Introduction
A removable overdenture prosthesis is a practical rehabilitative alternative to a conventional complete denture as it is more comfortable, retentive, and satisfying for patients. It is a cost-effective alternative to a fixed implant-supported complete denture.1 Advancements in diagnostic, surgical and prosthetic technologies, combined with clinical research comparing different treatment outcomes, have resulted in an improvement in implant overdenture therapy. In providing overdentures for patients the implant surgeon and the restorative dentist must have a thorough understanding of each patient’s unique restorative needs and expectations, as well as esthetic and functional demands.2 It is particularly important to select a prosthesis that satisfies the patient, as a lack of satisfaction may lead them to abandon the prosthesis and look for other treatments.1
We sometimes see our own cases requiring revision or re-treatment 10 or more years later, even though treatment was carefully planned and executed with existing philosophies and technologies at the time. Furthermore, our patients age with us, and we should expect that a proportion will display an increase in well-defined risk factors for implant treatment failure, such as un-controlled diabetes or the inability to perform optimal home plaque control. This case report describes a removable implant prosthetic rehabilitation of both failing fixed implant bridgework as well as remaining dentition.
Surgical Considerations: Surgical-Restorative Collaboration
Correct implant positioning is critical if the end goal is to achieve an esthetically and functionally acceptable restoration that can be maintained through proper oral hygiene. Implant placement, although restoratively dictated, must also respect the various anatomic constraints that are often present in the vicinity. The most important advantage of guided surgery is that it allows all dental care providers to be involved and provide input from the beginning, ensuring a comprehensive diagnosis and treatment plan, as well as an improved outcome for the patient.2
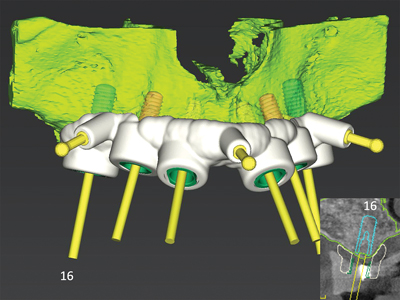
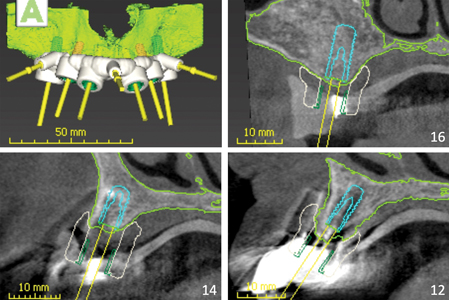
In figure 1, CoDiagnostiX© software (Dental Wings GmbH,) was used to merge an intraoral scan and cone beam CT (CBCT) image and create a virtual diagnostic wax-up of a future implant-supported bar overdenture. This diagnostic tool allows active collaboration of the implant surgeon, restorative dentist and registered dental technician. First, an ideal setup of prosthetic tooth position can be simulated, followed by a backwards workflow to simulate a favourable bar position and finally implant position within the existing alveolar ridge. This diagnostic tool can help to facilitate the planning of a structurally stable prosthesis , as it allows for the anticipation of sufficient space for both the acrylic and metal framework, thus potentially avoiding denture repairs later on.
Fig. 1

