Abstract
Inadvertent displacement of teeth or fragments of teeth beyond the tooth socket during extraction is an uncommon occurrence. In this paper, we present two cases of displacement of impacted third molars, one maxillary and one mandibular. We outline our removal technique as well as some general management considerations, should this situation arise. Most importantly procedures and processes to prevent this complication of dental extraction will be discussed.
Displaced teeth during the routine extraction of impacted third molars is a rare but potentially serious complication. 1 Displacement of maxillary third molars can occur into the maxillary sinus, buccal space or infratemporal fossa and displacement of mandibular third molars can occur into the sublingual, submandibular, pterygomandibular or lateral pharyngeal spaces. 1,2,3,5 Although not common, this is a well-recognized complication that can cause increased morbidity and undue stress for both the patient and the practitioner. 5 Numerous retrieval techniques have been described ranging from direct exposure/access using intra and/or extra-oral approaches, fluoroscopy with triangulation, endoscopic retrieval and even CT guided intra-operative navigation or some combination of these techniques. 1,4,5,6
We report two cases of displaced third molar teeth and our protocol for their retrieval. In addition to this we provide recommendations to the general practitioner for how to avoid this complication as well as what to do should this unfortunate occurrence arise.
Case 1
A 16-year-old patient was undergoing the routine extraction of four impacted third molar teeth at a general practitioner’s office when tooth #1-8 was accidentally displaced superiorly and imaging at the time of surgery suggested displacement into the maxillary sinus. After an attempt at locating and retrieving the tooth by the general dentist, the patient was placed on Amoxicillin and then referred to our Oral and Maxillofacial Surgical program at London Health Sciences Center (LHSC). On examination, the patient had mild swelling and trismus to 30 mm. An oroantral communication with buccal fat herniation was also noted at site #1-8. The tooth was unable to be visualized on examination. A panorex obtained in the dental office was sent with the patient (Fig. 1); however, it was unclear from the panorex and clinical exam, whether the tooth was displaced into the infratemporal fossa or maxillary antrum. A CT was then ordered revealing the displacement of tooth #1-8 into the right maxillary sinus (Figs. 2 & 3).
Fig. 1
A Panorex from the referring dentist of the patient in case one demonstrating superior displacement of tooth #1-8.

Fig. 2
A coronal (left) and sagittal (right) section of a CT obtained of the patient demonstrating displacement of tooth #1-8 into the right maxillary sinus.

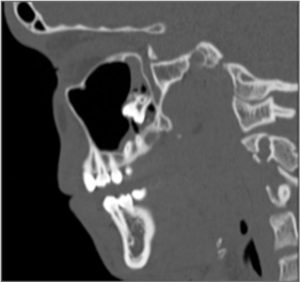
Fig. 3
An axial section of a CT of the patient demonstrating the position of tooth #1-8 in the right maxillary sinus.

The patient was maintained on Amoxicillin and sinus precautions for an additional week until removal of the tooth could be performed under intravenous sedation. Retrieval was carried out with a vestibular incision from tooth #1-1 – #1-6 and a Caldwell-Luc approach was employed to gain access to the right maxillary antrum (Fig. 4). The dimensions of the tooth were measured from the CT pre-operatively and the bone window was created ensuring adequate clearance superior to the apices of the adjacent tooth roots.
With full visualization, it was noted that the #1-8 and the maxillary tuberosity were displaced into the sinus. Following retrieval of the tooth and tuberosity (Fig. 5), fixation bone plates were applied to stabilize the bone window (Fig. 6) and the wound was closed using a 3-0 chromic gut suture. The patient was then placed on two weeks of antibiotics and six weeks of sinus precaution. Follow up appointments were arranged, and their post-operative course was uneventful.
Fig. 4
Intraoperative image of the bone window created in the anterior sinus wall. White arrow points to tooth #18.

Fig. 5
Specimens obtained from the right maxillary sinus include tooth #1-8 and a bone fragment from the maxillary tuberosity. Locating the tuberosity in the sinus at the time of tooth retrieval indicates excessive forces applied at the time of initial surgery.

Fig. 6
Closure of the bone window with internal fixation.

