The restoration of endodontically treated teeth (ETT) has been guided historically by anecdotal empiricism rather than biomechanical dynamics. Decisions regarding the configuration of the restoration, the diameter of the post channel and the post and core materials to be used have plagued foundational dentistry for decades.1,2 The loss of coronal tooth structure due to caries,3 excessive access cavity design4,5 and the taper of the root canal preparation are vectors that will create stress at the cervical region during functional loading.6,7 The ongoing confusion regarding design and materials has caused paradoxical statements and illogical contradictions to be factored into the restorative matrix for ETT.
The introduction of fibre posts has altered the root to restoration harmonic. Fibre posts provide a reliable alternative to metal posts (cast or prefabricated) as their modulus of elasticity (20 GPa) is closer to dentin than metal posts (200 GPa). Stiff, hard metal posts transfer forces along their long axis creating a wedging effect on tooth structure. This can lead to catastrophic failure. The use of fibre posts obviates such an event.8,9
Factors in the decision-making process for the use of posts include:10-24
ETT are weakened by the loss of strategic tooth architecture resulting in structural and occlusal compromise. This is dependent on the amount of native tooth structure removed due to previous or existing caries, the state of the current restoration and the volume of tooth structure removed during the endodontic treatment procedure. ETT are more vulnerable to tooth loss than teeth with vital pulps due to the possibility of either recrudescent or persistent post-treatment disease subsequent to root canal treatment.25 Historically, ETT were considered to be brittle, subject to fracture due to the loss of tooth vitality, decreased moisture content, resultant inelasticity and the loss of collagen cross-linking. Contemporary studies comparing ETT to contralateral vital teeth challenge these findings; no decrease in compressive or tensile strength was associated with changes in the water content of dentin.26-30
In the case of ETT, the distribution of stress concentration zones and the magnitude of tensile stresses has been perceived to increase significantly when tooth structure is lost, or occlusal loads are delivered off-angled to the long axis of the tooth. Fracture resistance is a function of resistance to deformation under load. Restorative materials are less likely to endure stress vectors with sustained load further validating the need for bio-minimalism of ETT restorations.31-35 As well, the loss of tooth structure at the floor of the pulp chamber in ETT leads to significant biomechanical changes in as little as three weeks, with ensuing recontamination of the pulp canal space, resulting in a higher incidence of fractures.36,37 The more native tooth structure retained in ETT, the more enhanced the load management during function, the more effective the stress management and the more predictable the long-term prognosis.38,39
Biologic Width
Biologic width (BW) is the natural seal that develops around teeth and that protects the alveolar bone from infection and disease (Fig. 1). The dimension of BW is not a constant; it depends on the location of the tooth in the alveolus, it varies from tooth to tooth and the configuration of the tooth. BW is essential for the preservation of periodontal health. It is sustained by the removal of any irritation that might damage the periodontium (marginal discrepancies). Exposure of sufficient sound tooth structure in the case of a deep subgingival tooth fracture or carious lesions enhances the retention of the restoration, ensures accurate impression taking and enables correct placement of the restoration margins without violating the BW. This is an imperative in the esthetic zone in patients with uneven gingival margins or excessive gingival display.40,41
Fig. 1

The choice of marginal position is either supragingival, equigingival or subgingival. Restorations placed where the alveolar bone is thin or the gingiva is thin and highly scalloped are prone to recession.42,43 When a restoration invades the biological width, the body’s response is to move the attachment zone apically until a tolerable biological width is re-established.44
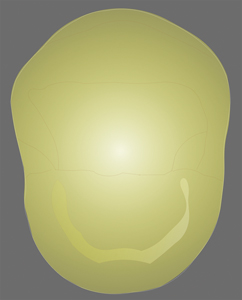
Ferrule
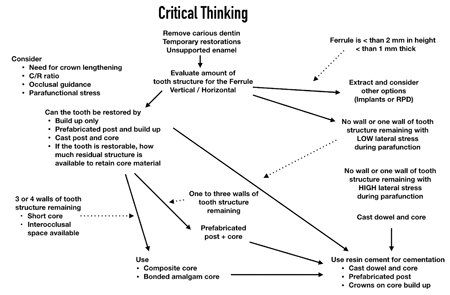
The “ferrule effect” is an enduring foundational tenet in restorative dentistry. It is defined as the height of natural tooth structure extending from the crown margin coronally. Numerous studies have reported that 2 mm of ferrule is required to resist displacement45,46 of the crown from the remaining tooth structure. The effectiveness of the ferrule in the restoration of ETT is determined by; 1) the height and width, 2) the number of remaining walls, 3) the location of the ferrule, 4) the condition of the residual tooth structure, 5) the tooth type and 6) the degree of parafunctional loading (Fig. 2).47
Fig. 2

Exposure of sufficient sound tooth structure in the case of deep subgingival fractures and/or carious lesions enhances the retention of the restoration and enables correct placement of the restoration margins without violating the biologic width. This improves aesthetics in patients with uneven gingival margins and excessive gingival display.48,49 In situations where a substantial volume of tooth structure is lost, adhesive materials will not overcome the lack of ferrule and should not be an alternative to sound engineering principles when restoring ETT.
