Surgical Background and Treatment
The patient is a 31 year old healthy gentlemen who presented to the oral surgery office with a 3 month history of a left mandibular swelling. He was evaluated by his dentist and the thought at that time was a dental infection originating from tooth #36. Subsequently, he saw an endodontist and received endodontic treatment on tooth #36. Unfortunately, the swelling failed to subside, and he was referred to me for further evaluation.
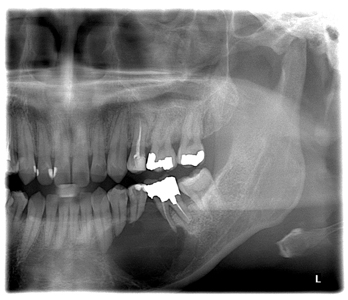
His initial examination revealed a firm swelling with buccal expansion in the mandible from #33 to 36. His panorex showed a large multilocular, radiolucent lesion in the left mandible, with root resorption of #33, 34, 35, 36. (Fig 1) The differential diagnoses at that time included inflammatory processes like dental infection or residual cyst, but more likely an odontogenic cyst or tumor versus other mesenchymal neoplasms (ex central giant cell granuloma, sarcoma etc).
Fig. 1
A biopsy was performed and the result came back as conventional type ameloblastoma. Ameloablastoma is a benign tumor of odontogenic epithelial origin. It is a slow-growing, locally invasive tumor that can occur in three different clinico-radiographic forms: convention solid/multicystic, unicystic, or peripheral. Of these, the conventional type is the most common, at about 86 percent of all cases.1 Ameloblastoma is usually asymptomatic until it has reached a size to produce swelling, tooth and dental occlusion disturbances, or it is revealed incidentally on radiographs.2 The standard treatment for a conventional type of ameloblastoma is mandibular resection with 1 -1.5 cm margin.3 In this current case, given the extend of the tumor, the resection would include the inferior border resulting in a discontinuity defect. (Fig 2,3) The reconstructive options for such a defect include free vascularized tissue transfer (fibular or scapular flaps) versus a non-vascularized bone graft. There are advantages and disadvantages to these options which are beyond the scope of this article. For a 5-6 cm discontinuity defect in the mandibular body, a high success rate can be achieved using iliac crest bone graft.4,5 After throughout discussion with the patient, he opted for this option. As such, he was reconstructed using both posterior and anterior iliac crest bone graft in a staged manner. (Figs. 4,5)
Fig. 2

Fig. 3

Fig. 4

Fig. 5

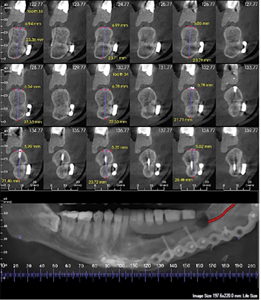
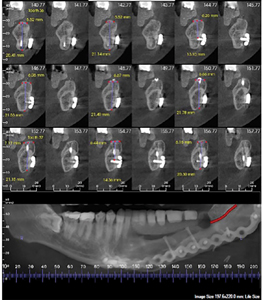
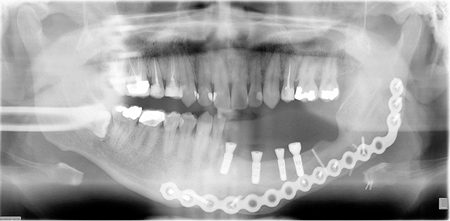
After about 6 months of healing of the iliac crest bone graft, the patient was referred to a prosthodontist for the appropriate pre-surgical planning. Four dental implants were placed using CT guidance. (Fig. 6)
Fig. 6
Prosthetic Consideration:
Following the surgical resection of the ameloblastoma lesion and the subsequent reconstruction to restore mandibular continuity, the patient is ready for prosthetic rehabilitation. In planning for the prosthetic treatment, the goals in this case are to restore form, function and aesthetics. However, due to the nature of the surgical procedures, patient with an acquired mandibular defects will exhibit some common clinical features.
Clinical Consideration:
The patient may:
- be missing multiple anterior and posterior teeth on the affected side
- have a large compromised denture bearing surface
- have both a large hard and soft tissue defect
- lack proper sensory and motor control to detect and manipulate food bolus on the resected side
- have a tendency of the mandible to deviate during mandibular movement if continuity is not achieved.
