Introduction
Many years ago Dr. David Garber was quoted saying, “Soft tissue is the issue, but bone sets the tone.” By the end of this opinion piece the reader should understand that this statement proves to be an important consideration in the modality of retention of implant prosthetics. The debate comparing mechanical (screw) retained, and cohesively (cement) retained implant restorations is as old as implant dentistry itself. The literature is replete with articles and systematic reviews of varying quality comparing these two retention modalities.1 The conclusions made are universally similar; that is, there is no statistical difference in the survival and/or success rates of the particular implant prosthesis being compared, and that none of the fixation methods were clearly advantageous over the other.2 As well, the literature suggests that complication rates are essentially identical. This leaves the clinician to choose. In order to help make this choice more evidence based3 and less literature based, or even worse preference based. This article will be delving into the critical factors that need to be considered to make a well-informed decision. It is well known that in order to practice evidence-based dentistry one must treatment plan with a three-pronged approach. The savvy clinician should balance the best evidence, his personal preferences (based on his skill set or the skill set of his referral network), and the informed patient’s wishes/desires (adequate aesthetics, function, speech, longevity, cost etc.) When these three legs are firmly in place and balanced, they will provide a stable foundation for an evidence-based treatment plan. The factors that are traditionally discussed and will be briefly highlighted in this article are: aesthetics, retention/resistance, retrievability, passivity, provisionals, occlusion, soft tissue health
The purpose of this article is to briefly summarize the advantages, disadvantages and the limitations of the two systems used to secure a fixed dental prosthesis onto a dental implant, that is, cohesion vs. screw retention. As well, a secondary purpose is to present and discuss a novel reason proposed as a distinct conceptual advantage to the surgical placement of a dental implant in a manner that could be restored via abutment screw retention, that would allow for a more certain long term functional and aesthetic success.
AESTHETICS:
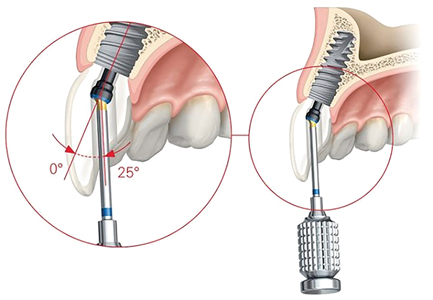
A well-made implant prosthesis that is being retained by cement will always have the potential to be more aesthetic than a screw retained implant prosthesis. This is due to the fact that a screw retained prosthesis by definition will always have a screw channel to contend with. Even if this is expertly camouflaged by an experienced and conscientious clinician, over time the margin between the porcelain and the resin tends to stain thereby leaving a less aesthetic prosthetic when looking at the prosthesis in isolation. Thankfully, with the advent of the angled screw channel (Fig. 1) most screw retained prosthesis can be made to have aesthetics that will leave most patients and clinicians satisfied with the aesthetics. The main reason for this is the satisfaction of the aesthetics of an implant prosthesis has little to do with the existence of a screw access channel. Patient satisfaction with aesthetics is mostly dependent on implant position, tissue volume and type surrounding the implant, and as always patient selection.
Fig. 1
RETENTION/RESISTANCE:
Similar to core supported crown and bridge, retention of a cement retained implant prosthetic is largely dependent on the geometry of the abutment and less so on the type of cement utilized. The clinician and laboratory should focus on the tooth preparation principles of retention and resistance when designing an implant abutment to maximize the cohesive qualities of the cement. In a screw retained prosthesis, the level or retention is dependent on the geometry of the connection (either internal or external) and is therefore implant specific. As well, it is dependent on the clamping force or preload applied to the screw while tightening and securing the prosthesis in place. This is dependent on thread geometry as well as the alloy used to manufacture the abutment or prosthetic screw. Retention failure can and does occur in both modalities. In cemented restorations, a cohesive failure can occur requiring the prosthesis to be recemented. Alternatively, failure can occur when the abutment screw loosens, without a cohesive failure of the cement. This becomes more challenging due to the resultant financial consequences of modifying and in fact sometimes sacrificing/replacing the cemented prosthesis as is often needed. Therefore, the factors of screw retention are generally controlled by the manufacturer while the factors controlling cement retention is largely controlled by whims of the clinician and/or lab technician.
RETRIEVABILITY:
The ability to remove a prosthesis in a non-destructive manner is of utmost importance in implant dentistry. During the life of an implant prosthesis, the clinician may find it needs to be removed for hygiene, fracture repairs, design modifications and abutment screw tightening. Removing a screw retained prosthesis is as simple as gaining access to the screw and unscrewing it. A multiple unit cement retained prosthesis can be removed in a non-destructive manner however doing so is much less predictable and much more time consuming. Removing a cemented single crown is very unpredictable and many times the crown is damaged as a consequence.
PASSIVITY:
Passivity of fit is crucial in implant prosthetics in order to minimize the concentration of off angle forces transmitting down the implant potentially resulting in bone loss worse a loss of osteointegration as a consequence. In general, it is desirable to have a passively fitting framework that will allow the screw to exert the appropriate amount clamping force to hold components together firmly in a screw retained prosthesis. As well, a passively fitting framework will not cause strain to the interface between the implant and bone. Unfortunately, a totally passive framework is difficult to achieve due to the variable sources of error during the laboratory processes. As such, it is safe to assume that many if not most of the frameworks that are in place and functioning are not totally passive. In screw retained prosthesis passivity is improved by splinting the units intraorally when making impression or by checking the fidelity of the master cast with verification jigs. As digital technologies (digital impressions, CAD/CAM manufacturing) improve, they remove many of the inherent errors of material-based master cast fabrication. We are seeing improved fit and increased passivity of screw retained frameworks as a benefit. Another way to minimize the passivity of a framework in an implant prosthesis is to utilize cohesion as the mode of retention. In a cohesive or cement retained prosthesis, the abutments are individually retained to the implants by screws and the super structure is cemented over the abutments. The cement space between the bridge and the abutments allows for a passive fit. In fact, the less accurate the casting, and the less resistance/retention form that the abutment has, the greater the passivity of fit. This leads to reliance of cement to retain the prosthesis, therefore requiring a more permanent, less soluble cement system. This can lead to negative peri-implant response if the excess cement is not fully removed. A hybrid of these 2 approaches that can help to avoid the complications of excess cement is the so-called screwmentable hybrid prosthesis whereby a zirconia superstructure is cemented onto an abutment in the laboratory and screw retained in the mouth. (Fig. 2)
Fig. 2

