Introduction
This article is the third in a series for Oral Health magazine (August issues) that highlights the discipline of Implant Dentistry. The first article 1 of the series was published in the August 2015 issue with the title “Surgical Risk Factors in Implant Dentistry: “Effect on Failures and Bone Loss”. The second article 2 was published in the August 2016 issue with the title “Surgical Risk Factors in Implant Dentistry: Patient Related Risk Factors”. See Table 1 in this article, which outlines risk factors that are organized into four categories. The first article in August 2015 introduced these four risk factor categories, reviewed the author’s clinical private practice experience, reviewed the concept of “evidence based dentistry” and presented several clinical cases. The second article in August 2016 focused on the first of the four categories as seen in Table 1, namely “Patient related systemic risk factors”, as well as a discussion on patient informed consent, the importance of responsible diagnosis, prognosis, and treatment planning, and showed clinical cases.
This current third article of the series will focus on the second risk factor category as seen in Table 1, namely “Patient related local risk factors”, and will present some data that include the author’s private practice results, and representative cases will be shown. Future Oral Health articles in this series will cover more examples in this second risk factor category, as well additional articles on the third and fourth categories namely “Operator” and “Biomaterial” related risk factors.
Patient Related Local Risk Factors (Table 1)
This category includes but is not limited to: the patient smile type, lip support and other esthetic related considerations, dental discrepancies such as restorative space available, hard and soft tissue quality and quantity and related grafting procedures, plaque control, and excessive forces related to for example bruxism. This current article will focus on Bone Quality and Bone Quantity and the related use of Short Implants and Narrow Implants, and will show representative clinical cases.

Bone Quality and Bone Quantity
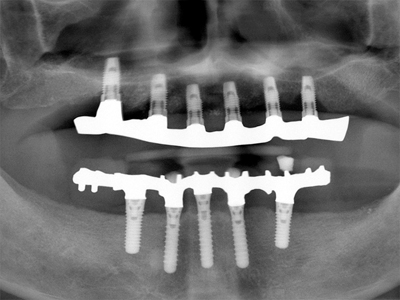
Bone quality may be the most significant risk factor for implant failure. Many studies have documented higher failure rates in poor density bone especially with the utilization of relatively smooth implant surfaces. A recent systematic review and meta-analysis3 included 19 controlled studies, 3,937 patients and 12,465 implants. Success rates were 88.8% in poor density Type IV bone compared to 96% to 97% in better bone densities. Many studies and clinical experience has shown that in the majority of cases, bone density is greater in the anterior mandible and of poorer density in the maxilla, which can result in a higher risk of implant failure and bone loss in the maxilla compared to the anterior mandible. This bone density pattern has been observed in the author’s private practice (Tables 2-4). Another example of this pattern has been experienced in the author’s private practice, where an analysis of 2,000 unsplinted implants for overdentures, showed a 3% failure rate in the mandible vs. a 9% failure rate in the maxilla (unpublished). Representative cases following this pattern are seen in Figures 1A through 1E. Implants placed in poor density bone may initially have poorer initial stability and a higher risk of early failure (Figs. 1A & 1B) or may exhibit late failure i.e. after restoration (Figs. 1C & 1D). With poor quality or quantity of bone there may be a higher risk of significant crestal bone loss (Fig. 1E). The case in Figure 1E was restored with a full maxillary arch implant supported bar-overdenture and a full mandibular arch fixed implant restoration. The long-term (over 10 years) radiographic follow up of this case demonstrated advanced crestal bone loss at the maxillary implants, while the implants placed in the anterior mandible displayed radiographic implant bone levels that had been maintained at excellent levels.

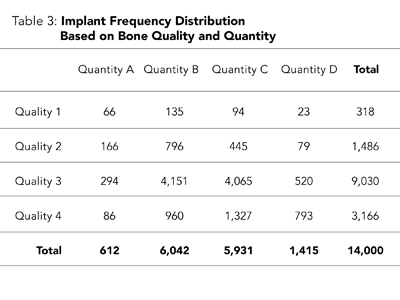

Figure 1A
Failed implant (5 mm x 13 mm) thathad poor initial stability in poor density bone.