Prosthetic Options and Considerations:
In this clinical case, similar to other partial edentulous cases, the treatment options are very similar.
They include
- Removable Partial Denture
- Implant Supported Overdenture
- Implant Supported Fixed Partial Denture
However, unique to a case with an acquired mandibular defect, there are additional considerations when it comes to treatment planning for a prosthetic rehabilitation.
Fig. 7
Fig. 8
Fig. 9
Fig. 10
Fig. 11
For a removable partial denture, unique to a case with an acquired mandibular defect, the edentulous span is unusually long and unilateral. The remaining adjacent teeth are often not suitable abutments to provide the ideal retention, stability and support for a removable partial denture. Some important considerations are the possible location of fulcrum lines, the strategic use of RPD components for bracing effect as well as minimizing the possible undue stress on the available abutments during functional movements.
For an implant supported removable solution, the use of implants can improve significantly in patients with an acquired mandibular defect. However, before one can consider the use of dental implants, one must consider the size of the available bone. The available bone may be in the form residual bone or grafted bone. In any case, it is ideal to have at least 10mm of vertical bone before implants can be considered. The success rates of implants placed in residual bone as well as grafted bone have been great. One of the many advantages of using dental implant includes the improved support mechanism as compared to the conventional removable partial denture. Also, specific to a removable solution, the use of a denture flange can help restore the much needed soft and hard tissue defect. Lastly, the removable nature of this solution also facilitates hygiene practice around the implants as well as the intaglio surface of the prosthesis.
In considering the position of implants for a removable solution, due to the often pre-existing vertical defect, there is usually an abundance of prosthetic space vertically for the prosthesis. However, the common challenge is to ensure the placements of implants can be made within the contours of the anticipated prosthesis in the buccal and lingual direction and the mesial distal direction. The reality of these resected cases is that the available residual and/or grafted bone may deviate from the ideal location of the prosthetic teeth. Practitioners must evaluate carefully to ensure that the placement of implants can be placed within the confines of the anticipated prosthesis as much as possible. Ideally the implants should be perpendicular to the occlusal plane and within the zone of the residual attached gingiva. The retentive mechanism can be both in the form of individual stud supported abutments and/or part of a splinted bar. Similar to conventional implant prosthodontics, the decision depends on the location and the distributions of implants and the anticipated of forces during loading. Unique to a resected case in the mandible, the forces of loading may deviate from conventional cases where the patient may tend to move towards the unresected side and that the location of the prosthetic teeth may be arranged differently to minimize tipping forces. Therefore, there are many elements at play to provide a favourable outcome.
Unfortunately, some patients, such as in this case, cannot accept a removable implant solution despite the many advantages. As a result, a fixed implant solution has been selected for this patient.
Fig. 12A
Fig. 12B
Fig. 13
Fig. 14
Initial Examination and Treatment Planning
To begin treatment, an initial examination was carried out to determine the state of the defect that needs to be restored. The patient was presented with a partial edentulous area with the following missing teeth 38 37 36 35 35 34 33 32 31 and 41. Also noted are the soft and hard tissue defect with a small zone of attached gingiva.
The preliminary stages of the treatment have been reviewed. They include the following:
- Prosthetic work up with radiographic template and a CBCT
- Surgical Stage by the oral surgeon for implant placement
- Prosthetic Stage for the fabrication of definitive prosthesis.
At this stage, I have reviewed the two most sensible treatment solutions and their advantages and disadvantages:
- Fixed Implant Supported Prosthesis
- Removable Implant Supported Prosthesis with stud or bar attachments.
During the prosthetic work up appointments, additional radiographs and pictures were taken. Preliminary impressions with stock trays in polyvinyl siloxane putty and light body material were used. The odontogram and the periodontal charting were also completed.
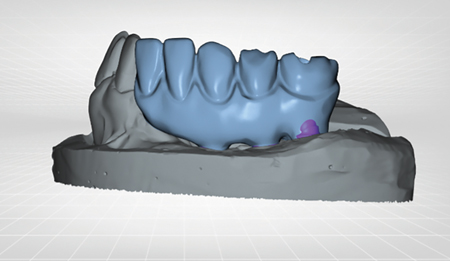
It was decided to fabricate a radiographic template to evaluate the available bone in comparison to the planned prosthetic teeth. A custom tray was fabricated from the study model and a final impression was made using polyether impression material.
