Introduction
Consider a new patient who has come to a dental office and undergoes a screening examination. A quick look at any missing teeth may prompt a dentist to ask, why were these teeth lost? While patient responses may be vague, the answer often involves fractured endodontically treated teeth (ETT). For the most part, teeth that require endodontic treatment have already undergone a prior sequence of restorative procedures, which invariably results in dentin loss and structural weakening. The addition of endodontic treatment to this sequence removes additional coronal and radicular dentin and potentially further decreases fracture resistance.1 Dentin removal during root canal treatment (RCT) is considered an operator (modifiable) factor that could be associated with increased vertical root fracture incidence. Vertical root fractures (VRF) are defined as fractures, usually involving ETT, that are initiated exclusively in the root and ultimately lead to tooth loss.
The goal of endodontic treatment is stated as the “prevention and healing of apical periodontitis”.2 Over the last six decades, much of the endodontic research has been focused on how to successfully manage apical periodontitis (AP). The monitoring of AP progression consists of two parts: a clinical aspect that is focused around patient symptoms and a time-dependent radiographic evaluation of bone volume changes around root apices. Clinical symptoms, if present, most frequently resolve fairly quickly after RCT, however the radiographic evaluation has formed the main focus of endodontic outcomes research. These clinical studies, albeit very few in comparison to laboratory research, have inherent flaws, some of which include short observation times, uncontrollable confounding variables, low patient sample sizes and loss of patients to follow-up.3,4 These shortcomings contribute to the difficulty many researchers have had when trying to find direct correlations between the technical aspect of RCT and radiographic ‘healing’ of apical periodontitis. Thus, over the years, dentists performing RCT have been forced to make clinical decisions under high levels of uncertainty.5 While clinicians place a high value on radiographic healing of periapical tissues, this outcome measure may be meaningless to asymptomatic patients who desire long-term tooth survival.
An outcome is defined as an end result or event succeeding an action. For the most part, outcomes in dentistry can be divided into process-centered outcomes and patient-centered outcomes.45 A process-centered outcome relates to the way in which the operator exercises their dexterity to satisfy the technical standards of a procedure, either non-surgical or surgical. In endodontics, many process-centered outcomes are assessed by the ‘look’ of the immediate post-operative radiograph.
Education and clinical practice in dentistry historically stem from the biomedical model which focuses on disease management.6 Clinicians are often unaware of this model and how it governs their reasoning since it represents the norm that cannot be questioned.7 Dental interventions consist of surgical procedures in the oral cavity. “Traditionally, these interventions are performed with an undivided focus on the process”.8 Consequently, dentists remain focused on technical processes, not realising how these may translate on some occasions to unfavorable
patient-centered outcomes. Furthermore, research suggests that clinicians think they know what patients want and do not try to find out what patients actually want.9 Patient-centered outcomes relate to variables that matter to patients. It puts the attention on the patient’s priorities rather than the clinician’s.10 In the context of endodontics, a central component of patient-centred outcomes is the long-term asymptomatic and functional retention of ETT,11 which entails longevity of treatment. Research has suggested that conservation of tooth structure, together with placing quality permanent restorations can lead to improved tooth survival outcomes.12 The aim of this review is to explore the most common reasons for extraction of ETT and to provide insights on treatment modalities that may have the potential to improve patient-centered outcomes.