Case 2
A 19-year-old patient was undergoing routine extraction of impacted tooth #3-8 when the tooth was displaced medially into the floor of mouth. The patient was subsequently referred to our service at LHSC for examination and definitive management. On examination, the patient was in no acute distress and the tooth was palpable bimanually in the left floor of mouth, however, it was not visible. Examination of the extraction socket revealed a fracture of the lingual cortex. A panorex and CT were obtained which revealed displacement of tooth #3-8 into the left submandibular space (Figs. 7-9). The patient was placed on antibiotics and referred to the Department of Oral and Maxillofacial Surgery at the London Health Sciences Center.
Treatment options included immediate or delayed retrieval. We elected to delay treatment to allow for fibrosis of the soft tissue around the tooth to encapsulate it, stabilize its position and therefore minimize the potential for further displacement at the time of definitive surgical retrieval. The patient was seen for follow up and approximately three months after initial presentation, the patient was then taken to the operating room where general anaesthesia was administered and tooth #3-8 was removed with a trans-oral approach with intra-operative real-time imaging using fluoroscopy with triangulation (Fig. 10). This technique requires localization with spinal needles and multiple intra-operative fluoroscopic images taken at different angulations to develop an appreciation for the object in 3-dimensions. The tooth was removed transorally, however, if this had not been successful, a submandibular extra-oral approach would be used. Following retrieval of tooth #3-8, the wound was thoroughly irrigated and closed. The patient healed without any sequelae and the post-operative period was uneventful. In particular, there was no injury to the inferior alveolar neurovascular bundle, lingual neurovascular bundle or submandibular duct.
Fig. 7
A Panorex of the patient from case two demonstrating inferior displacement of tooth #3-8.

Fig. 8
An axial section of the CT demonstrating the position of tooth #3-8 relative to the mandible.

Fig. 9
Coronal (left) and sagittal (right) sections of a CT of the patient demonstrating the displacement of tooth #3-8.


Fig. 10
Intraoperative image obtained via fluoroscopy. Spinal needle (A) held in position by a hemostat (B) is in place marking the location of tooth #3-8. A side action mouth prop (C) maintains the patient’s mandible in a stable position. The nasoendotracheal tube is labelled (D).