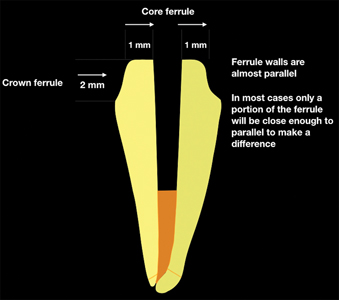
There are two ferrules; the crown ferrule and the core ferrule. The greater the height of residual tooth structure above the margin of the preparation (crown ferrule), the greater the fracture resistance. The same premise applies to the buccal thickness (core ferrule).50 Ideally, 2.0 mm of crown ferrule and 2.4 mm of dentin thickness (core ferrule) minimizes the fracture potential in molars. Full coverage preparation for ETT maxillary and mandibular bicuspids, regardless of the coronal ferrule height, results in diminished buccal thickness and increased fracture potential (Fig. 3).51-53
Fig. 3
There are numerous contraindications to achieving an ideal ferrule; immunological disease, close adjacent roots, tori, the ascending ramus, occlusion, muscle insertions, furcation exposure and lip position.54 It is best to do a risk-benefit analysis by creating a provisional restoration prior to crown lengthening to ensure the restorative treatment plan objectives can be met (Fig. 4).
Fig. 4

The Paradigm Shifts
The developments in adhesive restorative technologies and techniques enable functional and aesthetic reconstruction of debilitated tooth structure when adequate coronal tooth structure remains. A more conservative non-invasive rehabilitation is possible for rebuilding the integrity of the residual tooth structure.55 Improvements in direct restorations relating to the enhanced properties of composite resins engender a shift in the traditional default full coverage treatment plan.
In order to compensate for parafunctional occlusal forces, the marginal placement of a protective restoration should provide cuspal coverage.56 Posterior teeth that have undergone ETT have been reported to have greater cuspal flexure then non-ETT. Teeth missing marginal ridges allow greater cuspal flexure than teeth with intact marginal ridges, whether ETT or non-ETT. Direct or indirect onlays can be used when there is residual tooth structure that is not undermined and if the marginal ridges are intact. Onlays with cuspal shoeing and full coverage crowns restrict cuspal displacement and will prevent coronal fracture under loading (Fig. 5).57
Fig. 5
Clark58 advocates a substantially altered perspective on the reconstruction of ETT; 1) enamel bevels, 2) flared walls, 3) aluminum oxide blasted 4) and etched and uncut enamel. He advocates monolithic composites in contrast to porcelain fused to metal, dilithium silicates, and zirconia. He recommends not to layer, the use of a translucent matrix system and the removal of biofilms with a pressurized air-water-mild abrasive slurry.58 This will be discussed in depth in Part II.