This technology allows the implant surgeon to visualize both the restorative and anatomic restrictions of each implant site, and work backward to select alveolar bone sites of adequate quality and quantity (Fig. 2).2
Fig. 2
Surgical Considerations: 1. Maximizing Irrigation Efficiency with Surgical Guides
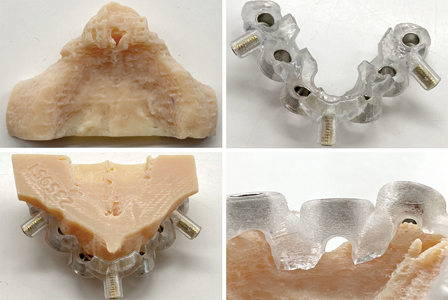
Adequate drill cooling is essential to prevent overheating of the bone, which could lead to thermal osteonecrosis. Figure 3 shows an example of a computer-aided design and computer-aided manufacturing (CAD-CAM) implant surgery guide and hard tissue model, in which guiding tubes are positioned at a distance from the bone. Longer drills are required to negotiate both these tubes and the set distance before entering the osteotomy site. Because of the increased drill length, the possible friction between the drill and guiding tube, and the physical barrier represented by the guide itself, irrigation efficiency has the potential to be significantly decreased.2 This can lead to an increase of frictional heat. To reduce this risk, buccal-lingual slots were created in the guide to provide access and help ensure adequate cooling during the osteotomy preparation. Frequent withdrawal and reinsertion of the drill, the use of drills with internal cooling, as well as copious and continuous irrigation with cold saline solution should all be considered to help improve irrigation efficiency.2
Fig. 3
Surgical Considerations: 2. Bone Quality and Volume
The reduced bone quality of the edentulous maxilla presents the primary challenge when compared to the edentulous mandible. The secondary challenge is reduced bone volume.3 The maxillary edentulous ridge resorbs both palatally and superiorly.4 Furthermore, this resorption process results in an increased proximity of the residual ridge relative to the maxillary sinus (Fig. 4).5
Fig. 4

A systematic review of long-term implant survival in the grafted maxillary sinus using the lateral window approach involving 18 studies, 2,149 patients and 6,500 implants found a 3-year post-loading implant survival rate of 93.7%.6 The use of textured implant surfaces, xenograft, and the placement of a barrier membrane over the window have all been found to increase implant survival rates in conjunction with sinus grafting (Fig. 5).5 Staged grafting of the maxillary sinus to permit implant placement carries with it the challenges of an increased number of surgeries for the patient, increased rehabilitative cost, and an overall increased treatment duration. Furthermore, the use of a removable interim prosthesis following bone grafting, to replace both function and esthetics, increases the risk of movement and compression of gingival tissues leading to wound dehiscence and possible complications with graft healing.7
Fig. 5

Surgical Considerations: 3. Engaging Available Bone
Alternatives to sinus grafting include the use of shorter implants in the posterior maxilla, the use of tilted implants to maximize their cross-arch antero-posterior distribution, or the use of extra-alveolar implants, including pterygoid and zygomatic implants. Systematic reviews of both zygomatic and pterygoid implants have revealed 12- and 10-year survival rates of 95.21% and 94.85% respectively.8-9 Complications associated with zygomatic implants are reportedly higher than for conventional implants,3 however, and the most common complication is sinusitis, which may develop several years after their placement. In these cases, it is rather difficult to remove zygomatic implants.10 Furthermore, challenges and complications may accompany the restoration of zygomatic implants, including unhygienic contours and phonetic challenges with palatal positioning of the implants.3
Surgical Considerations: 4. Peri-Implant Keratinized Mucosa
The presence of an adequate width of keratinized attached mucosa around dental implants may improve both soft and hard tissue stability, reduce plaque accumulation, help to prevent soft tissue recession and lower the incidence of peri-implant mucositis (Fig. 6).11 A systematic review of 15 studies and meta-analysis of 8 studies, including 1,031 patients and 3,408 implants, which assessed the association between peri-implant keratinization, with adequate defined as ≥2mm, and peri-implant health and stability, measured as tissue inflammation, plaque accumulation, bleeding and probing depth, found a statistically significant association between adequate keratinized tissue (KT) level and a lower Gingival Index / modified Gingival Index (mGI/GI), with a standard mean difference of -1.25 (P=0.01). KT was significantly associated with less peri-implant inflammation, evaluated qualitatively with mGI/GI.12 An apically positioned partial thickness flap in combination with a free gingival graft remains the gold standard in achieving predictable keratinization and soft tissue volume.11
Fig. 6

