To view figures, click on figure mentions throughout the article.
This article is the fourth in a series by the author submitted to, and published exclusively by Oral Health. The first article of the series was published in the August 2015 issue with the title: Surgical Risk Factors in Implant Dentistry: Influence on Failures and Bone Loss. That first article organized risk factors in implant dentistry into four major categories (Table 1), reviewed the concept of evidence-based dentistry and illustrated some of the risk factors with the author’s cases. The second article published in the August 2016 Oral Health issue focused on the influence of the first of the four risk factor categories namely “Patient Related Systemic Risk Factors”. That second article also described the importance of patient informed consent and emphasized how the knowledge of risk factors was a crucial prerequisite to achieving informed consent. As well several risk factors in that category were illustrated with some of the author’s cases. The third article published in the August 2017 Oral Health issue, covered some risk factors in the second of the four risk factor categories namely: “Patient Related Local Risk Factors” and again several of the author’s cases were illustrated. This current fourth article will discuss the third group of the risk factor categories as seen in Table 1 and expanded upon in Table 2 in this article, namely “Operator Related Risk Factors”. Future articles will cover more topics in this third, and also the fourth of the four categories namely “Biomaterial Related Risk Factors” (Table 1).
Table 1
Risk Factors in Implant Dentistry
1) “Patient Systemic” Related Risk Factors
- Unrealistic expectations e.g. esthetics, Psychological status, Non-compliance e.g. oral hygiene and professional re-care, Limits e.g. financial, History of aggressive periodontitis, Smoking (dosage), Certain systemic diseases and medications
2) “Patient Local” Related Risk Factors
- Soft and or hard tissue deficient quality and or quantity, “High” smile zone, Lip length-support, Restorative space available, Malocclusion, Parafunction
3) “Operator” Related Risk Factors (see Table II for more detail)
- Operator experience and expertise, Techniques and Protocols: e.g. asepsis, antibiotics, surgically-induced trauma, implant malposition, implant over-size vs. available bone, 1 vs. 2-stage, immediate vs. delayed implants, failed replacements, biomechanically related risks: e.g. occlusion, number of implants, splinting, implant to crown ratio, cantilevers, appliance
prescription, Prosthesis design, Prosthesis fabrication materials and Prosthetic Protocols
4) “Biomaterials” Related Risk Factors
- Implant material e.g. titanium grade, Microscopic implant surface, Macroscopic design e.g.: threads, intraosseous portion, crestal module, prosthetic connection e.g.: flat external vs. internal vs. conical, flush fit vs. platform switch.
Operator Related Risk Factors (Table 2)
This category of risk factors includes but is not limited to operator related issues as outlined in more detail in Table 2. Concerning the operator’s experience and expertise, one might expect that there is a “learning curve” in developing surgical expertise. In fact, some studies have indicated this. Of note the results from a recent Systematic Review and Meta-Analysis has been consistent with the concept of a “learning curve” and specifically with an association of expertise related to the number of implants placed. 1 Some other risk factors related to “Surgical Techniques and Protocols” are discussed and illustrated below.
Table 2
Operator Related Risk Factors
Experience / Expertise
- Surgical Techniques and Protocols:
- Aseptic vs. hospital level surgical sterility
- Antibiotic prescription: pre-op, post op or none
- Flap Design: (Visor vs. Crestal vs. Flapless)
- Surgical Trauma (related to implant placement):
- Excessive heat related to osteotomy drilling
- Excessive compression of the implant on thin bone
- Poor implant to bone congruency (poor fit/stability)
- Implant Malposition:
- Oro-facially /Mesio-distally /Apico-occlusally
- Penetration into anatomic sites e.g. nasal cavity, sinus, inferior alveolar nerve, cortical bone plate
- Placement: 1 stage (exposed) vs. 2 stage (submerged)
- Immediate implant placement: technique, indications, contraindications, anterior vs. posterior sites, risks with residual infection and or residual root fragments
- Failed implant Replacement: efficacy of 2nd or 3rd attempts, timing: immediate replacement vs. delayed replacement