Figure 1B
Successful delayed replacementof the failed implant as seen in Fig. 1A.
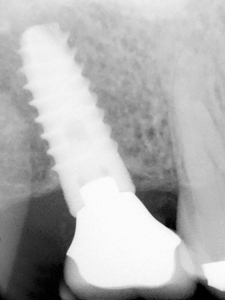
Figure 1C
6 mm length tissue level implant inrelatively poor quality and quantity bone.

Figure 1D
Failed implant from Fig. 1C, which is more frequent with poor quality and quantity of bone.

Figure 1E
Maxillary implants with advanced bone loss as compared to the mandibular implants.
Bone quantity can be deficient in the oro-facial dimension and or in the apico-coronal dimension and treatment options can include utilization of narrow and or short implants respectively and bone augmentation. Some studies have shown less predictable results with certain bone augmentation techniques 4 for example, vertical ridge augmentation. There have been additional advanced procedures that have been advocated for dealing with inadequate bone volume, such as distraction osteogenesis and inferior alveolar nerve transposition, but these have been associated with significant risks, including high levels of unpredictability and patient morbidity. On the other hand, in cases with limited bone in the apico-occlusal dimension, promising results have been reported with short implants10 (Table 5). Concerning bone deficiency in the oro-facial dimension, studies have shown that if there is residual bone thickness of less than 2 mm after the implant surgical osteotomy preparation, then there can be more bone loss, recession and lower success rates 5,6 (Figs. 2A-2D) where two cases are shown that demonstrate significant recession. This type of bone deficiency could possibly be mitigated with the appropriate use of narrower implants. The author’s private practice data as well as numerous studies 7 have shown equivalent survival rates between narrow implants and wider diameter implants. The use of short and narrow implants will be discussed in more detail later in this article (Figs. 3A-6F).

Figure 2A
Note recession at initial cementation of the full arch fixed implant prostheses.

Figure 2B
Further recession is seen at the 12-year follow up of the case as seen in Fig. 2A.

Figure 2C
Clinical appearance at the initial insertion of the splinted posterior fixed implant prostheses.

Figure 2D
At the 12-year follow up of the case seen in Figure 2C, significant tissue recession has occurred.

Figure 3A
Bone grafting was avoided by utilizing a narrow diameter implant splinted to two short implants.

Figure 3B
Clinical view of 3 implants in occlusion as seen in the radiograph from Fig. 3A.

Figure 4
Panoramic radiograph of a 17 year follow-up, where all implants when initially placed were “spinners”, were submerged, had an extended pre-loadinghealing period and were splinted.
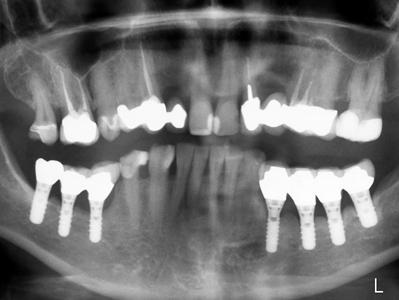
Figure 5A
Completed restoration at 2.2 with a 3.3 mm diameter implant (see Fig. 5B for the radiograph).

Figure 5B
6-year follow up of MIS titanium alloy 3.3 mm diameter implant as seen in Fig. 5A.

Figure 5C
Completed implant restoration from 3.2 to 4.2 with 3.3 mm diameter implants (see Fig. 5D).