Prosthetic Considerations: 1. Number of Implants
A systematic review and meta-analysis of post-loading implant loss for removable and fixed implant-supported prostheses in edentulous jaws involving 54 studies, 2368 patients and 9267 implants found that implant loss rates for maxillary overdentures on less than 4 implants were significantly higher than for four implants, 7.22 versus 2.31 (P<0.0001).13 It has been recommended to use four to six implants and maximize their anteroposterior distribution to increase long-term treatment success with maxillary implant overdentures.14
Prosthetic Considerations: 2. Implant Trajectory
For a porcelain-fused-to-metal, porcelain-fused-to-zirconia, and monolithic zirconia screw-retained fixed prosthese s, the trajectory of the implants should be within the confines of the prosthetic tooth, as these prosthetic materials have excellent fracture resistance with thinner dimensions (Fig. 7A). For a screw-retained hybrid prosthesis or an implant-supported bar overdenture the implant trajectory should instead be within the prosthetic base and not tooth position. The screw access channel should exit lingual or palatal to the prosthetic teeth. Lingual positioning of the implants increases the restorative space for both the prosthetic framework as well as teeth. This, in turn, helps to prevent prosthetic tooth fracturing or debonding from the prosthetic base (Fig. 7B).15
Fig. 7A,B

Implant trajectories should be as parallel as possible when planning unsplinted implant-retained overdentures. This facilitates maintenance of the prosthesis as non-parallel implant axes compromise the insertion path which can lead to rapid wear of matrices, resulting in frequent replacement.16 The mandibular alveolar ridge almost always permits the placement of parallel implants, resulting in an overdenture that can be inserted vertically and with a parallel insertion path (Fig. 8). The maxillary alveolar ridge in contrast often has a small base, and implants are more likely to be placed with axial divergences. Although the LOCATOR® Implant Attachment System and Straumann® Novaloc® Retentive System can compensate for up to 40° and 60° of axial divergences respectively, retention seems to be decreased when these divergences are present.17
Fig. 8

Prosthetic Considerations: 3. Implant-Supported Bar Overdenture versus Unsplinted Implant-Retained Overdenture
A systematic review of 16 randomized clinical trials that compared overdentures supported by either bar and clip or ball and O-ring attachments for retention, masticatory efficiency, bone loss, and patient satisfaction found that the attachment type did not affect implant marginal bone loss, patients’ perceived masticatory quality, or their degree of satisfaction. Overdentures with the bar and clip attachment tended to have higher initial retention.1 Treatment with a bar overdenture has been found to involve a higher initial cost, but lower maintenance cost. On the other hand, replacement of missing or worn nylon inserts, such as with the LOCATOR® system, in an unsplinted implant-retained overdenture can often be done chairside.18
Bar overdentures are advantageous in providing support when there is excessive space between the maxillary and mandibular arches. They are also effective in providing support to manage the horizontal prosthetic cantilever which forms with advanced residual ridge resorption of the maxilla palatally and the mandible facially. (Fig. 1) Furthermore, bar overdentures help to facilitate in achieving ideal parallelism of retentive elements regardless of implant angulation.15 The minimum interocclusal space requirement from the platform of the implant to the opposing occlusion for an unsplinted implant-retained overdenture using the LOCATOR® system is 8.5mm, whereas an implant-supported bar overdenture requires 13-14mm of space.16
Prosthetic Considerations: 4. Cleans-ability and Patient Compliance
Careful bar design with proper clearance from the gingiva, that allows accessibility for plaque control and cleaning of peri-implant tissues, will help to reduce the susceptibility to peri-implantitis to that of an unsplinted implant-retained overdenture.19 A rigid parallel-wall CAD-CAM milled bar, designed to leave 1mm of clearance to enhance hygiene, will help to reduce rotational overdenture movements, comparable to that of a fixed prosthesis, while also reducing the wear of the attachment system and veneering material. This design, which permits a vertical path of insertion, may ease the removal of the prosthesis, and may be advantageous for elderly patients with reduced dexterity.20
A supportive periodontal therapy program that includes radiographic assessment for the first 5 years, and then every 3 years thereafter or when needed, supragingival polishing, subgingival instrumentation with titanium scalers, chlorhexidine disinfection, and continuous and repeated oral hygiene instruction, will help to achieve long-term survival and success with implant overdenture therapy.19
Patient Profile
The case presented is a 73-year-old female with well-controlled hypertension and hypercholesterolemia. (Fig. 9) She had a 12.5 pack-year history of smoking and was considering quitting. The patient had received a full maxillary clearance and fixed implant bridgework 10 years prior. The implants later experienced peri-implantitis and an open flap debridement as well as implant thread plasty was performed 5 years later. Peri-implant health was restored temporarily, however the peri-implant abscesses later re-occurred. During this time the remaining mandibular dentition had also become symptomatic. The patient’s primary concern was that she wanted to try to restore health again to her implants. Her secondary concern was that she was considering an implant solution to replace her remaining lower teeth.
Fig. 9