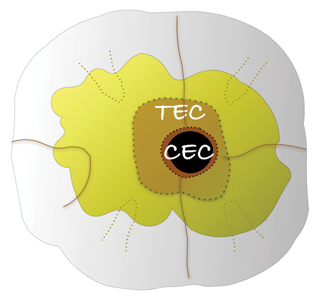
Access Cavity Design Revision
Recently, a trend to patient centric conservative endodontic cavities (CEC) has changed the focus of the restoration of ETT.59 As the adhesion era in restorative dentistry progresses, extra-coronal restorations requiring minimal preparation are replacing full coverage restorations depending upon the volume of tooth structure remaining. The CEC concept recognizes that endodontics is restoratively driven; an access to apex, apex to access paradigm that preserves peri-cervical dentin to diminish the potential for fracture. Traditional endodontic cavities (TEC) are procedure centric and prone to structural compromise. Logically, a balance between the preservation of native tooth structure and dentin removal for access to the canal system is beneficial. However, a minimal access could compromise the efficacy of debridement and disinfection as it limits access to the entirety of the root canal system. The size reduction engenders the possibility that infected tissue could remain and iatrogenics ensue (Figs. 6A-6D).60
Fig. 6A

Fig. 6B
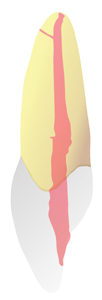
Fig. 6C
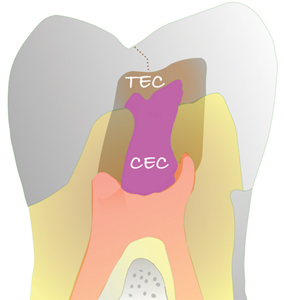
Fig. 6D
Decision making for restoring ETT:
• Best practices; remove the restoration(s) and carious tooth structure prior to endodontic treatment in order to evaluate the restorative matrix.
• Best practices; assess how occlusal forces affect the EET in regard to the angulation and the biomechanics of the residual tooth structure. Determine the algorithm of success with cuspid protected occlusion or group function on a single tooth, a bridge abutment, an abutment for an RPD, a single tooth adjacent to an implant retained prosthesis.
• Best practices; crown lengthening considerations
• Short clinical crowns
• Placement of subgingival restorative margins
• Excessive occlusal or incisal wear
• Inadequate interocclusal space
• Partial restorative ferrule
• Best practices; boxes or grooves for secondary retention
• Best practices; Would cementation of a crown on tooth structure be more effective than on core material
• Best practices; Choice of bonding agent, total-etch or self-etch resin cements
Conservative non-invasive rehabilitation in the adhesion era:
• Best practices; Are posts a prerequisite for all ETT?
• Best practices; Is there an evidence- based data analysis that fibre post systems are preferable to cast or prefabricated metal?
• Best practices; Is there evidence-based data analysis that restorations without posts are reliable and predictable?
• Best practices; Are there alternative means by which to reinforce teeth?
• Best practices; Are there predictable adhesive restorative protocols for ETT?
Fig. 7A1

Fig. 7A2
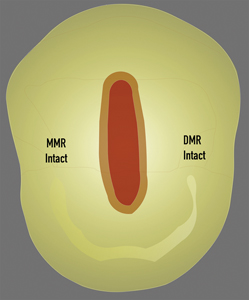
Fig. 7B

Fig. 7C1

Fig. 7C2
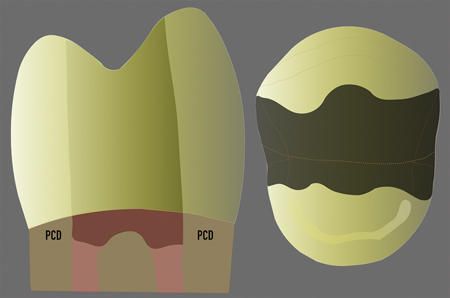
Fig. 7D
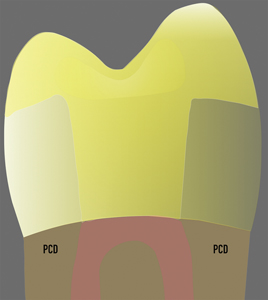
Fig. 8A

Fig. 8B
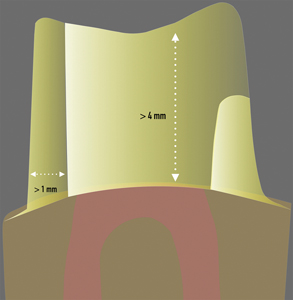
Fig. 9A

Fig. 9B
Conclusion
The voyage from anecdotal empiricism to scientifically validated protocols used for the restoration of ETT continues. Fundamental best practices are changing. Historically, posts/cores and the circumferential reduction of residual tooth structure were the standard technique for restoration of ETT. These aggressive procedures appeared to enhance failure possibilities. Investigations from the past and those ongoing do not provide evidentiary science that conclusively substantiates post composition, post shape, core material choice, ferrule height and width. Improvements in dentinal adhesives and biosmart materials appear to provide an alternative restorative paradigm with maximum preservation of tooth structure and a balance between esthetics and structural resilience.