Figure 5D
7-year follow up of MIS titanium alloy 3.3 mm diameter implants as seen in Fig. 5C.
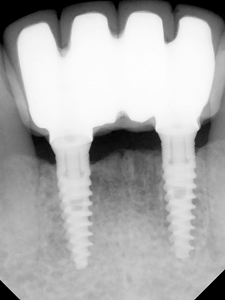
Figure 5E
Fixed bridge with a 3.3 mm diameter titanium alloy implant splinted to a 5 mm diameter implant.
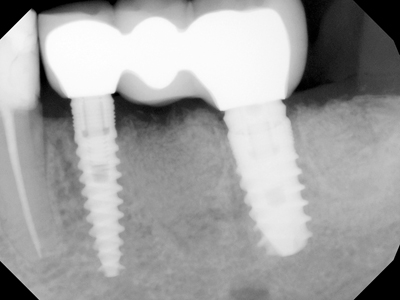
Figure 5F
Overdenture with 4 maxillary unsplinted 3.3 mm diameter MIS titanium alloy implants.
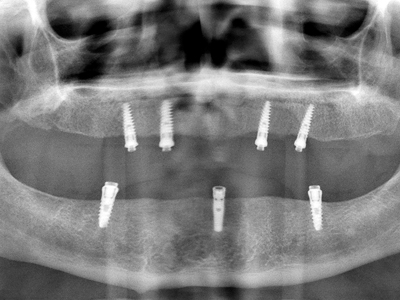
Figure 6A
Bilateral 4 unit splinted Straumann implants with 6 of 8 implants being 6 mm in length.
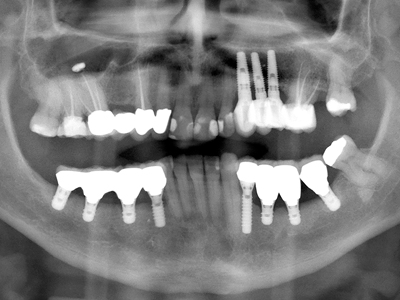
Figure 6B
Splinted Straumann 4.1 mm diameter implants with 3 of 4 being 6 mm in length.
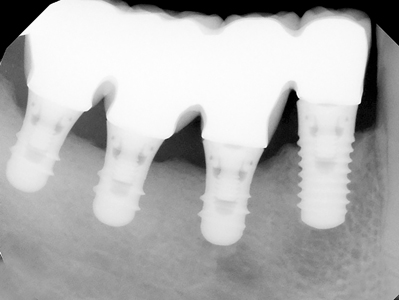
Figure 6C
Splinted Zimmer Screw-Vent 3.7 mm diameter implants, both 8 mm in length.

Figure 6D
Splinted posterior MIS titanium alloy 5.0 mm diameter implants both 8mm in length.
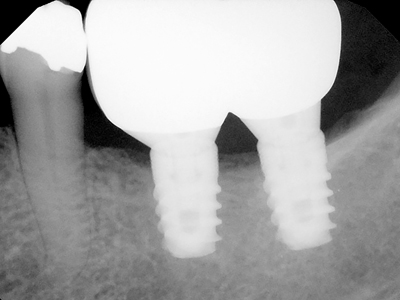
Figure 6E
Splinted posterior Straumann 4.1 mm diameter implants both 8mm in length.

Figure 6F
Single MIS titanium alloy 5.0 mm diameter implant: 6 mm in length.

