Dental caries is one of the most prevalent diseases affecting humans. Unfortunately, we do not yet have a grip on! 1 Over the years, researchers have actively looked for methods for treating and arresting decay other than traditional restorative options. Silver nitrate has been used for more a thousand years. G.V. Black, a founding father of modern dentistry, described protocols for arresting dental caries with silver nitrate in the late 1800s. 2 Silver fluoride (AgF) has been used in Japan for approximately 900 years; it prevents dental caries by cosmetically blackening the dentition. Silver and fluoride, in combination, have been used and studied extensively for efficacy in caries prevention and management. 2 More recently, ammonia (NH3+) was added to this formulation; it is now known as silver diamine fluoride (SDF). 3 Originally approved in Japan, it has been available in Australia, Brazil, Argentina, Mexico and China since the 1980’s. As a result, most studies were done in these countries, published in languages other than English. Recently, SDF was approved for use in the Canada and United States.
The U.S. Food and Drug Administration (FDA) cleared the new formulation of 38% SDF in 2014. It is currently available as Advantage Arrest (Elevate Oral Care) in a cavity varnish format. The indications include SDF’s ability to arrest and prevent dental caries and treatment of dentine hypersensitivity. Until late 2016, its use in the United States as a caries preventing or arresting agent was off-label. In October 2016, the FDA announced that they had granted Breakthrough Designation Therapy to 38% SDF Advantage Arrest (Fig. 1) as a product able to arrest and prevent tooth decay in children and adults.
Fig. 1
Advantage Arrest™.

In Canada, Advantage Arrest is distributed exclusively by Oral Science. It received approval from Health Canada in February 2017. In Canada, 38% Advantage Arrest liquid is recognized to have anti-caries properties that prevent, fight and/or protect against dental caries, as well as being an effective fluoride agent that helps to reverse the tooth decay process at the earliest stages before it can develop to a cavity. 5
Systematic reviews of clinical trials in children and older adults provide evidence of the effectiveness of SDF in arresting coronal and root caries. 2,4,6-9 A systematic review examining clinical trials using SDF to arrest dental caries among children reported an overall percentage of 81% of active caries being arrested (95% CI, 68% to 89%; p<0.001) when a concentration of 38% SDF was used. 4 Furthermore, a retrospective study found that an annual application of 38% SDF was more effective in hardening and arresting dentinal caries in the upper anterior primary teeth than the application of 5% NaF varnish at three month intervals. 6,10 Another literature review examined randomized clinical trials; it demonstrated caries arrest after the topical application of 38% SDF, and indicated better results when the SDF was applied twice yearly over a period of two years. 11 Additional studies are needed to determine the long-term effectiveness of single and multiple applications of SDF over a period of more than two to three years, particularly if the SDF treatment is discontinued.
What is silver diamine fluoride?
SDF is a colorless topical liquid with 25% (w/v) silver, 8% ammonia and 5% sodium fluoride. 3 SDF has been shown to be effective in preventing and arresting dental caries, and treating pain associated with dentin hypersensitivity. 2,4,6-9,12,13
How does SDF work as a caries arresting agent?
The silver acts as an anti-microbial that limits the reinvasion of cariogenic biofilm, including Streptococcus mutans 14, the sodium fluoride promotes remineralization 15 and inhibits growth of the cariogenic biofilm, and the ammonia acts as the solvent that stabilizes the high concentrations in the solution. 2 SDF applied to a carious lesion reacts with both the protein (collagen) in the dentin and the hydroxyapatite. 16 SDF deposits a layer of silver protein that resists acids produced by cariogenic bacteria, and furthermore, produces calcium fluoride that acts as a reservoir for fluoride by neutralizing the imbalance between demineralization and remineralization. Hydroxyapatite and fluorapatite form on the treated tooth surface, along with silver chloride and metallic silver. 16 The end-result is a harder tooth surface, arresting the caries process, with the decayed area stained brown or black. 6 An in-vitro study showed that SDF had a higher inhibitory effect on both dentin demineralization and collagen degradation when compared to sodium fluoride and silver nitrate alone, which can explain its success in arresting dental caries in clinical trials. 16
How does SDF work as a desensitizing agent?
The application of 38% SDF on exposed and painful dentinal tubules forms silver ion salts that occlude and block the dentinal tubules. As an added benefit of sodium fluoride, it effectively treats any pain related to dentinal hypersensitivity without staining the treated area. 12,13
Who can benefit from SDF?
SDF is indicated for:
1. Patients at high risk for dental caries
2. Patients with numerous carious lesions that cannot be treated in a single visit
3. Lesions that are too difficult to treat in a single visit
4. Patients who are behaviourally or medically-challenged
5. Patients without access to proper dental care
6. Young children waiting for hospital-based dental treatments
7. Non-invasive treatment of deciduous teeth about to exfoliate
8. Patients reporting pain from dentine hypersensitivity 11
SDF can be a treatment option for a myriad of patients.