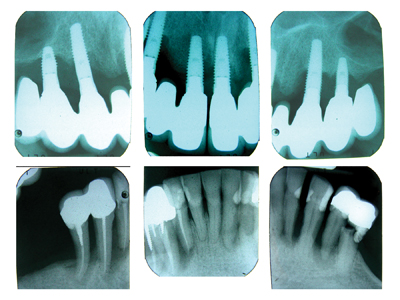
Clinical and Radiographic Assessment
Remaining dentition was diagnosed with generalized stage IV periodontitis. (Fig. 10-11) All previous maxillary teeth were suspected to have been lost due to periodontitis. Endodontic-periodontal lesions were suspected at teeth 34, 32, 42, 43, and 44. There was recurrent decay at teeth 35, 34, 33, 32 and 42. Existing fixed implant bridgework in the maxilla was failing due to peri-implantitis, with severe loss of the remaining supporting bone. There was a severe loss of both the maxillary labial vestibule and peri-implant buccal keratinized tissue.
Fig. 10

Fig. 11
Cone Beam CT Scan
The scan was taken using radiographic templates. (Fig. 12) There was severe bilateral pneumatization of the posterior maxilla. There were no contra-indications to sinus augmentation, except for the proximity of implants 14 and 24, which if not explanted could act as potential sources of infection for the bone graft. Residual ridge height in the mandible appeared adequate for implant placement, however inter-foraminal bone volume was reduced due to the widespread endodontic-periodontal lesions. All implants except for 23 had a severe loss of facial supporting bone. (Fig. 13) Implants 14, 13, and 24 also had a severe loss of palatal supporting bone. Figure 14 demonstrates the simulated future implants 16-26, as well as their apical and palatal position relative to the existing implants 21 and 23. Significant horizontal and vertical guided bone regeneration would be required to reduce the deficiency and permit implant placement for repeat traditional fixed implant bridgework that would avoid a facial cantilever. Figure 15 demonstrates the overall simulated implant plan. Six implants with a maximum anteroposterior distribution were planned in both the maxilla and mandible, to increase the chances of long-term treatment success with future implant overdentures, in light of the patients’ history of periodontal disease and peri-implantitis.
Fig. 12
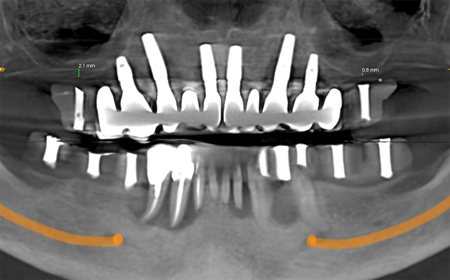
Fig. 13