The determination of bone quality and quantity should be assessed pre-surgically, primarily from radiographic analysis, and can be further assessed at the time of surgical implant placement. Implant design, size and the surgical protocol need to be modified dependant on the bone quality and quantity in order to mitigate the risk for failure. For example, when dealing with very poor bone density and quality, the surgeon may decide to undersize the osteotomy and/or use a larger implant to try to optimize initial implant stability, “submerge” the implant and give appropriate post-operative instructions in order to reduce the potential for excessive early tranmucosal loading and also include an extended healing period prior to exposure and prosthetic loading. As well, avoidance of excessive restoration forces should be incorporated into the treatment planning design, such as placing an adequate number of implants, splinting, creating a harmonious occlusion and use of a night guard. Similar clinical guidelines should be considered when confronted with limited bone quantity and utilization of narrower and or shorter implants. These approaches would be compatible with a “patient centered” approach to Implant Dentistry treatment. See Figure 4 where a case is presented with relatively short implants in poor density bone where the above guidelines were followed. In this case, the osteotomies were undersized and a submerged protocol was used because the implants attained only minimal initial stability, an extended healing time was carried out prior to second stage exposure prior to prosthetic restoration, the case was not “under engineered” i.e. a sufficient number of implants placed to try to compensate for the compromised bone quality and quantity, and excessive forces were mitigated in part by having the implants splinted in the definitive restoration.
Private Practice Data and Analysis with the “Triton DIMS” Computer Program
In this article, in addition to references to the published literature, the author will present some of his own personal private practice data. The author has documented every implant he has placed with a specialized software system called “Triton DIMS” which was described in more detail in the August 2015 article (reference #1, page 33). This software program includes documentation on the bone quality and quantity for each implant which is pertinent to this article, but the “Triton DIMS” program also has a large number of other implant related attributes. This facilitates producing a detailed analysis of a very large number of implant related attributes that can be identified as risk factors. Specifically concerning bone quality and quantity, the author at the time of surgical placement, subjectively assigns for each implant bone quality from most dense to least dense, a rating of 1,2,3 or 4 and for bone quantity from least resorption to most resorption a rating of A,B,C or D (Table 2). As well, see Table 3, which shows the author’s private practice data of the implant frequency distribution related to bone quality and quantity based on 14,000 implants with up to 28 years follow-up, and see Table 4 which documents the implant survival rates, based upon the bone quality and quantity.
Results and Statistics: Presentation Variables
Statistics can be presented as “Implant Success” or “Implant Survival” percentage rates. “Survival” only indicates the implant is still present in the mouth regardless of what complications may be associated with that implant. A designation of “Implant Success” on the other hand means the implant is not only surviving but also satisfies a defined set of criteria, such as limitations on the amount of bone loss. Another important factor is whether success or survival rates are presented as “absolute” rates or “cumulative” rates. “Absolute” rate calculations represent the successful or surviving percentage of implants at a single point in time. “Cumulative” rates on the other hand are calculated based on follow-up time period intervals, e.g. 1-2 years, 2-3 years etc., and the percentage calculation only includes those implants that been followed up for that full time period interval. See Table 4 for the summary of the “absolute survival rates” based on over 14,000 implants placed by the author that have been followed for up to 28 years, utilizing the above designations of Bone Quantity (A,B,C,D) and Bone Quality (1,2,3,4). The absolute survival rates are first presented with all implants included in each of the Quantity classifications, and then presented for each of the Quality classifications. Lastly of the 16 possible combinations of a specific Bone Quality combined with a specific Bone Quantity, the absolute survival rate for two combinations namely B3 vs. D4 are compared i.e. B3 designating good bone quality and quantity as compared to D4 designating very poor bone quality and quantity.
Quantity (Table 4)
Consider Quality D at 90.1% as compared to 94.3% to 95.3% for the better bone qualities A, B and C. These same numbers equate to about double the failure rates i.e. 9.9% for Quality D vs 4.7% to 5.7% failure rates with the better bone qualities A, B and C.
Considering bone quantity alone, the survival rate was somewhat lower only for the poorest quantity i.e. Quantity 4 at 92.3% as compared to 94.3% to 95.5% for the better bone quantities 1, 2 and 3. These same numbers equate to about 50% higher failure rates i.e. 7.7% for Quantity D vs 4.5% to 5.7% failure rates with the better bone quantities.
Considering bone quantity and quality combined, the survival rate was significantly lower for the poorest bone quality and quantity combination i.e. D4 at 89.1% as compared to 95.4% for B3 i.e. a good bone quality and quantity combination. These same numbers equate to about double the failure rate i.e. 10.9% for D4 vs 4.6% for B3.