- Prosthetic Techniques and Protocols:
- Immediate vs. Delayed Restoration and Loading
- Supporting implants: number, size, design and position
- Splinting, Cantilevers, Occlusion, Occlusal Guards
- Ratio: crown length to implant length
- Prosthesis materials and prosthesis design
- Implants connected to natural teeth
Surgical Techniques and Protocols
Aseptic vs. Hospital Level Sterility for Implant Surgery
The original “Branemark” protocol included a hospital level sterility protocol for routine implant placement. 2 Within a short time, studies showed equivalent success rates when utilizing routine dental aseptic techniques. 3,4 Subsequently all the implant companies including Nobelpharma, endorsed an aseptic technique for implant placement.
Antibiotic Prescription: Pre-op, Post-op or None
Many surgeons prescribe antibiotics for routine implant surgery but there is some contradictory evidence on the importance of their use pre-operatively or peri-operatively. 5 Of note, Chrcanovic et al 6 in 2014 published a systematic review and meta-analysis on this. There were 14 studies included and when the data was combined the conclusion was that there was no difference in post-operative infections rates. However, some of the individual studies did show about a 2% reduction in implant failures. In conclusion, there seemed to be some evidence for the benefit of prophylactic antibiotics for routine implant surgery and some evidence indicates that the benefit may be primarily attributed to the pre-surgical antibiotic dose rather than the post-operative dosages, especially considering they had no effect on the post-operative infection rates.
Flap Design: (Visor vs Crestal vs Flapless)
The original “Branemark” surgical technique included a submerged or one stage protocol utilizing a “Visor” incision (Fig. 1) which was located well facial from the crest of the ridge. The rationale for this was to keep the location of the incision and sutures distant from the implant sites. Unfortunately, with this type of incision there was often significant swelling and bruising (author’s experience).
Currently in most cases, a crestal or para-crestal incision has become the routine incision design with both one stage and two stage implant placement protocols. Typically, patients have minimal if any swelling and bruising with this type of incision (author’s experience). Studies have shown that there is no difference in early implant failure rates comparing the different incision designs. 7 More recently some clinicians have promoted the use of flapless implant surgery (Table 3). While an “immediate” implant placement into an extraction socket can easily be visualized when done “flapless”, there may be significant risks with attempting to place implants “blindly” in a healed ridge with a flapless approach (author’s opinion). See Table 3 for some considerations (both pros and cons) when considering a flapless approach to implant placement in a healed edentulous site.
Table 3
Flapless Implant Placement
- Potential of decreased morbidity and time
- Increased risk of implant malposition
- Potential loss of keratinized gingiva
- Safer when used with CT Scans and guides
- Ideally use computer guided surgery
- Operator needs to know if augmentation is required
- Operator needs to know how to treat complications
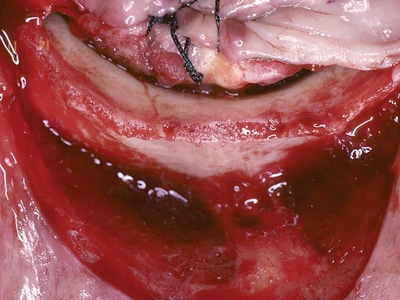
Fig. 1
The Visor incision was placed well facial to the bone crest to distance the incision and sutures from the implants. Often there was significant swelling and bruising.
Surgical Trauma (related to implant placement)
Excessive Heat Related to Drilling
Dental implant surgical techniques are routinely incorporated to minimize the risk of overheating the bone during drilling e.g. use of copious irrigation, sharp drills and an intermittent light drilling technique. 8 See Figures 2A, 2B, and 2C for a rare case that likely demonstrates overheating. The author suggests that the implant failures in this case were due to an equipment deficiency that resulted in the drilling inadvertently being carried out in “reverse”. The subsequent traumatic drilling technique likely led to overheating of the bone which in turn likely resulted in bone necrosis and subsequent early implant infection, bone loss and implant failure.
Fig. 2A
Initial osteotomies (done with inadvertent “reverse” drilling).
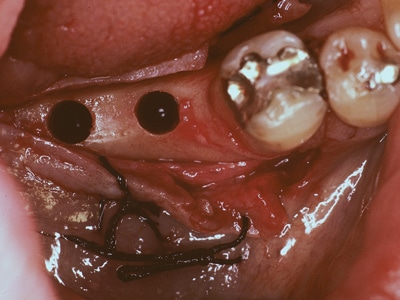
Fig. 2B
Infected implant sites seen at 5weeks post implant placement.

