxicillin 500 tid for 7days and Toradol 10 mg tid prn pain (x20 tabs). The patient was seen 2 weeks post operatively and the site was observed to be healing. She was further seen for a 2 month post operative recall (December 2017) during which time she reported no complaints and tissue healing appeared to be proceeding well.
In January 1018, the submerged fixture was exposed. Local anesthetic was achieved using 1.8 cc Lido 2% 1:100K Epi for B/P infiltration. A full thickness flap was elevated, and a significant bony fenestration was seen on the buccal aspect of the implant; torque testing of implant was positive for 35 Ncm. (Fig. 4) Axenogeneic ossifying collagen scaffold (Ossix® Volumax) was placed on the buccal aspect and tension-free primary closure was achieved using interrupted resorbable 5-0 chromic gut sutures. After achieving hemostasis, the patient was given a prescription for Amoxicillin 500 tid for7days and OTC(over the counter) analgesia. The patient was seen post operatively 3 weeks later, and healing was uneventful.
Fig. 3

Fig. 4

After allowing a healing period of close to four months, in May 2018, Stage 2 surgery was re-attempted. Local anesthesia was achieved using the protocol described above. A full thickness flap was elevated buccally and palatally. The implant fixture was reverse torque tested to 35 Ncm successfully and deemed to be integrated. (Fig.5) Post-operative instructions were reviewed, and the patient was scheduled to commence prosthetic procedures.
Fig. 5

Prosthetic procedures were commenced after a 5-week healing period following Stage 2 surgery, to fabricate a screw retained implant crown. Over the course of the next 3 weeks, a final impression was made using an open tray style impression coping with a custom tray and Flexitime® impression material. Subgingival decay was noted on the 24 mesial, decay was excavated and restored with Ketac™ Nano. A one-piece UCLA abutment and porcelain bonded to metal crown (PBM) were tried in. In July 2018, on the day of insertion, the patient reported soreness in the 23 area. The gingiva appeared mildly inflamed suggestive of trauma. The healing cap was removed, and the implant abutment/crown complex was seated. It was checked to ensure there was no occlusion in maximum intercuspation. During the process of torquing the screw of the implant crown to 32 Ncm, the crown rotated 180 degrees, indicating a loss of implant integration. Under local anesthesia 1.8 cc Lido 2% 1:100K Epi for B/P infiltration, the implant was removed by using the torque wrench in reverse mode. The site was irrigated with saline and allowed to heal. (Fig. 6)
Fig. 6

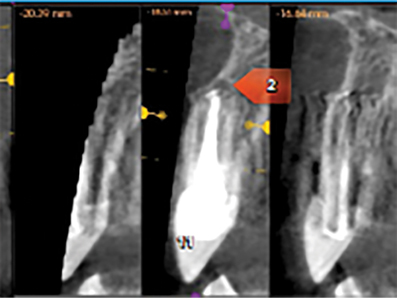
A CBCT done in September 2018 and revealed a knife edge ridge in the 23-site requiring GBR (guided bone regeneration) and periapical rarefying osteitis around 11,22,24, teeth which were previously endodontically treated. (Figs. 7,8,9). After an endodontic consult, a diagnosis of acute apical periodontitis was made, and treatment options for these teeth presented to the patient that included- re treatment, extraction or apicoectomy. Three months post implant removal under coverage of premedication (Amoxicillin 500mg tid for 2 days) apicoectomy of 22 and 24, in combination with periodontal surgery (GBR) was performed. Local anesthesia (LA) was achieved with 1.5 carps Lido 2%, 1:100K Epi and 2 carps Ultracaine 4% 1:200K Epi. A full thickness flap elevation (FTF) was done on the buccal and palatal aspects with remote vertical releases on the buccal for access to GBR on site 23. Apicoectomy was performed in 22/24 with ultrasonic root end preparation and filled with MTA (mineral trioxide aggregate). A significant vertical defect was seen in the 23 site with loss of buccal and palatal bone walls but the proximal walls were intact. For the cortical perforations; a composite mixture of 50:50 allograft: xenograft particulate bone was used to graft the deficient ridge. The bone graft was covered with a titanium reinforced barrier membrane (Cytoplast™ Ti-250) which was in turn covered by an amnion-chorion barrier membrane (BioXclude®). The membranes were secured with stabilizing sutures and a periosteal releasing incision was made for the buccal flap for tension-free primary closure with 4-0 PTFE sutures and 5-0 chromic gut sutures. Hemostasis was achieved and post operative instructions were reviewed with the patient. The patient was asked to continue taking the Amoxicillin (Amox) for a period of 7 days, additional Rx given for T3 (x25 tabs) 1-2 q4-6h prn pain and Decadron 4 mg once daily for 4 days (loading dose = 8 mg). The patient was seen for a 3-week postoperative visit and the surgical sites appeared to be healing well characterized by minimal inflammation and patency of the wound closure. During a 3month post operative follow up, a 2×2 mm membrane exposure was detected coronally, but the soft tissues were healthy and left to continue the natural course of healing.
Fig. 7