Why Are Endodontically Treated Teeth Extracted?
Extractions of ETT, in order of prevalence, are mostly associated with non-restorability, recurrent caries, compromised periodontal support, VRF and clinician/patient decisions (often related to a poor understanding of the cost-effectiveness of available treatment options), with causes of true endodontic origin at the bottom of the list.12-17 A true endodontic cause for extraction of ETT is exclusively defined as a lack of periapical radiographic healing or the presence of clinical signs and symptoms of endodontic origin. They account for only 4 per cent of the reasons for extraction of ETT at the 20-year mark.18 Furthermore, the risk of persistent clinical symptoms or painful flare-ups associated with ETT is low (5.8 per cent at 20 years).19 Extractions of ETT have multifactorial aetiologies and for simplicity sake, can be divided into non-modifiable and modifiable factors. Non-modifiable factors include the amount of tooth structure remaining from previous caries and restorative procedures, previous coronal tooth fractures, uncontrolled periodontal disease, parafunctional habits, malocclusion, terminal position in the arch and inherent tooth anatomical factors including the presence of isthmuses in mesial roots of mandibular molars. These non-modifiable factors may critically misguide the projection of survival times for all teeth receiving endodontic therapy. In contrast, modifiable factors can be controlled by the clinician to possibly improve patient-centered outcomes. By far the most common modifiable factors are the removal of coronal and radicular dentin during access cavity preparation, root canal shaping and post space preparation. Treatment approaches that address these modifiable factors by minimizing coronal and radicular dentin removal and the immediate placement of the coronal restoration, may lead to improved survival times of ETT.12
Endodontic Access
Traditional endodontic access design has placed the clinician’s needs for fast, unobstructed, safe and convenient coronal access to the root canal systems above the tooth’s restorative and structural needs. With the introduction of the microscope into endodontics in the mid- 90’s20 coupled with the availability of increasingly more flexible nickel-titanium rotary instruments, the need to cut the traditionally large access cavities became questionable. Within the last 10 years, there has been a shift towards reducing access size to the natural dimensions of the pulp chamber while still addressing the biological objectives of endodontic treatment with the aim of yielding improved survival outcomes. Clark and Khademi,21 initially proposed a hierarchial approach to accessing tooth structure and dental material – which leverages caries, missing tooth structure and existing restorations – to gain access to the root canal system. This process involves skewing the access towards structures of lower value while conserving important healthy tooth tissue. Structures said to have no value include caries, previous restorations, undermined enamel and tertiary dentin. The most valuable structures that must be preserved include peri-cervical dentin (PCD), undermined dentin and axial wall at the dentino-enamel junction.21 PCD refers to the dentin located 4 mm coronal and 6 mm apical to crestal bone (Fig. 1A). It has been proposed that PCD plays a crucial role in transferring occlusal forces along the root and that maintaining intact PCD (Fig. 1B) is arguably the single most important factor in achieving long-term retention of ETT.22 The preservation of PCD can be achieved internally through conservative access preparation and instrumentation and externally, through conservative crown margin preparation (Fig. 2). A traditional access in this lower left molar (Fig. 3) would have most likely ignored the presence of the distal restoration with recurrent caries. An alternative access design leverages the restoration or caries (Figs. 3 & 4), allows for dentin conservation and maintains the “soffit”. The soffit is an overhanging part of the pulp chamber roof remaining after endodontic access, thought to provide extra strength by increasing resistance to bending22 (Fig. 3 & 5).
Fig. 1A & 1B
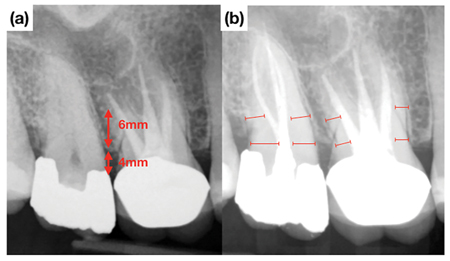
Fig. 2