What are the advantages of using SDF?
It is a non-invasive, cost-efficient, fast, and effective method for controlling the infection, with no need for cavity preparation and/or administration of local anesthetic. 17 The simple paint-on application does not require extensive training for dentists or dental hygienists. SDF is ideal for treating young children and dental emergencies. 6,17
Are there any contraindications or adverse reactions?
The only documented contraindication to using SDF is an allergy to silver or heavy metal ions. The presence of severe soft tissue or mucosal ulceration or inflammation is considered a relative contraindication. 17 Furthermore, like many other products, it has not been tested on pregnant or lactating women. Adverse reactions to SDF are rare. If SDF contacts soft tissues, a temporary gingival whiteness or redness may appear. 17 It is thus critical to have proper isolation of the treatment area, and to assure that the microbrush is not oversaturated with liquid during the application. Careful handling of the liquid is important; it can stain clothing, leather, countertops, and other hard surfaces. The only drawback in using SDF on carious lesions is that the treated area will be stained black-brown permanently. Patients or parents of children may not be pleased with the esthetics following the use of SDF, 11,17 and this should be explained beforehand.
What is the maximum safe dosage?
A 2012 study suggested that serum concentrations of both fluoride and silver after the application of SDF were well below the concentrations associated with toxicity in adults. 18 Other safety studies are reflected in the manufacturer’s maximum dosage guidelines for a safe application of SDF that suggest that dosage should be based on the weight of the patient. It is recommended to limit the dosage to 1 drop of 38% SDF per 10 kg of body weight per treatment visit. 2 Case studies have shown that 1 drop of liquid can be used to treat up to five teeth. 11
What is the suggested treatment protocol?11
When applying SDF for either arresting dental caries or treating dentinal hypersensitivity, it is imperative to use caution and to obtain proper patient consent. Patients with a known allergy to silver or any other ingredients found in the product should not be treated with SDF. Patients must be made aware that in the presence of decayed dentin, the treated area will stain dark (black-brown), harden over the course of the first week, as the depth of the carious lesion decreases. 16 It is important to mention that the resulting black staining will not fade away with time. SDF may also stain the surrounding soft tissue temporarily; it cannot be washed away and will disappear on its own within one to three weeks with no harm to the patient. SDF should not be applied in presence of soft tissue inflammation, injury, or close to a surgical site. Multiple applications may be needed to ensure the caries process is completely arrested or all dentinal tubules are obliterated. Based on findings from systematic reviews, Horst et al. recommends an application of 38% SDF twice a year to carious lesions for the first two years with proper documentation and follow-up appointments. 11
When applying SDF, protect the soft tissue and gingiva adjacent to the treatment site with petroleum jelly and isolate the area with cotton rolls or gauze. Dry the surface, and apply sparing amounts of the liquid using a microbrush. Allow the SDF to penetrate the tooth structure for at least one minute. Then remove any excess with gauze or a cotton roll. Rinse the area with water to minimize the metallic taste in the patient’s mouth. No special post-care instructions are needed. 11,19
After the carious lesion is arrested, a temporary (standard glass ionomer cement) or final restoration may be placed 11 (Figs. 2-5).
Fig. 2
Before and after application of silver diamine fluoride. Courtesy of Dr. John Frachella.
BEFORE
AFTER
Fig. 3
Silver diamine fluoride and application of composite to reduce staining. Courtesy of Dr. Josh Wren.
BEFORE
DURING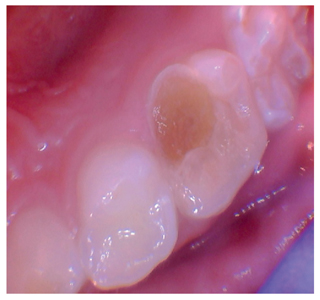
AFTER
Fig. 4
Silver diamine fluoride and application of self-curing glass ionomer to restore the tooth and reduce staining. Courtesy of Dr. Josh Wren.

Fig. 5
Typical stains. Courtesy of Dr. Jeremy Horst.

Conclusion
Silver diamine fluoride has the potential to play a very important role in minimally invasive dentistry for patients of all ages. It can also be a treatment incorporated into preventive community oral health programs as an adjunct to fluoride varnish and dental sealant programs for caries management. From a public health perspective, the use of 38% SDF is an interesting option for treating patients with barriers to dental care because it is a safe, effective, non-invasive, efficient, and economical treatment option to control and arrest carious lesions. Furthermore, it can potentially increase access to care, improve oral health and reduce the need for emergency dental care. It is a powerful treatment option to finally win the fight against dental caries for our clientele that is most at risk! OH
Oral Health welcomes this original article.