Fig. 8

Fig. 9
Retreatment: In July 2019, seven months after the combined apicoectomy/GBR procedure, the patient consented to a second implant procedure in the same site. Total LA was achieved with: 2×1.8 cc Lido, 2% 1:100K Epi for B/P infiltration. FTF B/P elevated; the titanium membrane was removed; an osteotomy was prepared for a BiohorizonsR Tapered Internal, Laser-Lok RBT 3.8×12 mm fixture (3.5 mm platform); and the fixture was placed with excellent primary stability. A cover screw was placed, saline irrigation was maintained throughout the procedure. (Fig. 10) The site was closed with 5-0 chromic gut int sutures. Rx given for Amox 500 tid/7days + T3(x25 tabs) 1-2 q4-6h prn pain. (Fig. 10) The patient was seen for a 2 week, followed by a 2.5 month follow up and both times healing was noted to be progressing well and was uneventful. Following a healing period of 4.5 months, stage 2 Surgery was performed using LA: 1.8 cc Lido 2% 1/100K Epi for B/P infiltration, to expose the implant.
Fig. 10

Prosthetic Procedures: were commenced one month later in February 2020, for fabrication of a screw retained one piece UCLA abutment/ PBM crown. Prosthetic procedures and materials used were similar to those described above. After a try in and confirmation of fit and shade, the crown was screwed in and torqued to 30 Ncm. (Fig. 11,12). Proximal contacts were assessed to be positive; occlusion was relieved in both centric and eccentric excursions. The access hole was permanently sealed with Teflon and composite resin once the patient had worn the crown for a few weeks and had adapted to it. A follow up was done in May 2021. (Fig. 13) Bone levels and the prosthesis were found stable. A CBCT was taken for an issue associated with the 26,27. And the report indicated that the implant in the 23 site to be within the range of normal., with circumferential osseous coverage along its surfaces. (Fig. 14)
Fig. 11

Fig. 12

Fig. 13

Fig. 14

Case#3
A 34-year-old male patient presented to our office in May 2010 with a fractured 22 with wanting options for replacement. He reported a previous history of orthodontic treatment. Medical history was significant for Down’s syndrome, Hepatitis C attributed to a previous blood transfusion and previous chemotherapy for leukemia. He reported allergies to penicillin, aspirin, aminoglycosides, benzodiazepines and Ibuprofen.
Pre -Treatment Assessment: Tooth 22 demonstrated a horizontal fracture and Grade 3 mobility. (Fig. 1) Prognosis was determined to be poor as the tooth was non restorable. In June 2010, the tooth was extracted under local anesthesia (2×1.8ccLlido 2%; 1: 100K Epi B/P infiltration), after reflecting a full thickness flap. (Fig. 2) The socket was curetted and grafted with MinerossTM particulate mineralized cortico-cancellous allograft (Biohorizons®) and closed with 4.0 plain gut sutures. Positive hemostasis was achieved. A prescription for Tylenol #2; 1-2 tabs q4-6 hours was given with instruction on care of the extraction site. The patient was seen two weeks postoperatively to assess healing. A transitional acrylic removable prosthesis was fabricated and inserted to restore esthetics and function. Treatment options were discussed, and the guardians consented on behalf of the patient to replace the 22 with an implant supported fixed prosthesis.
Fig. 1

Fig. 2
Implant Surgery: In December 2010, a surgical guide was fabricated for the proposed 22 implant. A full thickness flap was reflected with a para-crestal incision under local anesthesia (2×1.8cc Lido 2%; 1: 100K Epi B/P infiltration). The osteotomy was prepared for a 3.5x9m, 3.5 Platform Biohorizons Laser-Lok Implant. Excellent primary stability was achieved that resisted a 40Ncm torque. (Fig. 3) The site was irrigated and closed with 5.0 chromic gut sutures. A prescription for Clindamycin 300qidx 7days and Tylenol T2 1-2 tabs qid x7days was given along with a Peridex rinse bd. The patient was asked not to wear his transitional denture for 6 weeks. A week later, the patient presented for a post operative follow up. Oral hygiene instructions were given at this time.
Fig. 3

In January 2011, the patient presented with his guardian with the implant exfoliated. (Fig. 4)
Fig. 4