Clinical Utilization of Short and Narrow Implants
When the clinical situation presents with less than the ideal amount of bone quantity, the dentist needs to review all reasonable options with the patient. These would include but are not necessarily limited to: no treatment, bone augmentation, use of short or narrow diameter implants. The informed consent process includes taking into account the available evidence, clinical judgement and what is indicated for the specific needs of the patient. This portion of this article will focus on some of the results, indications and contraindications for the use of narrow diameter and short implants, and show some cases (Figs. 5A-6F).
Narrow Implants
Utilization of narrow implants can be successful if appropriate guidelines are adhered to (Figs. 5A-5F) and there are many publications attesting to their successful incorporation. In particular, a 2017 publication 7 was a systematic review and meta-analysis on narrow implants that found narrow implants performed as well as wider implants. As well, the author has found that a variety of narrow diameter implants have performed as well as the wider diameter implants in his private practice (unpublished). The design and diameter of what is generally considered to be standard two-piece narrow diameter implant would be in the 3.0 mm to 3.5 mm range. Some clinicians advocate the use of implants narrower than 3 mm; most of these are one-piece designs and are usually referred to as “mini-implants”. Good quality studies on mini implants are limited but some publications have shown promising results, especially for the survival rates of mini-implants in the mandible. The author has placed over 150 mini-implants with survival rates well over 90% but is not within the scope of this article to report on this topic in further detail. For the purposes of this article and the cases presented, narrow diameter implants will refer to two-piece implants in the 3.0 to 3.5 mm range.
Indications for Narrow Diameter Implants
The patient informed consent process has been carried out
• Bone availability is insufficient in the oro-facial dimension to ideally allow 1 mm (and preferably 2 mm on the facial) of residual bone after the implant osteotomy
• Bone augmentation to ideal width is not selected by the patient and the clinician
• There is a reasonable expectation of success
• The selected implant and case design will be of sufficient biomechanical strength
• The functional and or esthetic result will be satisfactory
Contra-Indications for Narrow Diameter Implants
• A wider diameter implant can “easily” be accommodated
• The selected implant and case design will NOT be of sufficient biomechanical strength
• The functional or esthetic result will NOT be satisfactory
Short Implants
Results: Utilization of short implants can be successful if appropriate guidelines are adhered to (Figs. 6A-6F) and there are many publications attesting to their successful incorporation. While there have been many studies indicating equivalent survival rates between normal and short implants, two recent systematic reviews and Meta-Analysis 8,9 did find somewhat lower survival rates with very short implants i.e. shorter than 8 mm. The author of this current article has published on the Straumann tissue level implants comparing the survival of 6, 8, 10 and 16 mm lengths 10 and has documented longer term follow-ups as seen in Table 5.
Author’s Experience of Survival rates with 6 mm to 16 mm length implants (Table 5)
The author has utilized multiple implant systems, however, in this article for the purposes of minimizing confounding variables in comparing different implant systems and designs, only the Straumann system tissue level design is presented. Specifically, the survival rates of short implants compared to longer length implants are presented at four different follow-up time periods (Table 5).
Discussion of Survival Rates for Short Implants (Table 5):
The 8 mm length implants were similar to the 10 to 16 mm length implants at all time intervals. The 6 mm short implants at all time intervals displayed over 90% survival rates but were 3% to 5% below the survival rates for 8 mm and 10-16 mm length implants, representing about 100% higher risk of failure rate for the 6 mm lengths. Nevertheless with over 90% of 6 mm length implants surviving after up to a 20-year follow up, the utilization of 6 mm length implants may be worth considering in certain cases. The treating dentist must utilize evidence based concepts to reach such a conclusion, which would of course include patient informed consent and notably informing the patient of the higher potential risk for failure of these 6 mm length implants compared to longer implants. As mentioned previously, this would be consistent with a “patient centered” approach. Of significance is that the Straumann system switched from a TPS coated surface to an SLA surface several years ago and the author’s above analysis did combine these two surfaces. The breakdown of the older TPS surface implants vs the newer SLA surface implants was not analyzed in this article. However, this breakdown was done previously i.e. the performance of these two different surfaces were investigated and published11 and the results did indicate a significant reduction in the crestal bone loss and failure rate with the SLA surface compared to the older TPS surface. In the current data base, about 20% were TPS implants. If only the SLA implants were to be presented, the author estimates that the survival rates would be approximately 1% higher than those presented in Table 5.
Clinical Considerations for Short Implants