Oral Health welcomes this original article.
Disclaimer: Part two of this article will provide a matrix for the choice of posts, the choice of core material and the choice of restoration. The author wishes to thank Clinical Research Dental for their support of this manuscript.
References
- Stokes AN. Post crowns: a review. Int Endodon J January 1987; 20(1):1-52
- Shillingburg HT, Hobo S, Whitsett LD. Fundamentals of Fixed Prosthodontics. Quintessence Publishing, Chicago 1978
- Linn J, Messer HH. Effect of restorative procedures on the strength of endodontically treated molars. October 1994;20(10):479–485
- Silva EJNL, Rover G et al. Impact of contracted endodontic cavities on fracture resistance of endodontically treated teeth: a systematic review of in vitro studies. Clin Oral Investig January 2018 Jan;22(1):109-118
- Krishan R, Paque F. Impacts of Conservative Endodontic Cavity on Root Canal Instrumentation Efficacy and Resistance to Fracture Assessed in Incisors, Premolars, and Molars
- Sabeti M, Kazem et al. Impact of Access Cavity Design and Root Canal Taper on Fracture Resistance of Endodontically Treated Teeth: An Ex Vivo Investigation. 2018 Sep;44(9):1402-1406
- Zogheib C, Sfeir G et al. Impact of minimal root canal taper on the fracture resistance of endodontically treated bicuspid. J Int Soc April March April 2018;8(2):179-183
- Bateman G, Ricketts DN, Saunders WP. Fibre based post systems: a review. Br Dent 2003;195:43–48
- Lamichhane A, Xu C, Zhang F. Dental fiber-post resin base material: a review. February 2014;6(1):60-65
- Haapasalo M, Shen Y, Quan W, Gao Y. Irrigation in Endodontics. Dent Clin N Am 2010:291-312
- Uzunoglu E, Aktemur S, Uyanik MO, Durmaz V, Nagas E. Effect of ethylenediaminetetraacetic acid on root fracture with respect to concentration at different time exposures. J Endod. 2012 Aug;38(8):1110-3
- KO CX, Chu CS, Chung KH, et al: Effects of posts on dentin stress distribution in pulpless teeth. J Prosthet Dent;1992;68:421-427
- Salameh Z, Sorrentino R, Ounsi HF, Sadig W, Atiyeh F, Ferrari M. The effect of different full coverage crown systems on fracture resistance and failure pattern of endodontically treated maxillary incisors restored with and without glass fiber posts. JOE July 2008;34(7):842.