After a re-discussion of the options, the guardians consented to a second surgical placement of the implant in the 22 site. In March 2011, using two cartridges of the anesthesia described previously an osteotomy was prepared for a Straumann® BL 3.3mmNC, SLActiveR 12mm Ti fixture. Good primary stability was achieved. The implant was closed with a cover screw and submerged. (Fig. 5) The site was closed with 4.0 plain gut interrupted sutures. Hemostasis was achieved and a prescription for Clindamycin given as described above with instructions on care and hygiene. At the two week post operative appointment, the transitional denture was relined with CoESoftR and the reline was repeated every 6 weeks. The patient was seen for a second surgical follow up six weeks post operatively. The implant fixture was exposed in July 2019 by reflecting a full thickness flap buccally and palatally under LA 2×1.8cc Lido 2%; 1: 100K Epi B/P infiltration.
Fig. 5

Prosthetic Procedures: In September 2011, after tissue healing, prosthetic procedures were commenced for fabrication of a screw retained crown. (Fig 6) Final impressions using medium body FlexitimeR on a custom tray were made after affixing an open tray transfer coping to the implant. In October 2011, a porcelain bonded to metal (IDentalloyR) screw retained crown was tried in, inserted and torqued to 30Ncm. Interproximal contacts were assessed to be positive and there was no occlusion with the opposing dentition either in centric or eccentric excursions. (Figs. 7,8,9) The access hole was sealed with Teflon and composite. Follow up appointments were done every year to assess the prognosis of the 22 implant and prosthetic restoration. To date, the bone levels are maintained, the occlusion on the crown is negative, and the patient continues to see his family dentist for regular hygiene and recall appointments. (Figs.10)
Fig. 6