The vast majority of 6 mm length implants were placed in the posterior mandible where one could postulate that the bone quality and survival rates would be higher as compared to implants placed in the posterior maxilla. A sufficient number of short implants were placed such that the cases were not “under engineered” i.e. often a 1:1 implant to tooth ratio was utilized where possible. Clinical guidelines were also taken to reduce the risk of biomechanical overloading. When multiple adjacent implants were placed, they were usually splinted. Cantilevers and balancing side contacts were avoided if possible and a harmonious occlusion was established and maintained over time. Night guards were also recommended.
Indications for Short Implants
• The patient informed consent process has been carried out
• Bone augmentation, distraction osteogenesis and inferior alveolar nerve transposition have not been chosen by the dentist and the patient
• There is a reasonable expectation of success
• The selected implant and case design will be of sufficient biomechanical strength
• The functional and or esthetic result will be satisfactory
Contra-Indications for Short Implants
• A longer implant can “easily” be accommodated
• The selected implant and case design will NOT be of sufficient biomechanical strength
• The functional and or esthetic result will NOT be satisfactory
• The selected implant will have too high a risk of damage to the inferior alveolar nerve
Summary
The first two articles in this Oral Health magazine August series (2015 and 2016) introduced risk factors in implant dentistry, and covered several important concepts and focused on patient related systemic risk factors. This third article focused on bone quality, bone quantity and the related use of narrow and short implants. In addition to references to the published literature, this article included the author’s personal private practice results representing a database of 14,000 implants that have been followed and documented on a specialized software program (Triton DIMS) for up to 28 years. The consensus in the published literature and the author’s private practice results are consistent. Specifically the author’s results indicated that failure rates in poor bone quality can be over 100% higher compared to good bone, and a 50% higher failure rate in moderately poor quantity bone compared to good bone. On the other hand narrow implants have survival rates comparable to wider implants and have had a wide range of clinical applications. Short implants can demonstrate reasonably good results with proper case selection and design. For example, the author’s private practice results have shown that the “judicious” use of very short implants of 6 mm length demonstrated over 90% survival for up to 20 years of follow up and 8 mm length implants had equivalent survival rates compared to implant lengths in the 10 to 16 mm range. Future articles in this series will cover risk factors in the other categories as outlined in Table 1 including more “patient related local risk factors” as well as “operator” and “biomaterial related risk factors”.
Oral Health welcomes this original article.
References:
- Arlin, M.L. “Surgical risk factors in Implant dentistry: Effect on failures and bone loss”, Oral Health, August 2015, pages 32-38
- Arlin, M.L. “Risk factors in implant dentistry: Patient related risk factors”, Oral Health, August 2016, pages 26-36
- Goiato MC, Santiago JF, Moreno A, Pellizer EP. “Longevity of dental implants in type IV bone: A systematic review”, in Int J Oral Maxilofac Surg, 2014 June;43 (6): 747-57
- Tepper G, Hass R, Zecher W, Watzek G. “Three dimensional finite element analysis of implant stability in the atrophic posterior maxilla: A mathematical study of the sinus floor augmentation”, in Clin Oral Impls Res 2002 Dec: 13 (6): 657-5
- Spray JR, Black CG, Morris HF, Ochi S. “The influence of bone thickness on facial marginal bone response: Stage 1 placement through stage 2 uncovering”, in Ann Periodontol. 2000 Dec; 5(1): 119-28
- Qahash M, Susin C, Polimeni G, Hall J, Wikesj, M, “Bone healing dynamics at buccal peri-implant sites”, in Clin Oral Implants Res. 2008 Feb; 19(2): 166-72
- Klein MO, Schregnitz E, Al-Nawas B, “Systematic review on success of narrow-diameter implants”, in Int. J. Oral Maxillofac Implants 2014,29 suppl:43-54
- Lemos CA, Ferro-Alves ML, Okamoto R, Mendonca MR, Pellizzer EP, “Short implants versus standard implants placed in the posterior jaws: A systematic review and meta-analysis”, in J. Dent. 2016, Apr; 47:8-17
- Stafford GL. “Short implants had lower survival rates in posterior jaws compared to standard implants”, in Evid based Dent. 2016, Dec; 17(4): 115-116
- Arlin ML. “Short dental implants as a treatment option: results from an observational study in a single private practice”. Int J of Oral Maxiliofac Implants 2006; 21 (5): 769-776
- Arlin ML. “Survival and success of sandblasted, large grit acid etched and titanium plasma sprayed implants: A retrospective study”. J. Can Dent Assoc. 2007;73 (9): 821a-821f
About the Author
 Dr. Murray Arlin received his D.D.S. at McGill University, Montreal, his Diploma in Periodontics at the University of Toronto and his Fellowship in the Royal College of Dentists of Canada. Dr. Arlin has numerous publications in the fields of Periodontics and Implant Dentistry, and has lectured internationally on Periodontics and Implant Dentistry. He maintains a full-time Periodontics and Implant Dentistry practice in Toronto, Ontario.
Dr. Murray Arlin received his D.D.S. at McGill University, Montreal, his Diploma in Periodontics at the University of Toronto and his Fellowship in the Royal College of Dentists of Canada. Dr. Arlin has numerous publications in the fields of Periodontics and Implant Dentistry, and has lectured internationally on Periodontics and Implant Dentistry. He maintains a full-time Periodontics and Implant Dentistry practice in Toronto, Ontario.