In an effort to complement the opposing arch contour and the existing adjacent teeth, the initial set up involved three anterior teeth, a premolar and two molars. The resulting teeth arrangement will lead to a mis-match of dental midlines and the subsequent replacement of three anterior teeth even though the patient was missing four anterior teeth. This prosthetic arrangement has been communicated with the patient well in advance and the patient has approved for the teeth arrangement. It was also communicated that the second molar may or may not be replaced depending on the available bone for implants.
In this particular case, it was decided to use radiopaque denture teeth in the set up to help with acquiring the CBCT images for more analysis. The set up was tried in the mouth to verify the aesthetics and the occlusion and then later processed in pink acrylic. Using this radiographic template, a CBCT was obtained to evaluate the available bone.
The attached CBCT revealed a very common finding in a case with an acquired mandibular defect. The available bone is often buccal to the desired prosthetic teeth arrangement. However, it is ideal to place implants directly over the prosthetic teeth for ideal force distribution. Unfortunately, the clinical challenge with reconstructed cases is that the available bone often lies buccal to where the prosthetic teeth are. As you review the CBCT scan, you will see that the problem is more significant along the posterior area.
Radiographic Stent Fabrication
Fig. 15
Fig. 16
Fig. 17
Fig. 18
Fig. 19
Conversion of radiographic stent to surgical stent
Fig. 20
Fig. 21
Based on the CBCT analysis, the surgical plan is to convert the radiographic template to a surgical template for the implant placement procedure. Four mandibular implants have been planned strategically to provide support for the implant prosthesis.
During the surgical placement of implants, it was noted there was a broken fixture screw. In any case, the implants were positioned as closely as possible within the confines of the planned prosthetic teeth. Four Straumann Bone Level Implants have been placed successfully.
Post surgical healing and evaluation
Fig. 22
Fig. 23
Fig. 24
Final impression
Fig. 25
Fig. 26
Following the surgical treatment of implant placement, the patient is now ready for the fabrication of the definitive prosthesis. In planning out this prosthetic phase, there were additional considerations. The prosthetic treatment plan included both a provisional implant supported restoration and a permanent restoration.
There were many treatment goals for the provisional implant supported restoration. The provisional restoration will allow for a more accurate diagnostic evaluation of how the patient will tolerate the aesthetic set up, the functional arrangement as well as how home care can be carried out with a fixed solution. In addition, given the relatively young age of the patient, it is expected that the definitive restoration will be subjected to the normal wear and tear and at some point, may require some form of prosthetic repair, partial refurbishment or a complete replacement. After testing out the provisional restoration as a diagnostic tool, this provisional implant supported restoration can also provide the patient a peace of mind and serves as a back up prosthesis should the permanent restoration require any future removal for routine maintenance need.
Verification jig/Pick up impression
Since the prosthesis will require splinting multiple implants over a relatively long edentulous span, the accuracy of the implant positions and angulations should be verified. Non engaging temporary cylinders along with light cured resin based material (Triad® VLC)were used to fabricate verification jigs. They were subsequently tried in intra-orally and luted together using low shrinkage autopolymerisation polymethylmethacrylate. (GC pattern resin). Once the resin has completely cured, a new pick up impression was made with polyether impression material in a custom tray. The impression was pour subsequently to fabricate the master model. Figs. 27, 28
Fig. 27A
Fig. 27B
Fig. 28
Once the model has been fabricated, the next step is obtain a jaw relation record. Using two temporary non engaging cylinders, an implant supported occlusion rim was fabricated. Rather than the conventional soft tissue supported occlusion rim, this occlusion rim will be implant supported and will provide more stability and accuracy in obtaining the jaw relation record. Once the occlusion rim has been adjusted and notched, a polyvinyl siloxane registration material (Futar) was used to record this jaw relationship. A shade was also selected at this appointment as well.