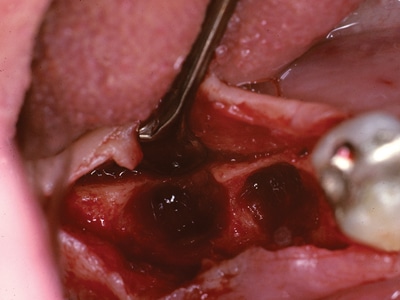
Fig. 2C
Osteotomy sites after implant removal at five weeks post placement.
Excessive Bone Compression
The concept of “pressure necrosis” has been anecdotally proposed by some, with the hypothesis that excessive implant insertion torque can cause cortical bone necrosis, bone loss and implant failure. This concept perhaps has been reinforced by the fact that most implant motors deliver a maximum torque of about 50 Ncm. Unfortunately, this concept has not been clearly elucidated in the literature. To confuse matters more, some studies have shown there was no deleterious effects when implants were inserted with up to 150Ncm. 9,10,11 However anecdotally and in the opinion of the author, clinical experience has shown that in the situation where there is implant compression on the thin facial labial cortical plate of bone, there is a higher risk for implant gingival recession (Figs. 4A-4F) bone loss and failure.
Fig. 4A
Labial angulation of implant evident from occlusal view.

Fig. 4B
Labial recession and longer clinical crown at 2.2.

Fig. 4C
Different case with apical exposure of the healing abutment.

Fig. 4D
Connective tissue graft placed to “cover” exposure.

Fig. 4E
Restoration showing “coverage” and acceptable esthetics.

Fig. 4F
Radiograph of 5mm diameter implant final restoration.

Poor Implant to Bone Congruency
(i.e. poor initial fit and or poor initial stability)
Over drilling the diameter of the implant osteotomy can result in poor congruency between the implant and adjacent bone osteotomy site. This in turn can lead to poor initial stability, early micromotion and a higher risk of non-osseointegtation especially with smoother implant surfaces. 12-14 It is the author’s opinion that initially placed relatively unstable implants, that subsequently seem to osseointegrate, may have a higher risk of showing “late” progressive bone loss and failure (Figs. 3A-3C). While this has not been well studied, a study on 1,554 Ankylos implants found that implants placed with poor initial stability that seemed to osseointegrate, experienced over 13% late failures at the three years follow up. 14
Fig. 3A
One year post restoration where implants at 34 and 36. Had poor initial stability.
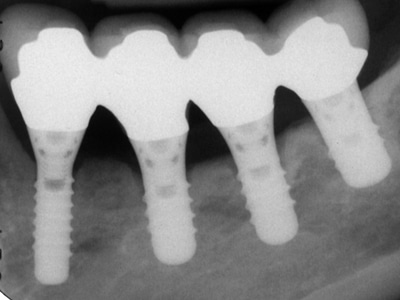
Fig. 3B
16-years post op: implant crestal bone loss at 3.4 and 3.6.

Fig. 3C
18-years post op: explantation of 3.4 and 3.6 due to bone loss.