PROVISIONALS:
When restoring implants in the aesthetic zone a provisional restoration should be used to shape and mold the tissue in order to achieve the gingival contours necessary for ideal aesthetics. The use of a screw retained interim prosthesis, will predictably and efficiently apply the amount of pressure required to accomplish this task. A cement retained prosthesis cannot predictably apply the amount of pressure that may be required to expand the peri implant mucosa leading to a less than desired aesthetic outcome.
OCCLUSION:
It is undeniable that the screw access can obliterate a portion of the occlusal surface of posterior teeth by occupying its precious real estate. As such, it can create an unsightly blemish on the occlusal surface of a restoration, and theoretically has the potential to affect its’ occlusal scheme. It is the authors experience that this does not seem to cause a significant disadvantage in a well-designed screw retained prosthesis. In an anterior screw retained implant prosthesis the screw channel is directed towards the lingual and, as such, does not play an integral part in the occlusal design. With the new angled screw channel, the screw access can be moved into an area that will minimize any negative occlusal effect if need be. A cohesively retained implant prosthesis by contrast does not have a screw access channel and as such has no break in its’ occlusal surface, therefore allowing for a theoretically optimal occluding surface.
SOFT TISSUE HEALTH:
The health and stability of the peri-implant mucosa is of utmost importance in both the success and survival rate of the implant and its’ prosthesis. As well, stable peri-implant mucosa will allow for an aesthetic result that is predictable over time. It is well documented that a significant cause of peri-implant mucositis is the inadequate clearance of all excess cement. This cement gets trapped into the sulcus. In many situations this leads to peri implant osteitis and possible implant loss as a consequence. This risk is completely eliminated when the clinician chooses to screw retain an implant prosthesis.
SCREW RETENTION FOR STABLE GINGIVAL ARCHITECHTURE in the AESTHETIC ZONE: A novel concept
The decision on the retention modality employed to restore an implant in the aesthetic zone is many times decided at the lab bench long after the implant was placed. The decision is essentially based on the trajectory of the screw access channel. If the trajectory is lingual to the incisal edge screw retention is possible. If the trajectory is at or buccal to the incisal edge and cannot be hidden, then the crown would typically be cement retained to avoid the aesthetic complication. (Fig. 3) Most recently the Angled Screw channel corrects much of this and allows many previously cement-retained crowns to be screw-retained for the purpose of satisfying the factors discussed in this article. An alternative and not often discussed reason to design our prosthesis with screw retention will be illustrated and explained as follows.
Fig. 3