- Hunter AJ, Feiglin B, Williams JF. Effects of post placement on endodontically treated teeth. J Prosth Dent 1989;62:166-172
- Ferrari M, Cagidiaco MC, Grandini M, De Sanctis M, Gorraci C. Post placement affects survival of endodontically treated premolars. J Dent Res 2007;86(8):729-734
- Nothdurft FP, Seidel E, Gebhart F, Naumann M, Motter PJ, Pospiech PR. The fracture behavior of premolar teeth with class II cavities restored by both direct composite restorations and endodontic post systems. J Dent June 2008;36(6):444-449
- Bachicha WS, DiFIore PM et al. Microleakage of endodontically treated teeth restored with posts. J Endodon November 1998;24(11):703-708
- Stone S, Whitworth, Wassell. Viability of posts and cores (Extra-coronal restorations) August 2018;BDJ Clinician’s guides:115-133
- Greenfeld RS, Marshall FJ. Factors affecting dowel (post) selection, use in endodontically treated teeth. J Can Dent Assoc 1983;49:777-83
- Peutzfeldt A, Sahafi A, Asmussen E. A survey of failed post-retained restorations. Clin Oral Invest 2008;12:37-44
- Saedi A, Hamidi M, et al. Effect of different torques on dentinal crack formation following canal preparation using neoniti rotary systems. Cas J Dent Res March 2018;7(1):8-13
- Scioscia A, Helfers A et al. Performance of monolithic and veneered zirconia crowns after endodontic treatment and different repair strategies. Op Dent March/April 2018;43(2):170-179
- Awawdeh L, Hemaidat K, Al-Omari W. Higher Maximal Occlusal Bite Force in Endodontically Treated Teeth Versus Vital Contralateral Counterparts. J Endodon June 2017;43(6):871-875
- de Chevigny C, Dao TT, et al. Treatment outcome in endodontics: the Toronto study—phase 4: Initial treatment. J Endodon March 2008;34(3):258-63
- Huang TJ, Schilder H, Nathanson D. Effects of moisture content and endodontic treatment on some mechanical properties of human dentin. J Endodon 1991;18:209–15
- Helfer AR, Melnick S, Schilder H. Determination of the moisture content of vital and pulpless teeth. Oral Surg Oral Med Oral Path 1972;34:661-70
- Papa J, Cain C, Messer HH. Moisture content of vital vs endodontically treated teeth. Endodontics & Dental Traumatology. 1994;10(2):91–93
- Kishen A. Biomechanics of fractures in endodontically treated teeth. Endodon Topics October 2015;33:3-13
- Benazzi S, Nguyen HN, Kullmer O, Hublin JJ. Unravelling the Functional Biomechanics of Dental Features and Tooth Wear July 2013;8(7):1-10
- Assif D, Gorfil C. Biomechanical considerations in restoring endodontically treated teeth. J Pros Dent June 1994;71(6):565-567
- Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical consideration of endodontically treated teeth: asystematic review of the literature. Part 1. Composition and micro-macrostructure alterations. Quintessence Int 2007;38:733-43
- Tang W, Wu Y, Smales RJ. Identifying the risks for potential fractures in endodontically treated teeth. J Endodon 2010;36:609-17
- Chun KJ, Choi HH, Lee JY. Comparison of mechanical property and role between enamel and dentin in the human teeth. J Dent Biomech February 2014
- Zhu J, Rong Q, Wang X, Gao X. Influence of remaining tooth structure and restorative material type on stress distribution in endodontically treated maxillary premolars: A finite element analysis. J Pros Dent May 2017;117(5):646-655
- Cumbo E, Gallina G. Leakage in the root canal system during and after treatment: A review. Int J Clinic Dent 2017;10(3):163-176
- Abramovitz L, Lev R, Fuss Z, Metzger Z. The unpredictability of seal after post space preparation: a fluid transport study. J Endodon April 2001;27(4):292-5
- Sjogren U, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endodon October 1990;16(10):498-504
- Harlur BH, Ahmari MA, et al. The effect of intra-radicular multiple fiber and cast posts on the fracture resistance of endodontically treated teeth with wide root canals. Bio Res Int August 2018
- Sarfati A, Tirlet G. Deep margin elevation versus crown lengthening: biologic width revisited. Int J of Esthetic Dent. January 2018;13(3)334-356
- Nugala B, Santosh Kumar BB, Sahitya S, Mohana Krishna P. Biologic width and its importance in periodontal and restorative dentistry J Conserv Dent. 2012 Jan-Mar; 15(1): 12–17
- Kois JC. The restorative-periodontal interface: Biological parameters. Periodontol 2000 1996;11:29–38
- Jorgic-Srdjak K, Dragoo MR, Bosnjak A, Plancak D, Filipovic I, Lazic D. Periodontal and prosthetic aspect of biological width part II: Reconstruction of anatomy and function. Acta Stomatol Croat 2000;34:441-4
- de Wall H, Castellucci G, The importance of restorative margin placement to the biologic width and periodontal health. Part II. Int J Periodontics Rest Dent. February 1994;14(1):70-83
- Nevins M, Skurow HM. The intracrevicular restorative margin, the biologic width, and the maintenance of the gingival margin. Int J Periodont Restor Dent 1984;4:30-49.