Implant Malposition
Oro-facially/Mesio-distally /Apico-occlusally
Implant malposition may be the most common operator related risk factor. Malpositioned implants can have an increased incidence of biological complications such as bone loss, implant loss, esthetic and prosthetic complications and even sinus and neurosensory complications. In the oro-facial dimension, the thin facial bone in the maxillary anterior may be more susceptible to damage with resulting gingival recession (Figs. 4A, 4B, 4C, 4D, 4F) bone loss, and possible total implant failure. In the mesio-distal dimension, the most common error is placing two implants in close proximity to each other with the resultant increased risk of recession, bone loss and a lack of an interproximal papilla 15,16 (Figs. 5A & 5B). Narrower implants may improve available mesio-distal spacing (Figs. 5C & 5D). In the apico-coronal dimension, an implant placed far apically may result in deeper periodontal pockets (Figs. 6A & 6B), while an implant placed too superficially may not allow sufficient vertical space for a well contoured restoration (Figs. 7A & 7B).
Fig. 5A
Implants positioned with insufficient mesio-distal space.

Fig. 5B
Restored case exhibiting loss of the interproximal tissues.

Fig. 5C
Narrow implants with limited mesio-distal space.
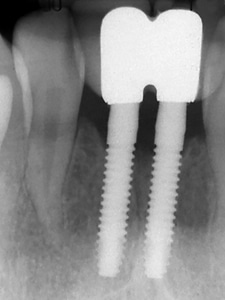
Fig. 5D
Restored implants with better tissue preservation.

Fig. 6A
Implant placed subcrestally with remodelled bone levels.

Fig. 6B
Deeper implant position associated with deeper pockets.

Fig. 7A
Implants positioned supracrestally to avoid “nerve”.
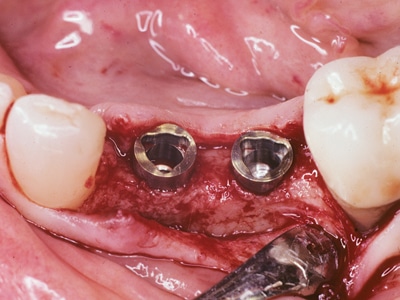
Fig. 7B
Limited vertical space resulted in “short” crowns.

Unintended Penetration into Anatomic Sites: (e.g. sinus, nasal cavity, inferior alveolar nerve, cortical bone perforation)
Unintended implant penetration into the sinus or nasal cavity may not always cause serious signs or symptoms but should be avoided if possible. In contrast, drill or implant penetration into the inferior alveolar nerve presents one of the most serious complications in implant dentistry (Fig. 8A). Strategies to deal with this risk include explicit informed consent, reducing the risk with proper diagnosis (e.g. radiographs), treatment safety features (e.g. drill stops), incorporating a drilling “safety zone”, etc. 17-21 As well, there can be a risk of neurosensory damage with an extraction socket debridement which may precede implant placement (Fig. 8B) (author experience).
The dentist needs to be aware that in some cases where bone loss is extensive, the debridement may encroach upon the inferior alveolar nerve and cause nerve injury. 22,23 Perforation through the cortical plate, (for example through the posterior lingual cortical plate into the sublingual fossa) can result in complications including pain and implant loss (author experience).
Fig. 8A
Implant placed beyond the inferior alveolar nerve.
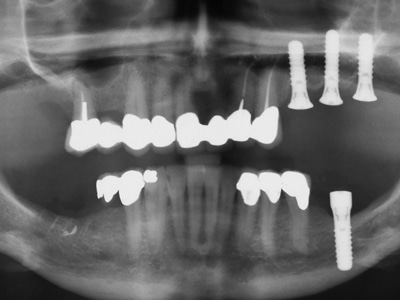
Fig. 8B
4.7 exhibits infection near the inferior alveolar nerve.