Discussion
Displacement of a third molar beyond the socket is a rare complication that can happen to the most experienced surgeon and the likelihood of this complication is increased with excessive or uncontrolled force. 3 In addition, patient specific anatomic factors such as lingual tooth position or fenestration of the lingual cortex are also associated with a higher incidence of displacement. 1
To minimize the incidence of displacement, adherence to basic surgical principles is recommended. This includes gaining appropriate and generous surgical access with flap development, adequate bone removal and sectioning of teeth where appropriate to minimize any undue application of force. With creation of purchase points via bone removal and section of the tooth, dental elevators can be utilized to elevate the tooth from the socket, minimizing the application of force in a buccal to lingual manor.
It is of the authors opinion that should a practitioner displace a tooth or fragment accidentally during the extraction, and the tooth not be easily seen and grasped, the procedure should be terminated and the patient promptly referred to an oral and maxillofacial surgeon for definitive management. Attempted retrieval without thorough understanding of the anatomy, can lead to unnecessary tissue damage and displacement of the tooth/fragment to deeper spaces, further complicating the process. Some surgeons recommend retrieval as early as possible to minimize pain, swelling, trismus and infection; 1,3 however, others recommend delaying treatment from 3-6 weeks to facilitate the formation of a fibrous scar, which encapsulates the tooth and therefore offers positional stability during retrieval. 2,5,9,10 In both cases described, delayed treatment was utilized, without untoward effect on the patient
The technique we describe for Case 1 utilized the Caldwell-Luc approach which was first described over 100 years ago. 8 It is a standard procedure for accessing the maxillary sinus that has been described frequently in the literature for treatment of this nature. 7,11 The main advantages of this technique are good surgical access and predictability. Some of the reported disadvantages are facial asymmetry due to soft tissue collapse, paresthesia, oroantral fistulas and devitalized teeth. 12
The technique we describe for Case 2 utilized C-Arm fluoroscopy with triangulation. This technique has previously been described by Pandyan et al. It involves the insertion of two spinal needles towards the foreign body followed by the application of a tube shift technique by taking multiple radiographs at various angulations to create triangulation between the two needles and the foreign body. This allows for an appreciation of the object in 3-dimensions. Once this has been established, the correct plane of dissection can be obtained. This is particularly useful when tissue is grossly inflamed and tissue planes have been lost. 4 This technique is beneficial in reducing operative time and soft tissue manipulation, therefore reducing the risk of complications.
Other intra-operative techniques have also been used. Navigation has become increasingly popular, in which a pre-operative CT scan is obtained and then registered to the patient while under general anaesthesia. A probe is then used to correlate the position on the patient to the CT scan. This allows direct feedback to the surgeon while they are operating. Campbell and Costello reported a case using navigation for the removal of a tooth from the infratemporal fossa. 5 Limitations of this technology are that any change in the position of the object, such as deeper displacement at the time of surgery, will not be reflected on the original CT scan. Intra-operative CT in which real-time scanning can occur while the patient is under anaesthesia can address this limitation, however, not all centers are equipped with this expensive technology and increased radiation exposure to the patient will also ensue. 4
The importance of detailed and accurate imaging cannot be overstated. A panorex alone is not sufficient to appropriately localize a displaced tooth. Two-plane imaging is the minimum required and if possible, 3-dimensional imaging with a CT scan is ideal. More advanced imaging such as intra-operative navigation or intra-operative CT should be reserved for cases in which there is close proximity to vital structures or access is severely limited.
Displacement of maxillary and mandibular third molars during extraction is a rare but potentially serious complication that can be managed either immediately or delayed, depending on the clinical situation. Patient well being is of utmost importance and the described cases demonstrate two successfully retrieved third molars using delayed treatment, with good outcomes in both instances thanks to timely referral. OH
Oral Health welcomes this original article.
References
1. Huang IY, Wu CW, Worthington P. The displaced lower third molar: a literature review and suggestions for management. Journal of Oral and Maxillofacial Surgery. 2007. 65: 1186 – 1190.
2. Sencimen M, Gulses A, Secer S, Zerener T, Ozarslanturk S. Delayed retrieval of a displaced maxillary third molar from infratemporal space via trans-sinusoidal approach: a case report and review of the literature. Oral and Maxillofacial Surgery. 2016. 1 -6.
3. Esen E, Aydogan LB, Akcalt C. Accidental displacement of an impacted mandibular third molar into the lateral pharyngeal space. Journal of Oral and Maxillofacial Surgery. 2000. 58: 96-97.
4. Pandyan D, Nandakumar N, Qayyumi BN, Kumar S. C-Arm fluoroscopy: a reliable modality for retrieval of foreign bodies in the maxillofacial region. The Journal of Contemporary Dental Practice. 2013; 14(6): 1193-1196.
5. Campbell A, Costello BJ. Retrieval of a displaced third molar using navigation and active image guidance. Journal of Oral and Maxillofacial Surgery. 2010. 68: 480 – 485.
6. Gao QM, Yang C, Zheng LY, Hu YK. Removal of long-term broken roots displaced into the maxillary sinus by endoscopic assistant. The Journal of Craniofacial Surgery. 2016. 27(1): 77-80.
7. De Souza Amorim K, da Silva VT, da Cunha RS, Souto ML, Sao Mateus CR, de Almeida Souza LM. Removal of an upper third molar from the maxillary sinus. Case Reports in Dentistry – Hindawi. 2015. 1 – 5.
8. Barzilai G, Greenberg E, Uri N. Indications for the Caldwell-Luc approach in the endoscopic era. Otolaryngology Head and Neck Surgery. 2005. 132(2):219-220.
9. Gomez-Oliveira G, Arribas-Garcia I, Alvarez-Flores M, Gregoire-Ferriol J, Martinez-Gimeno C. Delayed removal of a maxillary third molar from the infratemporal fossa. Medicina Oral Pathologia Oral Cirugia Bucal. 2010. 15(3);509 -511.
10. Orr DL. A technique for recovery of a third molar from the infratemporal fossa: case report. Journal of Oral and Maxillofacial Surgery. 1999. 57: 1459 – 1461.
11. Ramanojam S, Halli R, Hebbale M, Bhardwaj S. Ectopic tooth in maxillary sinus: case series. Annals of Maxillofacial Surgery. 2013. 3(1): 89 – 92.
12. DeFreitas J, Lucente FE. The Caldwell-Luc procedure: institutional review of 670 cases: 1975-1985. Laryngoscope. 1988. 98: 1297-1300.
About the Authors
 Lachlan McLean, Oral and Maxillofacial Surgery Resident, Schulich School of Medicine and Dentistry, Western University and Department of Oral and Maxillofacial Surgery, London Health Sciences Centre, London, Ontario. E-mail: Lachlan.mclean@lhsc.on.ca
Lachlan McLean, Oral and Maxillofacial Surgery Resident, Schulich School of Medicine and Dentistry, Western University and Department of Oral and Maxillofacial Surgery, London Health Sciences Centre, London, Ontario. E-mail: Lachlan.mclean@lhsc.on.ca
 Jeff Soparlo, Oral and Maxillofacial Surgery Resident, Schulich School of Medicine and Dentistry, Western University and Department of Oral and Maxillofacial Surgery, London Health Sciences Centre, London, Ontario. E-mail: Jeff.soparlo@lhsc.on.ca
Jeff Soparlo, Oral and Maxillofacial Surgery Resident, Schulich School of Medicine and Dentistry, Western University and Department of Oral and Maxillofacial Surgery, London Health Sciences Centre, London, Ontario. E-mail: Jeff.soparlo@lhsc.on.ca
 Jerrold E. Armstrong, Associate Professor, Schulich School of Medicine and Dentistry, Western University and Chief of Dentistry, London Health Sciences Centre, London, Ontario.
Jerrold E. Armstrong, Associate Professor, Schulich School of Medicine and Dentistry, Western University and Chief of Dentistry, London Health Sciences Centre, London, Ontario.
RELATED ARTICLE: Palatally Displaced Canines Is There A Way To Prevent Impaction Of These Teeth?
Follow the Oral Health Group on Facebook, Instagram, Twitter and LinkedIn for the latest updates on news, clinical articles, practice management and more!