Fig. 7

Fig. 8

Fig. 9

Fig. 10

Discussion
Whether an implant survives or fails can be dependent on numerous individual surgical factors or in multifactorial association. These include, but are not limited to, quality and quantity of bone at the time of implant placement, insufficient thickness of buccal bone shelf (i.e., < 2mm), soft tissue thickness and width of keratinized gingiva, insertion torque values, heat generated during drilling and insufficient irrigation of bone during osteotomy preparation, operator experience, and health status of the patient (Zhou et al., 2016). Most of these factors can be controlled for but despite the attention to these factors’ failures can still occur. Some failures are clean in that the implant fails to integrate and is lost early during the healing process (known as “early” implant failures) whereas other failures are considered as “late” implant failures occurring typically after 5 years in function.
A site of previous failure is not a contra-indication for reimplantation however certain precautions must be taken in order to increase the prospects of implant integration, success, and survival. All failed sites require careful debridement of the site, typically using curettes, upon implant removal. Oftentimes, it is beneficial to allow the site to heal for 2-3 months before reattempting implant placement as a large number of failed sites will require additional hard and soft tissue augmentation prior to reimplantation. Sometimes, if there is a clean failure and no active infection, good quality of soft tissue and intact bone walls, immediate reimplantation can be considered. Lastly, hard and soft tissue augmentation at the time of the failed implant removal can also be considered with delayed implant placement at the appropriate time (~ 4-6 months). The rationale for this is to allow for more bone healing as it is presumed that sites of failure would be inherently compromised. In general however, with respect to timing, a longer healing and integration period is prudent.
We have presented 3 cases of successful reimplantation into previously failed sites with long-term follow-up. Although limited conclusions can be made from a small number of cases, we have shown that sites of previous failure can be successfully rehabilitated, and this is consistent with the literature. Of course, patient preparation is critical for understanding that with each failure, the subsequent success and survival rates may be slightly less given that the sites of failure are potentially more compromised than sites of initial success.
Oral Health welcomes this original article.
Acknowledgements
Case 1: Orthodontic treatment credited to Dr. Girish Deshpande at Mississauga Dental Specialists. Final Bone grafting and Implant surgery to Dr. Daniel Zeiter, Hamilton.
Case 2: Apicoectomy was performed by Dr. Pavel Cherkas at Mississauga Dental Specialists.
Laboratory work for all cases performed by Randy Kwon at Progenic Dental Lab- Oakville.
Informed consent was obtained from patients prior to publishing this manuscript.
References
- Ata-Ali J, Ata-Ali F, Ata-Ali F. Do antibiotics decrease implant failure and postoperative infections? A systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2014 Jan;43(1):68-74. doi: 10.1016/j.ijom.2013.05.019.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Periodontally compromised vs. periodontally healthy patients and dental implants: a systematic review and meta-analysis. J Dent. 2014 Dec;42(12):1509-27. doi: 10.1016/j.jdent.2014.09.013.
- Grossmann Y, Levin L. Success and survival of single dental implants placed in sites of previously failed implants. J Periodontol. 2007 Sep;78(9):1670-4. doi: 10.1902/jop.2007.060516.
- Jemt T (a). A retro-prospective effectiveness study on 3448 implant operations at one referral clinic: A multifactorial analysis. Part I: Clinical factors associated to early implant failures. Clin Implant Dent Relat Res. 2017 Dec;19(6):980-988. doi: 10.1111/cid.12539.
- Jemt T (b). A retro-prospective effectiveness study on 3448 implant operations at one referral clinic: A multifactorial analysis. Part II: Clinical factors associated to peri-implantitis surgery and late implant failures. Clin Implant Dent Relat Res. 2017 Dec;19(6):972-979. doi: 10.1111/cid.12538.
- Machtei EE, Mahler D, Oettinger-Barak O, Zuabi O, Horwitz J. Dental implants placed in previously failed sites: survival rate and factors affecting the outcome. Clin Oral Implants Res. 2008 Mar;19(3):259-64. doi: 10.1111/j.1600-0501.2007.01466.x.
- Machtei EE, Horwitz J, Mahler D, Grossmann Y, Levin L. Third attempt to place implants in sites where previous surgeries have failed. J Clin Periodontol. 2011 Feb;38(2):195-8. doi: 10.1111/j.1600-051X.2010.01629.x.
- Manzano G, Montero J, Martín-Vallejo J, Del Fabbro M, Bravo M, Testori T. Risk Factors in Early Implant Failure: A Meta-Analysis. Implant Dent. 2016 Apr;25(2):272-80. doi: 10.1097/ID.0000000000000386.
- Mardinger O, Ben Zvi Y, Chaushu G, Nissan J, Manor Y. A retrospective analysis of replacing dental implants in previously failed sites. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012 Sep;114(3):290-3. doi: 10.1016/j.tripleo.2011.07.010.
- Moraschini V, Poubel LA, Ferreira VF, Barboza Edos S. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg. 2015 Mar;44(3):377-88. doi: 10.1016/j.ijom.2014.10.023.
- Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A. Periodontitis, implant loss and peri-implantitis. A meta-analysis. Clin Oral Implants Res. 2015 Apr;26(4):e8-e16. doi: 10.1111/clr.12319.
- Zhao D, Wu Y, Xu C, Zhang F. Immediate dental implant placement into infected vs. non-infected sockets: a meta-analysis. Clin Oral Implants Res. 2016 Oct;27(10):1290-1296. doi: 10.1111/clr.12739.
- Zhou Y, Gao J, Luo L, Wang Y. Does Bruxism Contribute to Dental Implant Failure? A Systematic Review and Meta-Analysis. Clin Implant Dent Relat Res. 2016 Apr;18(2):410-20. doi: 10.1111/cid.12300.
- Zhou W, Wang F, Monje A, Elnayef B, Huang W, Wu Y. Feasibility of Dental Implant Replacement in Failed Sites:
A Systematic Review. Int J Oral Maxillofac Implants. 2016 May-Jun; 31(3):535-45. doi: 10.11607/jomi.4312.
About the Author
 Dr. Vinay Bhide is a periodontist with special interest in esthetic and reconstructive periodontics. In addition to private practice, Dr. Bhide teaches both undergraduate and graduate levels at the University of Toronto, and is also an Adjunct Assistant Professor in the Department of Periodontics at UPenn. He lectures nationally and internationally on periodontics and surgical implantology.
Dr. Vinay Bhide is a periodontist with special interest in esthetic and reconstructive periodontics. In addition to private practice, Dr. Bhide teaches both undergraduate and graduate levels at the University of Toronto, and is also an Adjunct Assistant Professor in the Department of Periodontics at UPenn. He lectures nationally and internationally on periodontics and surgical implantology.
 Dr. Neena D’Souza is an Adjunct Professor at the Faculty of Dentistry, University of Toronto. She is involved in several clinical research projects and teaches in the graduate and undergraduate programs . Dr. D’Souza is a prosthodontist who provides a full range of prosthodontic services at Mississauga Dental Specialists, an interdisciplinary specialty practice in Mississauga Ont. Direct correspondence to Dr. D’Souza at drndsouza@dentalspecialist.ca.
Dr. Neena D’Souza is an Adjunct Professor at the Faculty of Dentistry, University of Toronto. She is involved in several clinical research projects and teaches in the graduate and undergraduate programs . Dr. D’Souza is a prosthodontist who provides a full range of prosthodontic services at Mississauga Dental Specialists, an interdisciplinary specialty practice in Mississauga Ont. Direct correspondence to Dr. D’Souza at drndsouza@dentalspecialist.ca.