Jaw relation record
Fig. 29
Fig. 30
Fig. 31
Teeth Try in
Fig. 32
Fig. 33
Fig. 34
Fig. 35
Following obtaining the jaw relation record, the case was mounted on a semi-adjustable articulator. Prosthetic teeth arrangement was completed for evaluation and tried in. During the teeth try in phase, the occlusal relation and the aesthetic arrangement were evaluated and approved by the patient. Fig. 36
Fig. 36
Fabrication of Provisional Implant Supported Restoration
Figs. 37, 38, 39
Fig. 37
Fig. 38
Fig. 39
Once the teeth arrangement has been approved, the case was sent back to the lab for processing. This resulting provisional implant supported restoration was made with four temporary cylinders and laboratory processed acrylic. During the insertion appointment, the occlusion and aesthetics were again reviewed and approved by the patient and finally inserted. Prior to delivering this prosthesis, an index was fabricated to record the relationship of the prosthetic teeth on the model. The master model with the prosthesis was also scanned to obtain a digital record of the case. Once the provisional prosthesis was delivered, an important element was to evaluate how hygiene can be carried out and whether the soft and hard tissue defect is of concern to the patient. Knowing the limitation of a fixed implant supported prosthesis, the patient was instructed to function for six months before the definitive prosthesis can be planned and finalized.
Evaluation At Six Month
During the six month evaluation, the patient tolerated the prosthesis well. There was no fracture or any issue with the function of the prosthesis. The lack of facial or lip support without the flange was not an issue to the patient. However, the intaglio surface was difficult to clean and the patient reported one episode of soft tissue inflammation around the implants. Based on the patient’s experience, the decision was to move forward in fabricating a definitive fixed prosthesis with one modification. The modification involved the provision of a larger space between the soft tissue and the intaglio surface of the definitive prosthesis to facilitate home care.
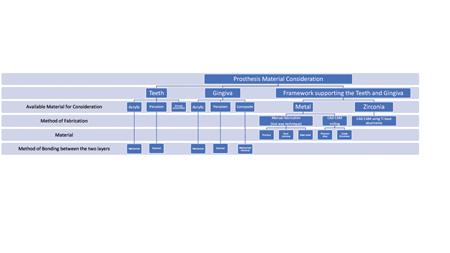
In moving forward to fabricate the definitive prosthesis, a decision has to be made regarding the choice of material. This was explored and discussed in detail with the patient during the provisional phase. At this time, the options are reviewed once again. The options are:
- Acrylic based with a metal frame
- Metal ceramic restoration
- Monolithic zirconia restoration
- Facially veneered zirconia restoration
Every material carries a different set of advantages and disadvantages. Along with the material comes with the decision making process regarding the available manufacturing methods that also come with their advantages and shortcomings. Unique to this case, unlike single unit dentistry, this is a relative long span restoration both in the mesial distal direction as well as the occlusal gingival direction. Fortunately, the span has been well supported by four well placed dental implants with very little area for unsupported restoration.
In considering the different materials and manufacturing methods available, a flow chart has been prepared to help summarize the available options. Along with the different materials available, the consideration should also be based on their reparability of the material, the aesthetic outcome of the case, their wear resistance and mechanical and optical properties. All of these may impact on the patient’s decision on which material to use for the definitive prosthesis. Figs. 40, 41
Fig. 40
Fig. 41
In reviewing the different materials with their advantages and disadvantages, the patient had selected acrylic with a metal frame to be the material for the definitive prosthesis. Once this decision has been made, the fabrication has been quite straight forward as we still have the a verified model from before, an index of the provisional implant bridge as well as the digital scan of the case with and without the provisional prosthesis which has been tried and tested in the mouth for comfort, aesthetic and function. The only modification is to design a framework that will raise the intaglio surface occlusally to allow a space for home care.
The patient has been sent the digital view of the proposed framework and approved with such design. The framework was subsequently milled in titanium using CAD/CAM technology.
Fabrication of metal framework (milled bar)
Fig. 42
Fig. 43
Fig. 44
Try in milled titanium bar
Fig. 45

Fig. 46
Fig. 47
Fig. 48
Fig. 49
Fig. 50
The titanium metal framework was tried in to ensure a passive fit. Radiographs were taken to confirm the positive seat of the framework to all the implants.