Fig. 14

Fig. 15

Treatment Plan Discussion
The risks and benefits of a staged surgical and prosthetic replacement of the remaining implants and natural dentition with removable implant overdentures were discussed with the patient. Treatment would involve multiple surgeries to regenerate both missing hard and soft tissue in the maxilla to permit repeat implant placement and would have a total duration of over one year. The patient was advised that the long-term prognosis of any repeat treatment to restore health to her existing implants was hopeless, and that their removal was recommended. Removable implant overdentures were recommended to allow accessibility for home and professional plaque control, and to help reduce her susceptibility to repeat peri-implantitis. The patient was highly encouraged to quit smoking. As discussed, and acknowledged the past history of periodontitis, peri-implantitis and smoking put the patient in a high risk group for recurrence and overall failure, in spite of all efforts to overcome them. Informed consent was obtained.
Surgical Treatment
All procedures were performed under intravenous moderate conscious sedation, for optimal patient comfort and recovery. Treatment in the mandible was delivered in 2 procedures, spaced 6-weeks apart. (Fig. 16) Remaining mandibular teeth were extracted and a provisional complete denture with soft liner was inserted. In the second procedure, the radiographic stent was converted into a surgical stent by removing the radiopaque markers. An alveoloplasty was done to increase ridge width and to create a platform for better visualization and management of the osteotomy sites. A buccal osseous concavity remained at implant sites 43 and 45. Straumann© S SLA implants were used. Implant sites and corresponding dimensions were: 37 & 47 (4.8x6mm WN), 35 & 45 (4.8x6mm RN), 33 & 43 (4.1x12mm RN). Particulate xenograft (Bio-Oss© – Geistlich) was used to graft the exposed 43 and 45 implant surfaces and remaining buccal concavity. (Fig. 17) A resorbable collagen membrane (Mem-Lok©–BioHorizons) was draped over the implants. Site closure was achieved using a combination of chromic gut absorbable sutures and monofilament poly-tetra-fluoroethylene non-absorbable sutures (Cytoplast™–Osteogenics). The patient was seen at 1-week, and 1-month for post-operative checks. The site showed favourable healing at 1-month post-operative, without signs of infection, and with an adequate amount of peri-implant KT. (Fig. 18)
Fig. 16
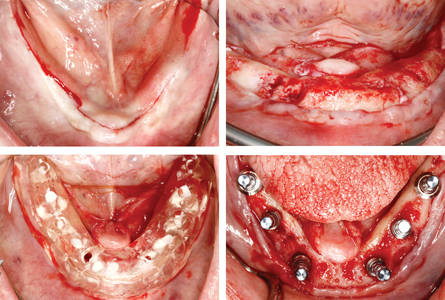
Fig. 17

(Bio-Oss© – Geistlich) and a resorbable collagen membrane (Mem-Lok©–BioHorizons). Site closure and radiographs.
Fig. 18

Treatment in the maxilla was delivered in five stages. During the first procedure, the bridge was sectioned and polished at the distal aspect of sites 13 and 23. Implants 14 and 24 were then explanted. (Fig. 19) In the second procedure 6 weeks later, a bilateral direct sinus augmentation (open lateral wall approach) was performed. (Fig. 20) Internal and external resorbable collagen membranes (Mem-Lok©–BioHorizons) were used to house the grafted bone. A 50/50 ratio of particulate xenograft (Bio-Oss© – Geistlich) and allograft (MinerOss©–BioHorizons) was used. Site closure was achieved using a combination of chromic gut absorbable sutures and monofilament poly-tetra-fluoroethylene non-absorbable sutures. The patient was seen at 1-week, and 1-month for post-operative checks. Figure 21 shows a CBCT comparison of the pre-operative and 8-month post-operative grafted ridge dimensions.
Fig. 19

Fig. 20

Fig. 21

A gingival onlay graft was performed across sites 14-24 buccal 2-months following the sinus augmentation. (Fig. 22) A partial-thickness flap was reflected and secured apically at the recipient site. Epithelium-connective tissue grafts, harvested from the bilateral hard palate, were secured at the recipient sites with 5-0 chromic gut absorbable sutures. The donor sites were coapted with 4-0 chromic gut absorbable sutures. Coe-PakTM periodontal dressings lined with Cyanoacrylate oral adhesive (PeriAcryl®–Citagenix) were used to cover the donor sites. The patient was seen for 1-week, 2-week, and 2-month post-operative checks. A comparison of the initial site and 2-month postoperative follow-up shows that the graft had revascularized. (Fig. 23) A wide zone of keratinized tissue was achieved and the vestibule was deepened across sites 12–23. The donor site showed complete regeneration of the harvested tissue, with minimal evidence of scarring.
Fig. 22