1 Stage vs. 2 Stage Implant Placement
The original “Branemark” protocol utilized a two-stage placement (submerged) protocol. Although some early studies may have shown a slightly higher failure rate with the 1 stage (exposed) protocol more recent studies have shown similar success and survival rates. 22,23,24 A 2018 systematic review and meta-analysis 24 concluded there also was no clinical difference in bone loss around implants with either surgical placement protocol (the results actually showed slightly more bone loss with the submerged technique vs. non-submerged). Notably in the late 20th century, the Straumann system promoted the one stage surgical protocol for most cases, with the obvious advantage of eliminating the need to uncover an implant. However, the author believes there are situations where a two-stage submerged protocol may still be considered for example, when initial stability is poor and any forces must be severely minimized and/or when significant bone grafting is carried out concomitantly with implant placement.
Immediate Implant Placement
Immediate implant placement can be discussed in relation to technique, indications, contraindications, anterior vs. posterior sites, and risks with residual infection or root tips. The original “Branemark” protocol suggested a waiting period of six months after extraction before attempting implant placement. Within a short time, many studies and clinical experience lead to the acceptance of immediate post extraction implant placement. While numerous studies have been published on immediate implants, two recent Systematic Reviews with Meta-Analysis confirmed their equivalency. 25,26 Anecdotally many clinicians very commonly incorporate immediate implants, and in the author’s practice immediate implants account for almost 25% of the total number of implants placed. The subject of immediate implants is extremely expansive and multifaceted, and will be the subject of a future article in this Oral Health series where the author will go into more detail on the aspects outlined above.
Failed Implant Replacement
Replacement of a failed implant can be considered in relation to whether it is a second or subsequent replacement attempt and if the replacement of the failed implant is carried out immediately after the implant removal or after a delay to allow healing of the explantation site. Unfortunately, implants do fail and this has been well documented, however, what is less well documented are the implant success and survival rates when replacing implants a second or even a third time. 27,28 Results for second and third time attempts at failed replacements were reported in a 2016 publication by Zhou et al. 27 They reported a survival rate of 88.84% for second attempts and 74.10% for third attempts. What have also not been well reported upon are the relative risks of replacing a failed implant immediately vs. allowing the explanation site to heal before attempting the replacement. However, the author has tracked these results in his practice and found that delayed replacement has yielded better results compared to immediate replacement. Specifically, the author’s statistics are as follows: immediate replacement of 77 failed implants=74% vs. delayed replacement of 193 failed implants =95% (unpublished). While it is clinically more efficient for the dentist and patient to immediately replace a failed implant, based on the above, one should be careful before attempting the immediate replacement technique. Despite this, in the opinion of the author the immediate technique may still be a good option in specific circumstances. For example, the author suggests a CT scan and if there is sufficient bone to place a wider implant, and there are no other contraindications (e.g. infection) then the immediate replacement technique may be justified (Figs. 9A-9B). On the other hand, when there is significant bone loss is associated with a failed implant, a delayed approach to implant replacement is indicated (Figs. 10A-D).
Fig. 9A
CT Scan demonstrates sufficient bone surrounding the fractured implant to allow for a wider diameter replacement.
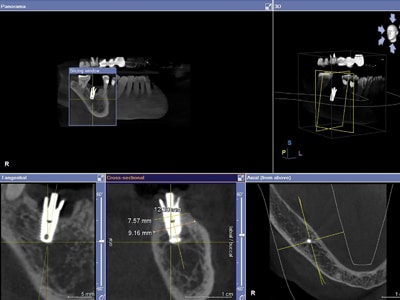
Fig. 9B
Radiograph: The 6mm diameter implant that replaced the fractured 4.7mm diameter implant “immediately”.

Fig. 10A
Failed implant with extensive circumferential bone loss.

Fig. 10B
Several months of healing allowed after removal.

Fig. 10C
10 years post “delayed” implant replacement protocol.

Fig. 10D
10D: 10 years post op delayed replacement final restoration.