Try in of titanium milled bar with teeth
Fig. 51

Fig. 52
Fig. 53
Fig. 54
The next step is to transfer the teeth set up to the metal framework and to confirm the jaw relation and the aesthetic tooth arrangement with the patient.
Delivery of Implant Supported Fixed Prosthesis
Fig. 55

Fig. 56
Fig. 57
Fig. 58
Fig. 59
Fig. 60
Once the set up has been confirmed, the final processing of the acrylic will be completed on the framework and prepared for the final delivery.
Post delivery
Once the prosthesis has been delivered, the patient has been seen two weeks to evaluate the comfort, function and home care. The patient has been able to demonstrate proper home care and reported to have no discomfort with the prosthesis. The provisional prosthesis was returned to the patient in case maintenance or repair is needed on the definitive prosthesis.
Challenges Encountered During Treatment
In treating these cases with an acquired mandibular defect, due to the pre-existing vertical defect, the available typical drivers were often too short to engage the prosthetic screws through the long clinical crowns. An extra long driver had to be ordered to facilitate treatment during the appointments. At times, the soft tissue interference, the difficulty in negotiating the screws through the long clinical crowns may cause discomfort during the try in appointments. At times, the administration of local anesthesia may be necessary to improve the comfort for the patient.
Summary of Prosthetic Treatment
This article documents the thought process, the treatment consideration as well as the actual treatment provided for a patient who had undergone mandibular reconstruction from a benign but locally aggressive ameloblastoma lesion. The prosthetic treatment provided here is a fixed implant supported solution restoring the patient’s function and aesthetics.
Oral Health welcomes this original article.
LHM Dental Studios is a full-service Toronto dental lab that has been serving the Canadian dental industry for 64 years. Slawek Bilko is the president of LHM
Slawek Bilko, RDT, President
LHM Dental Studios Ltd., 1407 Dufferin St. Toronto, ON M6H 4C7. (416) 924-6684 x 206 Toll Free: (800) 387-0092. slawek@lhmdentallab.com
Steve Somerville is the General Manager of DSG Novo, a lab specializing in cutting-edge, digitally-focused practices. DSG Novo has built its industry reputation by pairing digital implant services with a personalized touch. When he’s not spending time in the lab or connecting with customers, Steve enjoys time at the cottage and travelling.
Novo Dental Studio DSG
905-2300 Yonge Street, Toronto, ON M4P 1E4
Phone: (647) 352-6866. Toll-Free Phone: 1-877-374-5227. Fax: (905) 342-2803
ssomerville@dentalservices.net
Panthera Dental
Andreas Klie, RDT, Sales Director – Ontario and Western Canada
C: 1.905.220.6122
9105 rue John-Simons, Quebec, QC
Canada, G2B 0S6
Phone: + 1 (418) 527-0388
Toll Free: + 1 (855) 233-0388
Email: info@pantheradental.com
About Panthera Prosthetic
The Prosthetic division offers the widest variety of CAD/CAM dental prosthetic products on the global market and is renowned for its unprecedented product quality and its ability to offer the most comprehensive compatibility of implant connections and platforms. All Panthera Prosthetic products are 5 µm precision manufactured using high speed 5 axis milling or CNC turning manufacturing and a wide variety of medical materials.
References
- Budtz-Jörgensen E. Restoration of the partially edentulous mouth—a comparison of overdentures, removable partial dentures, fixed partial dentures and implant treatment.
J Dent. 1996 Jul;24(4):237-44. doi: 10.1016/ 0300-5712(95)00075-5. PMID: 8783527. - Conrad HJ, Seong WJ, Pesun IJ. Current ceramic materials and systems with clinical recommendations: a systematic review. J Prosthet Dent. 2007 Nov;98(5):389-404. doi: 10.1016/S0022-3913(07)60124-3. PMID: 18021828.
- Fonseca et al, Oral and Maxillofacial Surgery 2nd edition. Elsevier 2009
- Guess PC, Att W, Strub JR. Zirconia in fixed implant prosthodontics. Clin Implant Dent Relat Res. 2012 Oct;14(5):633-45. doi: 10.1111/j.1708-8208.2010.00317.x. Epub 2010 Dec 22. PMID: 21176095.