Fig. 23

showing an increase in width of the keratinized tissue and deepening of the maxillary labial vestibule.
Figure 24 shows mounted models in occlusion using the patient’s mandibular provisional denture. Prosthetic teeth were then waxed into position. A radiographic stent was then fabricated. 8-months following sinus augmentation, the patient received both a post-graft CBCT scan and intraoral scan. Measurements taken at all implant sites revealed sufficient interocclusal space for an implant-supported bar overdenture. CoDiagnostiX© software was used to merge the intraoral scan and cone beam CT (CBCT) image and create a virtual diagnostic wax-up of a future implant-supported bar overdenture. (Fig. 1) Upon review of the virtual wax-up it was decided to use bone level as opposed to tissue level implants to help maximize the available inter-occlusal space. A CAD-CAM implant surgery guide was then simulated. (Fig. 25)
Fig. 24

Fig. 25
The remaining implants were removed, and the new implants were installed using the guide 9-months following sinus augmentation. (Fig. 26) Straumann© BL implants were used. Implant sites and corresponding dimensions were: 16 & 26 (4.8x12mm RC), 14 & 24 (4.1x8mm RC), 12 & 22 (3.3x10mm NC). Particulate xenograft was used to graft the exposed implant surfaces and the previous implant osteotomies. (Fig. 27) Site closure was achieved using a combination of chromic gut absorbable sutures and monofilament poly-tetra-fluoroethylene non-absorbable sutures. A provisional complete denture with soft liner was inserted. The patient was seen for 1-week, and 1-month for post-operative checks. The implants were uncovered and osseointegration was verified 3-months following placement. (Fig. 28)
Fig. 26

