Implant treatment complications related to both screw and cement-retained installation systems appear to be similar and troubling. Peri-implant disease treatments can be uncomfortable, expensive, and unpredictable.1,2 Intra-oral cementation can consistently optimize the fit of implant parts and reduce cantilevers to improve access to care,3,4 but has been plagued by complications related to residual subgingival cement and open margins.5-7 An intra-oral cementation system that mitigates these peri-implant risk factors can reduce installation-related complications, making treatment safer for patients.4,8
This article compares single crown installation utilizing Chamfer Margin (CMS) and Reverse Margin (RMS) Systems to determine their relative efficacy at averting subgingival cement and open margins.
A previous publication measured the effect of installation pressure on generating subgingival cement.9 Crowns, complimentary abutment retainers and models were designed on 3Shape (New Providence NJ) software and printed. (Figs. 1-3) Lifelike gingiva was mastered to fit the retainer profile. Crowns margins were placed subgingivally as follows: Lingual (L) ½ mm; Buccal (B) 1 mm; Mesial (M) and Distal (D) ½-1 mm. (Figs. 4,5)
Fig. 1
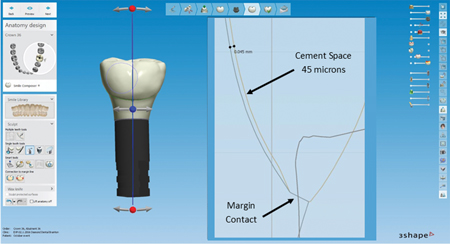
Fig. 2

Fig. 3

Fig. 4

Fig. 5

For installation, each crown was half-filled with directly dispensed Rely-X Unicem cement (3M, London ON) and then pushed into place onto its abutment retainer. The crown systems trials were alternated to control for operator inconsistencies. Crowns were pressed into place over 5 seconds to reach the desired pressure and held for 5 more seconds before the cement was polymerized with an Elipar Deepcure S light (3M Espe, London ON)). (Fig. 6)
Fig. 6

Photographs against a millimeter grid were taken of the B, M, L and D aspects of each abutment-crown interface. The images were copied into a Windows Publisher program (www.Windows.com) and enlarged to facilitate the measurement process. (Figs. 7,8) Differences between groups were tested (p≤0.05) using the Mann-Whitney U test.
Fig. 7

Fig. 8

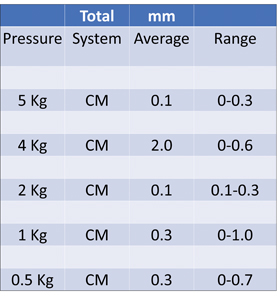
The extent of cement travel beyond the abutment margins was measured on each margin face. Table 1 shows the range and average of submarginal cement under each pressure condition tested.
For open margin measurements, excess cement covering the marginal interface was removed and measurements in the center of each margin face were taken. (Fig. 9) No open margins were observed when gingiva had been removed and the crowns were installed onto abutments with or without cement. (Fig. 10)
Fig. 9

Fig. 10

Results:
1) Effects of System Design and Installation Pressure on Submarginal Cement
Table 1 indicates the sum of cement travel past B, M, L & D abutment margins. Ten trials were completed for each pressure condition. The RMS prevented cement from breaching the abutment margin better than the CMS at every pressure tested. Unlike the CMS, the RMS eliminated cement breach at 2Kg or less cementation pressure. (Table 1)
Table 1

2) Effects of System Design and Installation Pressure on Open Margins
None of the RMS trials had any vertical openings between margins, while all the CMS trials had open margins at all installation pressures. (Table 2, Fig. 11)
Fig. 11
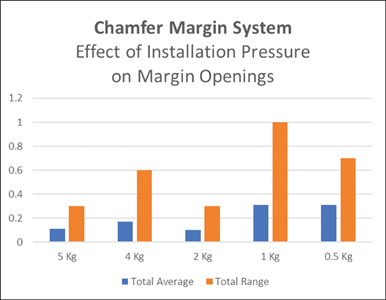
Table 2
3) Effects of System Design, Installation Pressure and Margin Depth on Open Margins
All the CMS trials had vertical interface spaces that increased with deeper margins and decreasing installation pressure. None of the RMS trials had any vertical openings between margins. There was a difference between RMS and CMS at all pressures and margin depths tested. (Table 3, Figs. 12,13)
Table 3