Prosthetic Techniques and Protocols
Crown to Implant Ratio: Crown to implant ratio is often mentioned as a potential biomechanical related risk for complications and this concept may have originated from traditional concepts in conventional crown and bridge (and those guidelines may have been empirical and anecdotal). Compared to natural teeth, implants are often shorter, and the corresponding implant prosthetic crowns may be much longer, as often there is significant bone ridge resorption. Contrary to what one might expect, many studies have NOT found deleterious effects of high implant to crown ratios. 29 An exception, however, may be where a high implant crown to implant ratio may be a risk factor for implant loss with un-splinted short implants of 6mm or less (30 and unpublished-author’s experience) (Fig. 11).
Fig. 11
“Late failure” of an un-splinted 6 mm length implant.

Implants Connected to Natural Teeth
There are several potential advantages and disadvantages to take into account when considering splinting implants to natural teeth (Table 4). However, the general consensus seems to be that one should try to avoid this technique. 31 A 2017 Systematic Review and Meta-Analysis 32 including 10 studies found implant survival ranging from 90% to 100%, abutment teeth survival ranging from 94% to 100% and prosthesis survival ranging from 85% to 100%. The most frequent complications were periapical lesions = 11.53% of the natural teeth, porcelain occlusal fracture = 16.6%, screw loosening = 15%, and intrusion with non-rigid connections = 9%. See Figures 12A, 12B, 13A and 13B below, which illustrate two cases where there were rigid connections between implants and natural teeth. The first case (Figs. 12A & 12B) continues to have an excellent long-term outcome (20 years and still ongoing) while the second case (Figs. 13A & 13B) displayed a poor outcome with fractures occurring within five years.
Table 4
Implants Connected to Natural teeth

Fig. 12A
Radiographic view of successful implant (2.1 and 2.2) to tooth (1.3) rigid splint (20 years duration).
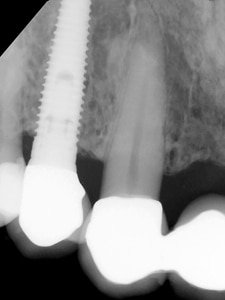

Fig. 12B
Clinical view of successful implant (2.1 and 2.2) to tooth (1.3) rigid splint (20 years duration).

Fig. 13A
Initial restoration: implant to tooth rigid splint.
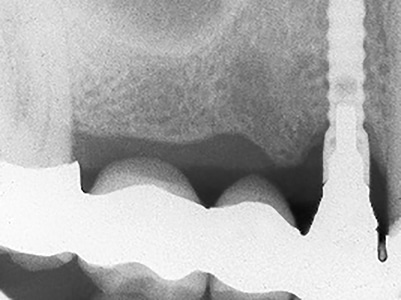
Fig. 13B
Four-year follow-up: Note decay at natural cuspid.
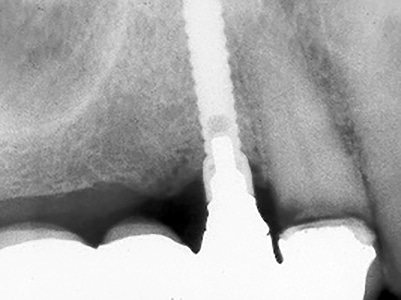
Fig. 13C
Five-year follow-up: Cuspid and implant have fractured.

Fig. 13D
Five-year follow-up: Lost prosthesis with fractured implant.