- Janyavula S, Lawson N, Cakir D, Beck P, Ramp LC, Burgess JO. The wear of polished and glazed zirconia against enamel. J Prosthet Dent. 2013 Jan;109(1):22-9. doi: 10.1016/S0022-3913(13)60005-0. Erratum in: J Prosthet Dent. 2015 Jul;114(1):159. Lawson, Nathaniel [corrected to Lawson, Nathaniel C]. PMID: 23328193.
- Keller EE, Desjardins RP, Eckert SE, Tolman DE. Composite bone grafts and titanium implants in mandibular discontinuity reconstruction. Int J Oral Maxillofac Implants. 1988 Winter;3(4):261-7. PMID: 3075966.
- Ludovichetti FS, Trindade FZ, Werner A, Kleverlaan CJ, Fonseca RG. Wear resistance and abrasiveness of CAD-CAM monolithic materials. J Prosthet Dent. 2018 Aug;120(2):318.e1-318.e8. doi: 10.1016/j.prosdent.2018.05.011. PMID: 30097264.
- Mendenhall WM, Werning JW, Fernandes R, Malyapa RS, Mendenhall NP. Ameloblastoma. Am J Clin Oncol. 2007 Dec;30(6):645-8. doi: 10.1097/COC.0b013e3181573e59. PMID: 18091060.
- Moreno-Soriano C, Estrugo-Devesa A, Castañeda-Vega P, Jané-Salas E, López-López J. Postsurgical Prosthetic Rehabilitation after
- Mandibular Ameloblastoma Resection: A 7-Year Follow-Up Case Report. Case Rep Dent. 2021 Mar 28;2021:5593973. doi: 10.1155/2021/5593973. PMID: 33854802; PMCID: PMC8021463.
- Moura LB, Carvalho PHA, Xavier CB, Post LK, Torriani MA, Santagata M, Chagas Júnior OL. Autogenous non-vascularized bone graft in segmental mandibular reconstruction: a systematic review. Int J Oral Maxillofac Surg. 2016 Nov;45(11):1388-1394.
- Neville et al, Oral and Maxillofacial Pathology 1st edition. W.B. Saunders 1995
- Okoturo E. Non-vascularised iliac crest bone graft for immediate reconstruction of lateral mandibular defect. Oral Maxillofac Surg. 2016 Dec;20(4):425-429.
- Pjetursson BE, Valente NA, Strasding M, Zwahlen M, Liu S, Sailer I. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic single crowns. Clin Oral Implants Res. 2018 Oct;29 Suppl 16:199-214. doi: 10.1111/clr.13306. PMID: 30328190.
- Zarone F, Russo S, Sorrentino R. From porcelain-fused-to-metal to zirconia: clinical and experimental considerations. Dent Mater. 2011 Jan;27(1):83-96. doi: 10.1016/j.dental.2010.10.024. Epub 2010 Nov 21. PMID: 21094996.
About the Author
 Dr. Leung received her DDS degree at the University of Toronto. She then completed a General Practice Residency at the Boston Medical Center and a Prosthodontics Residency Program at the University of Pittsburgh. Dr. Leung is a prosthodontist in midtown Toronto and York region. She has a long history with prosthodontic education at the University of Toronto and recently joined the Faculty as an Assistant Professor.
Dr. Leung received her DDS degree at the University of Toronto. She then completed a General Practice Residency at the Boston Medical Center and a Prosthodontics Residency Program at the University of Pittsburgh. Dr. Leung is a prosthodontist in midtown Toronto and York region. She has a long history with prosthodontic education at the University of Toronto and recently joined the Faculty as an Assistant Professor.
 Dr. Lee is an oral and maxillofacial surgeon with Crescent Oral Surgery in the Greater Toronto Area. He is a staff surgeon at Mount Sinai Hospital and Centenary Hospital (Scarborough health network). Kris received his dental degree in Toronto, and received his medical degree and oral and maxillofacial surgery certificate from the university of Michigan.
Dr. Lee is an oral and maxillofacial surgeon with Crescent Oral Surgery in the Greater Toronto Area. He is a staff surgeon at Mount Sinai Hospital and Centenary Hospital (Scarborough health network). Kris received his dental degree in Toronto, and received his medical degree and oral and maxillofacial surgery certificate from the university of Michigan.