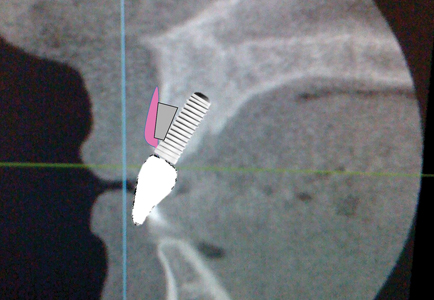
If an implant is placed in a manner that would necessitate a cement retained crown due to the location of the screw access channel, we would have a situation like the hypothetical one seen in Figure 4. Because the implant is tipped buccally, thereby not allowing for screw retention, the amount of buccal bone is minimized at the crest. Many times, creating an inverted triangle as the bone is thinnest at the crest. (Fig. 5) In spite of the thin crestal bone an adequate restoration with adequate soft tissue can usually be expected. (Fig. 6) Occasionally however, due to multitude of factors including the remaining thickness of the bone, crestal bone can be lost. (Fig. 7) If the patient is fortunate enough to have a thick gingival biotype, or if the savvy clinician soft tissue grafted to increase the thickness of tissue, then the aesthetic consequences can be minimal. (Fig. 8) However, if the patient has thin gingival biotype and/or the clinician did not increase its thickness the result can be devastating for the patient, especially one with high lip dynamics. (Fig. 9)
Fig. 4

Fig. 5
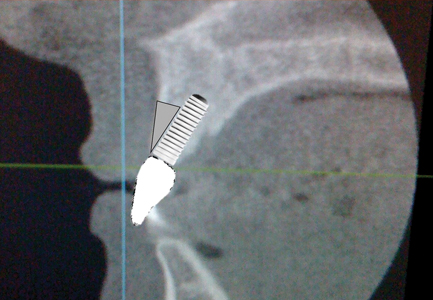
Fig. 6
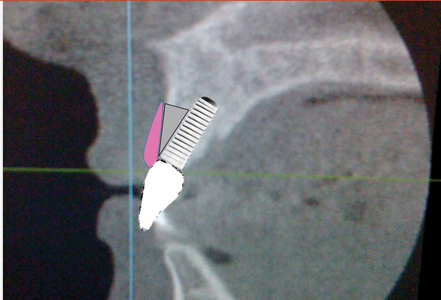
Fig. 7

Fig. 8

Fig. 9
By contrast, if the implant was placed and restored successfully with a screw retained solution that did not require an angled screw channel, the amount of buccal bone at the crest would be maximized. This would lead to more stable buccal gingival architecture which is known to be crucial for a long term aesthetically successful implant restoration. If the “tissue is the issue, but the bone set the tone” then the primary focus should always be to maximize the amount of buccal bone at the crest of the implant.
In conclusion, it is the authors opinion that when placing implants in the aesthetic zone, the surgeon and restoring clinician should always insist on restoring the implant with a screw retained crown. This would satisfy the prosthetic convenience of retrievability, eliminate the negative consequences to the peri-implant mucosa due to excess cement, as well as creating a long-term aesthetic outcome by maximizing the amount of crestal buccal bone thereby creating a stable gingival architecture.
Oral Health welcomes this original article.
References
- Sailer I, Mühlemann S, Zwahlen M, Hämmerle CHF, Schneider D. Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. Clin. Oral Implants Res.23(Suppl. 6), 2012, 163–201.
- Gaddale, R, Mishra SK, Chowdhary R. Complications of screw- and cement-retained implant-supported full-arch restorations a systematic review and meta-analysis. Int J Oral Implantol 2020; 13(1): 11-40.
- Richards, D., Lawrence, A. Evidence based dentistry. Br Dent J 179, 270–273 (1995).
About the Author
 Dr. Joseph Fava earned his undergraduate dental degree, masters degree and prosthodontic specialty certificate at the University of Toronto. He currently maintains a private prosthodontic specialty practice in the Yorkville and Forest Hill area of Toronto with emphasis and focus on aesthetic and implant dentistry. He is a clinical instructor in the graduate prosthodontics program at the University of Toronto and enjoys being involved in clinical research. His scope of practice includes cosmetic dentistry, surgical and prosthetic components of dental implants and advanced restorative and reconstructive full mouth therapies. He is a distinguished Kois Mentor and the Co-director of the University of Toronto’s Implant Residency Program.
Dr. Joseph Fava earned his undergraduate dental degree, masters degree and prosthodontic specialty certificate at the University of Toronto. He currently maintains a private prosthodontic specialty practice in the Yorkville and Forest Hill area of Toronto with emphasis and focus on aesthetic and implant dentistry. He is a clinical instructor in the graduate prosthodontics program at the University of Toronto and enjoys being involved in clinical research. His scope of practice includes cosmetic dentistry, surgical and prosthetic components of dental implants and advanced restorative and reconstructive full mouth therapies. He is a distinguished Kois Mentor and the Co-director of the University of Toronto’s Implant Residency Program.
RELATED ARTICLE: Predictable Immediate Implant Prosthetics: Part 2