Prosthetic Techniques and Protocols (continued)
Some additional topics on prosthetic techniques and protocols will be the subject of future articles in this Oral Health series, such as immediate vs. delayed restoration and loading, supporting implants: number, size, design and positioning, splinting, cantilevers, occlusion, occlusal guards, prosthesis materials and designs.
Summary
This fourth article of the series for Oral Health has continued on the subject of “Risk Factors in Implant Dentistry”.
Specifically, this article has discussed the influence of some of the risk factors in the third of fourth categories, “Operator Related Risk Factors”. This article also illustrated some of the author’s cases that incorporated some of the principles and the risk factors discussed. Future articles will cover additional risk factors and will illustrate other cases highlighting more of this third category and additional future articles will cover the fourth category “Biomaterial Related Risk Factors” (Table 1). OH
Oral Health welcomes this original article.
References
- Sendyk DI, Chrcanovic BR, Albrektsson T, Wennerberg A, Zindel Deboni MC. “Does Surgical Experience Influence Implant Survival Rate? A Systematic Review and Meta-Analysis”. Int J Prosthodont. 2017 Jul/Aug; 30(30):341-347
- Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, Ohman A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977; 16:1-132.
- Kraut RA. “Clean operating conditions for the placement of intraoral implants”. J Oral Maxillofac Surg. 1996 Nov; 54(11):1337-8.
- Scharf DR, Tarnow DP. Success rates of osseointegration for implants placed under sterile versus clean conditions. J Periodontol. 1993 Oct; 64(10):954-6.
- Abu-Ta’a M, Quirynen M, Teughels W, van Steenberghe D. Asepsis during periodontal surgery involving oral implants and the usefulness of peri-operative antibiotics: a prospective, randomized, controlled clinical trial. J Clin Periodontol. 2008 Jan;35(1):58-63.
- Chrcanovic BR, Albrektsson T. Prophylactic antibiotic regimen and dental implant failure: a meta-analysis. J Oral Rehabil. 2014 Dec; 41(12):941-56.
- Scharf DR, Tarnow DP. The effect of crestal versus mucobuccal incisions on the success rate of implant osseointegration. Int J Oral Maxillofac Implants.1993; 8(2):187-90.
- Möhlhenrich SC, Modabber A, Steiner T3, Mitchell DA, Hölzle F, Heat generation and drill wear during dental implant site preparation: systematic review. Br J Oral Maxillofac Surg. 2017 Nov; 55(9):985-986.
- Ottoni JM, Oliveira ZF, Mansini R, Cabral AM. Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofac Implants. 2005 Sep-Oct; 20(5):769-76
- Trisi P, Perfetti G, Baldoni E, Berardi D, Colagiovanni M, Scogna G. Implant micromotion is related to peak insertion torque and bone density. Clin Oral Implants Res. 2009 May; 20(5):467-71
- Consolo U, Travaglini D, Todisco M, Trisi P, Galli S. Histologic and biomechanical evaluation of the effects of implant insertion torque on peri-implant bone healing. J Craniofac Surg. 2013 May; 24(3):860-5
- Ivanoff CJ, Sennerby L, Lekholm U. Influence of initial implant mobility on the integration of titanium implants. An experimental study in rabbits. Clin Oral Implants Res. 1996 Jun; 7(2):120-7
- Orenstein IH, Tarnow DP, Morris HF, Ochi S. Factors affecting implant mobility at placement and integration of mobile implants at uncovering. J Periodontol. 1998 Dec; 69(12):1404-12
- Morris HF, Ochi S, Orenstein IH, Petrazzuolo V. Part V: Factors influencing implant stability at placement and their influence on survival of Ankylos implants. J Oral Implantol. 2004; 30(3):162-70.
- Salama H, Salama MA, Garber D, Adar P. The interproximal height of bone: a guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodontics Aesthet Dent. 1998 Nov-Dec; 10(9):1131-41
- Choquet V, Hermans M, Adriaenssens P, Daelemans P, Tarnow DP. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001 Oct; 72(10):1364-71.