Fig. 27

Fig. 28

Prosthetic Treatment
Due to COVID-19 prosthetic treatment has been delayed. Prosthetic treatment will follow in a later publication.
Conclusion
This case report discussed a staged surgical and prosthetic replacement of both failing implants and natural dentition with removable implant overdentures. The number of implants to support the overdentures was evidence based and the surgeries were planned and executed under three-dimensional assessment precise guidance. Treatment involved multiple surgeries to regenerate both missing hard and soft tissues in the maxilla to permit repeat implant therapy. This report highlighted the importance of how virtual planning software assists in the surgical-restorative collaboration, and how it allows all dental care providers to be involved and provide input from the beginning, ensuring a comprehensive diagnosis and treatment plan. This leads to an improved outcome for the patient. With such an extensive treatment plan it is important to spend time with patient and review their understanding of the different steps in the plan, and why each particular step is important relative to the remainder of the treatment. In this way we will help to ensure a healthy balance between likely outcomes and their expectations. Monitoring and maintenance after treatment completion is of paramount importance in all cases, but is especially important in this high-risk case.
Oral Health welcomes this original article.
References
- Goncalves F, et al. Effect of the attachment system on the biomechanical and clinical performance of overdentures: A systematic review. The Journal of Prosthetic Dentistry. 2020; 123: 589-594.
- Tatakis DN, et al. Guided implant surgery risks and their prevention. Periodontology 2000. 2019; 81: 194-208.
- Gallucci GO, et al. Maxillary Implant-Supported Fixed Prosthesis: A Survey of Reviews and Key Variables for Treatment Planning. The International Journal of Oral & Maxillofacial Implants. 2016; 31(suppl): s192-s197.
- Misch CE, editor. Dental Implant Prosthetics, 2nd Edition. St. Louis: Elsevier Mosby; 2015.
- Testori T, et al. Risk factors in lateral window sinus elevation surgery. Periodontology 2000. 2019; 81: 91-123.
- Del Fabbro M, et al. Long-Term Implant Survival in the Grafted Maxillary Sinus: A Systematic Review. The International Journal of Periodontics & Restorative Dentistry. 2013; 33: 773-783.
- Moy PK, et al. Risk factors in bone augmentation procedures. Periodontology 2000. 2019; 81: 76-90.
- Chrcanovic BR, et al. Survival and Complications of Zygomatic Implants: An Updated Systematic Review. Journal of Oral and Maxillofacial Surgery. 2019; 77: 1147-1151.
- Araujo RZ, et al. Clinical outcomes of pterygoid implants: Systematic review and meta-analysis. Journal of Cranio-Maxillo-Facial Surgery. 2019; 47: 651-660.
- Esposito M, et al. Interventions for replacing missing teeth: dental implants in zygomatic bone for the rehabilitation of the severely deficient edentulous maxilla (Review). The Cochrane Library. 2013; 9: 1-15.
- Chackartchi T, et al. Soft tissue-related complications and management around dental implants. Periodontology 2000. 2019; 81: 124-138.
- Longoni S, et al. Effect of Peri-Implant Keratinized Tissue Width on Tissue Health and Stability: Systematic Review and Meta-analysis. The International Journal of Oral & Maxillofacial Implants. 2019; 34: 1307-1317.
- Kern JS, et al. A systematic review and meta-analyses of removable and fixed implant-supported prostheses in edentulous jaws: post-loading implant loss. Clinical Oral Implants Research. 2016; 27: 174-195.
- Sadowsky SS, et al. Protocols for the Maxillary Implant Overdenture: A Systematic Review. International Journal of Oral & Maxillofacial Implants. 2016; 31(suppl): s182-s191.
- Carpentieri J, et al. Hierarchy of restorative space required for different types of dental implant prostheses. Journal of the American Dental Association. 2019; 150: 695-706.
- Laverty DP, et al. Implant retention systems for implant-retained overdentures. British Dental Journal. 2017; 222: 347-359.
- Geudat C, et al. Clinical performance of LOCATOR attachments: A retrospective study with 1-8 years of follow-up. Clincial and Experimental Dental Research. 2018; 4: 132-145.
- Boven GC, et al. Maxillary implant overdentures retained by use of bars or locator attachments: 1-year findings from a randomized control trial. Journal of Prosthodontic Research. 2020; 64: 26-33.
- Cortellini S, et al. Patient compliance as a risk factor for the outcome of implant treatment. Periodontology 2000. 2019; 81: 209-225.
- Pozzi A, et al. Four-implant overdenture fully supported by at CAD-CAM titanium bar: A single cohort prospective 1-year preliminary study. The Journal of Prosthetic Dentistry. 2016; 116: 516-523.
About the Author
 Dr. Valentin Dabuleanu maintains a private practice in Toronto limited to periodontics and implant surgery in a combined periodontal and endodontic practice with Dr. Mary Dabuleanu, Endodontist, and alongside the family practices of Dr. Tudor Dabuleanu and Dr. Emilia Nicola, General Dentists. Valentin is a Fellow of the Royal College of Dentists of Canada in Periodontology. He obtained his DDS from the University of Toronto in 2010, and subsequently completed a general practice residency at Vancouver General Hospital. Valentin completed his MSc degree and speciality training in Periodontology at the University of British Columbia in 2014. He can be reached at valentindab@gmail.com.
Dr. Valentin Dabuleanu maintains a private practice in Toronto limited to periodontics and implant surgery in a combined periodontal and endodontic practice with Dr. Mary Dabuleanu, Endodontist, and alongside the family practices of Dr. Tudor Dabuleanu and Dr. Emilia Nicola, General Dentists. Valentin is a Fellow of the Royal College of Dentists of Canada in Periodontology. He obtained his DDS from the University of Toronto in 2010, and subsequently completed a general practice residency at Vancouver General Hospital. Valentin completed his MSc degree and speciality training in Periodontology at the University of British Columbia in 2014. He can be reached at valentindab@gmail.com.
To read more from the 2020 Periodontics issue, please click here!