- Santos Pantaleón D, Morrow BR, Cagna DR, Pameijer CH, Garcia-Godoy F. Influence of remaining coronal tooth structure on fracture resistance and failure mode of restored endodontically treated maxillary incisors. J Prosthet Dent. March 2018;119(3):390-396
- Tan PL, Aquilino SA, Gratton DG et al. In vitro fracture resistance of endodontically treated central incisors with varying ferrule heights and configurations. J Pros Dent 2005;93(4):331-336
- Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Pros Dent 1990;63(5):529-536
- Jotkowitz A, Samet N. Rethinking ferrule – a new approach to an old dilemma. Brit Dent J July 2010;209(1):25-33
- Frankenberger R, Lohbauer U, Roggendorf MJ, Naumann M. Selective enamel etching reconsidered: Better than etch-and-rinse and self-etch? Journal of Adhes Dent November 2008;10(5):339-344
- Kois JC. The restorative-periodontal interface: biological parameters. Periodontology 2000 1996;11:29-38
- Magne P, Lazari PC, Carvalho MA et al. Ferrule-effect dominates over use of a fiber post when restoring endodontically treated incisors: An in vitro study. Oper Dent July/August 2017;42(4):396-406
- Shamseddine L, Chaaban F. Impact of a Core Ferrule Design on Fracture Resistance of Teeth Restored with Cast Post and Core. Adv Med Jun 2016
- Dua N, Kumar B, Arunagiri D et al. Comparative evaluation of the effect of different crown ferrule designs on the fracture resistance of endodontically treated mandibular premolars restored with fiber posts, composite cores, and crowns: An ex-vivo study J Conserv Dent May 2016;19(3):264–269
- Sirajuddin S, Narasappa K et al. Iatrogenic damage to the periodontium by restorative treatment procedures: An overview. Open Dent J June 2015;9:217-222
- Polesel A. Restoration of the endodontically treated posterior tooth. The restoration of the posterior tooth treated endodontically. Ital J of Endodon June 2014 ;28(1):2-16
- Schwartz RS, Robbins JW. Post placement and Restoration of Endodontically Treated Teeth: A literature review.
- Krishan R, Paque F, Ossareh A et al. Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars J Endodon 10.1016/j.joen.2013.12.012. Epub 2014 Jan 28.
- Clark D. The Injection Molded Class II Restoration. Dentistry Today.
- Plotino G, Grande NM, Isufi A, Ioppolo P, et al. Fracture strength of endodontically treated teeth with different access cavity designs. June 2017;43(6):995-1000
- Boveda C, Kishen A. Contracted endodontic cavities: the foundation for less invasive alternatives in the management of apical periodontitis. Endodontic Topics November 2015;33(1):169-186.
About The Author
 Kenneth S. Serota, DDS, MMSc, graduated from the University of Toronto Faculty of Dentistry in 1973 and received his Certificate in Endodontics and Master of Medical Sciences degree from the Harvard-Forsyth Dental Center in Boston, Massachusetts in 1981. Active in online education since 1998, he is the founder of the Endodontic forum ROOTS and the interdisciplinary Facebook forum NEXUS. Dr. Serota is a clinical instructor in the University of Toronto postdoctoral endodontics department. He is the social media and marketing director for Navident Dynamic Navigation.
Kenneth S. Serota, DDS, MMSc, graduated from the University of Toronto Faculty of Dentistry in 1973 and received his Certificate in Endodontics and Master of Medical Sciences degree from the Harvard-Forsyth Dental Center in Boston, Massachusetts in 1981. Active in online education since 1998, he is the founder of the Endodontic forum ROOTS and the interdisciplinary Facebook forum NEXUS. Dr. Serota is a clinical instructor in the University of Toronto postdoctoral endodontics department. He is the social media and marketing director for Navident Dynamic Navigation.
RELATED ARTICLE: Evolving Excellence: Scientific Advances In Dentistry And New Restorative Paths
Follow the Oral Health Group on Facebook, Instagram, Twitter and LinkedIn for the latest updates on news, clinical articles, practice management and more!