Fig. 12

Fig. 13

Discussion: Unlike the CMS, the RMS was designed to be sensitive to, and to mitigate the root causes of complications as described in Comparing the Chamfer and Reverse Margin Systems at Preventing Submarginal Cement while varying Crown Installation Pressure and Margin Depth., Svoboda, Sharma and Zakari, 2020.9 The RMS offers dentists a safe technique for using a low-pressure cementation system that protects patients from misfit implant parts, subgingival cement and open margins, that are recognized risk factors for complications including peri-implant disease.1,5,7
Previous publications have introduced new terminology to facilitate discussion and mitigation of peri-implant complications related to prevalent prosthesis installation systems.8 In addition to preventing subgingival cement and open margins, it is now possible to consistently optimize the fit of implant parts, reduce prosthesis width profiles for better access, and to segment the final prosthesis to reduce the impact of implant failure.10
Extrapolating from the studies of Lee1, Jepsen2, Wilson5 and Heitz,7 the impact of preventing the above risk factors is significant. The challenges of subgingival cement and open/overhanging margins are well-established in clinical dentistry. Misfit implant parts related to the screw-in installation technique are similarly problematic.10 According to Analysis of 15,000 Dental Implants placed over a 30-year period, Arlin, 2020,11 there was no difference in survival rates between the first 10-year group and the last 20-year group.
No discernable improvement in implant survival rates over 30 years should be a concern to the profession. Was it a lack of attention to common risk factors for complications? Or did the dental industry simply exchange one group of risk factors for another? It is clearly unacceptable that up to 81% of implant patients should suffer peri-implant disease.1
Once the overriding risk factors for complications directly related to implant prosthesis installation7 are eliminated or at least minimized, it will facilitate analyzing the differences between screw-in and cement-in techniques. This may foster the development of even more ways to improve treatment results benefitting both patients and dentists.
Conclusions:
- The RMS consistently outperformed the CMS in preventing subgingival cement under all conditions.
- The RMS eliminated both submarginal cement and open margins under low-pressure crown installation conditions. The CMS did not.
- The results of this study support the concepts of the root causes of complications.8
- More clinical studies are needed to further evaluate the efficacy of the RMS at improving patient outcomes.
Oral Health welcomes this original article.
References
- Lee CT, Huang YW, Zhu L, Weltman R. Prevalence of peri-implantitis and peri-implant mucositis: systematic review and meta-analysis. J Dent 2017;62:1-12.
- Jepsen S et al. Primary Prevention of peri-implantitis: Managing peri-implant mucositis. J Clin Periodontol 2015;42 (Suppl. 16): S152-158.
- Svoboda ELA. Fixed Prosthesis Installation: An Aviation Analogy Considering 3-D Position, Yaw, Pitch and Roll. www.ReverseMargin.com/articles: Oct 2021:1-5.
- Svoboda ELA. Screw versus Cement Debate: Will that be Peri-implant Disease by Misfits and Poor Access to Care or Bad Margins and Subgingival Cement? 2021 Spectrum Implants V12 N4: 38-47.
- Wilson TG Jr. The Positive Relationship Between Excess Cement and Peri-implant Disease: A Prospective Clinical Endoscopic Study.
J. Periodont 2009:1388-1392. - Linkeviˆcius T, Vindasiute E, Puisys A, Peciuliene V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin Oral Impl Res 2011;1379-1384.
- Heitz-Mayfield LJA, Heitz F, Lang NP. Implant Disease Risk Assessment IDRA – a tool for preventing peri-implant disease. Clin Oral Impl Res. 2020; 31:397-403.
- Svoboda ELA. New Dental Implant Terminology for Exposing and Mitigating the Root Causes of Installation-Related Treatment Complications. Spectrum Implants Mar/Apr 2021; Vol.12, No. 2: 28- 43.
- Svoboda ELA, Sharma A, Zakari M. Comparing the Chamfer and Reverse Margin Systems at Preventing Submarginal Cement while varying Crown Installation Pressure and Margin Depth. www.ReverseMargin.com/articles: 2020; 1-13.
- Svoboda ELA. Chamfer Margin Showdown, Bringing a New Standard of Care to Town. www.ReverseMargin.com/articles; 2021: Video Webinar.
- Arlin M. Analysis of 15,000 Dental Implants placed over a 30 year period. Spectrum Implants: Special Issue Dec 2020; 8-62.
About the Author
 Emil L.A. Svoboda graduated from the University of Toronto with a PhD, DDS. He is a Fellow of the AGD, an Honored Fellow of the AAID and a Diplomate of the ABOI/ID. He has received the Award of Merit from the ODA for his contributions to organized dentistry. He practices Implant Dentistry at ParkPlace Dental Centre in Brampton, Ontario. Dr. Svoboda has been granted Patents for his innovative Reverse Margin System designs. He is thankful to Diamond Dental Studio, Dental Laboratory and Design Centre for making Reverse Margin System products and the Aurum Group® of Dental Laboratories and Core3D Milling Centres North America for helping to make Reverse Margin System products available to dentists across North America. Dr. Svoboda lectures Nationally and Internationally and wants to make implant treatment better.
Emil L.A. Svoboda graduated from the University of Toronto with a PhD, DDS. He is a Fellow of the AGD, an Honored Fellow of the AAID and a Diplomate of the ABOI/ID. He has received the Award of Merit from the ODA for his contributions to organized dentistry. He practices Implant Dentistry at ParkPlace Dental Centre in Brampton, Ontario. Dr. Svoboda has been granted Patents for his innovative Reverse Margin System designs. He is thankful to Diamond Dental Studio, Dental Laboratory and Design Centre for making Reverse Margin System products and the Aurum Group® of Dental Laboratories and Core3D Milling Centres North America for helping to make Reverse Margin System products available to dentists across North America. Dr. Svoboda lectures Nationally and Internationally and wants to make implant treatment better.
 Anit Sharma is an Associate Fellow of the AAID and practices implant dentistry with Dr. Svoboda.
Anit Sharma is an Associate Fellow of the AAID and practices implant dentistry with Dr. Svoboda.
 Dr. Darminder Cheema practices General Dentistry at ParkPlace Dental Centre. Drs. Sharma and Cheema have no financial interests in the RMS. They have actively participated in this research project. Thanks to Marina Tereshchenko RDT of Diamond Dental Studio for creating the models, abutments and crowns used in this study.
Dr. Darminder Cheema practices General Dentistry at ParkPlace Dental Centre. Drs. Sharma and Cheema have no financial interests in the RMS. They have actively participated in this research project. Thanks to Marina Tereshchenko RDT of Diamond Dental Studio for creating the models, abutments and crowns used in this study.