Disclosure
Sylvie Martel is an independent dental hygienist consultant and key opinion leader for a number of leading dental corporations and has received financial compensation from Oral Science for writing this article.
References
1. WHO–What is the burden of oral disease? http://www.who.int/oral_health/disease_burden/global/en/ (accessed 04 May, 2017).
2. Rosenblatt A, Stamford TC, Niederman R. Silver diamine fluoride: A caries “Silver-fluoride bullet”. J Dent Res 2009;88(2):116-126.
3. Mei ML, Chu CH, Lo ECM, Samaranayake LP. Fluoride and silver concentrations of silver diammine fluoride solutions for dental use. Int J Paeditr Dent. 2013;23:279-285.
4. Gao SS, Zhao IS, Hiraishi N, Duangthip D, Mei ML, Lo EC, Chu CH. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clinical and Translational Research 2016; 1(3):201-210.
5. Health Canada (2017). Natural Health Products Database: Advantage Arrest–38% Silver diamine fluoride, Elevate Oral Care. NPN #80075746. https://health-products.canada.ca/lnhpd-bdpsnh/info.do?licence=80075746 (accessed 04 May, 2017).
6. Chu CH, Lo EC. Promoting caries arrest in children with silver diamine fluoride: a review. Oral Health Prev. Dent 2008;6(4):315-321.
7. Li R, Lo ECM, Liu BY, Wong MCM, Chu CH. Randomized clinical trial on arresting dental root caries through silver diamine fluoride applications in community-dwelling elders. J Dent 2016;51:15-20.
8. Tan HP, Lo ECM, Dyson JE, Luo Y, Corbet EF. A randomized trial on root caries prevention in elders. J Dent Res. 2010;89(10):1086–1090.
9. Zhang W, McGrath C, Lo ECM, Li JY. Silver diamine fluoride and education to prevent and arrest root caries among community- dwelling elders. Caries Res. 2013;47(4):284–290.
10. Marinho VC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2013;7:CD002279.
11. Horst JA, Ellenikiotis H, Milgrom P. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications, and consent. J Calif Dent Assoc. 2016;44:16-28.
12. Castillo JL, Rivera S, Aparicio T, Lazo R, Aw TC, Mancl LL, Milgrom P. The sort-term effects of diammine silver fluoride on tooth sensitivity: a randomized controlled trial. J Dent Res. 2011;90(2)203-208.
13. Craig GC, Knight GM, McIntyre JM. Clinical evaluation of diamine silver fluoride/potassium iodide as a dentine desensitizing agent: a pilot study. Aust Dent J. 2012;57(3):308-311.
14. Knight GM, McIntyre JM, Craig GG, Mulyani, Zilm PS, Gully NJ. Inability to form a biofilm of Streptococcus mutans on silver fluoride- and potassium iodide-treated demineralized dentine. Quintessence Int. 2009;40(2):155-161.
15. Gao SS, Zhang S, Mei ML, Lo EC, Chu CH. Caries remineralisation and arresting effect in children by professionally applied fluoride treatment – a systematic review. BMC Oral Health 2016. Feb 1;16(1):12.
16. Mei ML, Ito L, Cao Y, Li QL, Lo ECM, Chu CH. Inhibitory effect of silver diamine fluoride on dentine demineralisation and collagen degradation. J Dent 2013;41:809-817.
17. Mei ML, Lo ECM, Chu CH. Clinical use of silver diamine fluoride in dental treatment. Compend Continu Educa Dent. 2016; 37(2):93- 98.
18. Vasquez E, Zegarra G, Chirinos E, et al. Short term serum pharmacokinetics of diammine silver fluoride after oral application. BMC Oral Health 2012;12:60.
19. Safety Data Sheet – Advantage Arrest Silver Diamine Fluoride 38% http://www.elevateoralcare.com/site/images/AASDS082415.pdf (accessed 04 May, 2017).
About the Author
 Sylvie Martel is an international speaker, entrepreneur and educator. She works in close collaboration with the corporate sector as a lecturer, key opinion leader, trainer, writer and education specialist. She is the dental hygiene advisor for the National Dental Hygiene Certification Board of Canada, and is on the Commission on Dental Accreditation of Canada Board. She works as a consultant for certain dental hygiene regulatory bodies in Canada.
Sylvie Martel is an international speaker, entrepreneur and educator. She works in close collaboration with the corporate sector as a lecturer, key opinion leader, trainer, writer and education specialist. She is the dental hygiene advisor for the National Dental Hygiene Certification Board of Canada, and is on the Commission on Dental Accreditation of Canada Board. She works as a consultant for certain dental hygiene regulatory bodies in Canada.