- Shavit I, Juodzbalys G. Inferior alveolar nerve injuries following implant placement–importance of early diagnosis and treatment: a systematic review. J Oral Maxillofac Res. 2014 Dec 29; 5(4):
- Greenstein G, Tarnow D. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol. 2006 Dec; 77(12):1933-43.
- Bartling R, Freeman K, Kraut RA. The incidence of altered sensation of the mental nerve after mandibular implant placement. J Oral Maxillofac Surg. 1999 Dec; 57(12):1408-12
- Greenstein G, Carpentieri JR, Cavallaro J. Nerve damage related to implant dentistry: incidence, diagnosis, and management Compend Contin Educ Dent. 2015 Oct; 36(9):652-9
- Jacobs R, Quirynen M, Bornstein MM. Neurovascular disturbances after implant surgery. Periodontol 2000. 2014 Oct; 66(1):188-202.
- Cardelli P, Cecchetti F, Montani M, Bramanti E, Arcuri C. Clinical assessment of submerged vs non-submerged implants placed in pristine bone. Oral Implantol (Rome). 2014 May 19; 6(4):89-93.
- Cecchinato D, Olsson C, Lindhe J. Submerged or non-submerged healing of endosseous implants to be used in the rehabilitation of partially dentate patients. J Clin Periodontol. 2004 Apr; 31(4):299-308.
- Moustafa Ali RM, Alqutaibi AY, El-Din Gomaa AS, Abdallah MF. Effect of Submerged vs Nonsubmerged Implant Placement Protocols on Implant Failure and Marginal Bone Loss: A Systematic Review and Meta-Analysis. Int J Prosthodont. 2018 Jan/Feb; 31(1):15-22.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Dental implants inserted in fresh extraction sockets versus healed sites: a systematic review and meta-analysis. J Dent. 2015 Jan; 43(1):16-41.
- Mello CC, Lemos CAA, Verri FR, Dos Santos DM, Goiato MC, Pellizzer EP. Immediate implant placement into fresh extraction sockets versus delayed implants into healed sockets: A systematic review and meta- analysis. Int J Oral Maxillofac Surg. 2017 Sep; 46(9):1162-1177
- Zhou W, Wang F, Monje A, Elnayef B, Huang W, Wu Y. Feasibility of Dental Implant Replacement in Failed Sites: A Systematic Review. Int J Oral Maxillofac Implants. 2016 May-Jun; 31(3):535-45
- Quaranta A, Perrotti V, Piattelli A, Piemontese M, Implants placed in sites of previously failed implants: a systematic review. Implant Dent. 2014 Jun; 23(3):311-8.
- Quaranta A1, Piemontese M, Rappelli G, Sammartino G, Procaccini M. Technical and biological complications related to crown to implant ratio: a systematic review. Implant Dent. 2014 Apr; 23(2):180-7
- Mendonca JA, Francischone CE, Senna PM, et al. A retrospective evaluation of the survival rates of splinted and non-splinted short dental implants in posterior partially edentulous jaws. J Periodontol 2014;85:787-794.
- Klinge B. Implants in relation to natural teeth. J Clin Periodontol. 1991 Jul; 18(6):482-7.
- Tsaousoglou P, Michalakis K, Kang K, Weber HP, Sculean A. The effect of rigid and non-rigid connections between implants and teeth on biological and technical complications: a systematic review and a meta-analysis. Clin Oral Implants Res. 2017 Jul; 28(7):849-863.
About the Author
 Dr. Arlin received his DDS in 1977 (McGill), his Periodontics degree in 1980 (Toronto) and his FRCD(C) in 1983. He lectures locally, internationally, and authors many articles. He founded several study clubs, is a past president of the OSP, OSCO, and was head of the CAP’s Perio course. In 1980 Dr. Arlin started his practice and has placed over 14,500 implants.
Dr. Arlin received his DDS in 1977 (McGill), his Periodontics degree in 1980 (Toronto) and his FRCD(C) in 1983. He lectures locally, internationally, and authors many articles. He founded several study clubs, is a past president of the OSP, OSCO, and was head of the CAP’s Perio course. In 1980 Dr. Arlin started his practice and has placed over 14,500 implants.
Read Part 1
Read Part 2
Read Part 3
 Read more from this issue!
Read more from this issue!
Follow the Oral Health Group on Facebook, Instagram, Twitter and LinkedIn for the latest updates on news, clinical articles, practice management and more!