Fig. 3
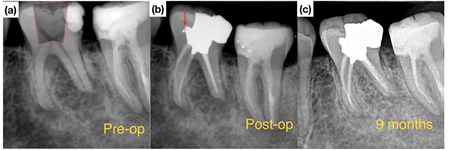
Fig. 4A-H
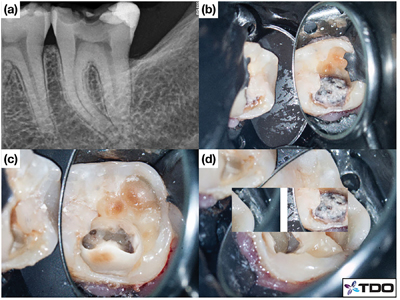

Fig. 5
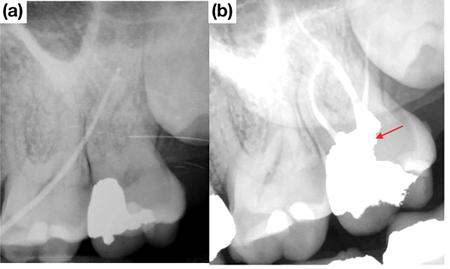
Image-Guided Endodontic Access
Image-guided access utilizes image modalities available to the clinician (2D projection radiography as well as 3D Cone Beam Computed Tomography or CBCT) in order to plan the access cavity more precisely. Instead of prescribing a “one size fits all” access design, the tooth’s specific and unique needs dictate the location and size of the access cavity. The goal is not to make the smallest access possible, but to strategically remove and conserve dentin (Fig. 6). One implementation of image-guided access design is the dual access or “truss” access which is the access design of choice in a mandibular molar when the canal convergence is minimal, and the platform is wide (Fig. 7).45 It is being argued that the preserved dentin structure helps to resist tensile and compressive forces by bracing the lingual and buccal dentin walls (Fig. 8).45
Fig. 6

(h) Final radiograph.
Fig. 7

Fig. 8

with leveraged distal caries which was restored with an amalgam core. The deep finishing line was placed. (c) Post-operative radiograph. (d) 3-year follow-up showing complete periapical bone healing. The patient is asymptomatic.
Dynamically Guided Access
In the early 2000’s, dynamic guidance was introduced in order to help with the accurate placement of dental implants.23 Based on this approach, dynamically guided access (DGA) was first applied in endodontics by Dr. Charles Maupin.24 DGA uses information from the patient’s CBCT volume to plan an access cavity. Overhead tracking cameras relate the position of the patient’s jaw and the clinician’s bur in 3-dimensional space. The clinician, by looking at the software interface, gets immediate feedback about the position of the bur as it relates to the position of the planned access and the tooth.24 Static guides designed based on CBCT and intra-oral scanner data and fabricated by 3D-printing can also guide the clinician during endodontic access or microsurgery.25 DGA provides significant advantages over static 3D-printed guides which lack inter-occlusal distance, can only be utilized with slow speed handpiece burs, take time to prepare and do not allow for minor but important treatment plan changes that may occur during the procedure, which may lead to unnecessary removal of dentin.24 DGA does not require long burs, is compatible with high speed handpiece burs, does not require waiting time for the preparation of a 3D-printed guide and allows real-time treatment plan changes if required (Fig. 9).24
Fig. 9

Conservative Root Canal Instrumentation
What constitutes optimal root canal apical instrumentation size and cervical taper is controversial. For decades, a plethora of instrumentation techniques have been suggested in endodontics but, unfortunately, there are no publications on the long-term effectiveness for any of the techniques. Root canal instrumentation with a large coronal taper was traditionally thought to enhance irrigation and disinfection and provide convenience and resistance form for obturation procedures.26 In vitro studies indicate that increased taper and apical size instrumentation is necessary for irrigation to reach the apex during treatment however, there are no publications indicating if this even translates into improved patient-centered outcomes. On the contrary, these process-centered outcomes could be associated with an increase in vertical root fractures.27 The best available evidence “supports the current intuitive premise that healthful tooth survival is likely to be influenced by the distribution, amount, strength and integrity of remaining tooth tissue”.12 The preservation of intact coronal and radicular tooth tissue, mainly at the PCD level (Fig. 10) has been argued to be the critical factor in achieving a favorable long-term biomechanical response in root-filled teeth (Figs. 11 & 12).22
Fig. 10
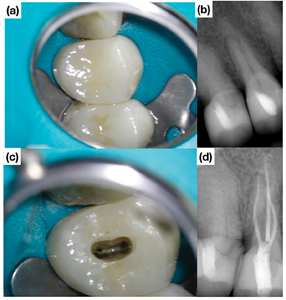
Fig. 11
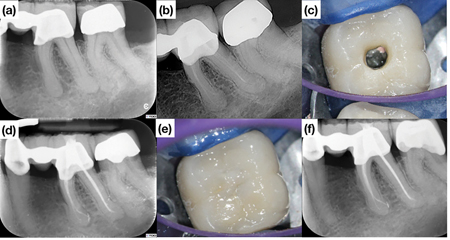
first molar with a radiographic periapical radiolucency treated in two visits. (b) Placement of calcium hydroxide as an
inter-appointment medicament. (c) Conservative access cavity. (d) Post-operative radiograph showing conservative
access preparation and canal instrumentation and placement of amalgam core and (e) tooth colored access closure.
(d) 3-year follow-up showing periapical bone healing. The patient is asymptomatic.
Fig. 12
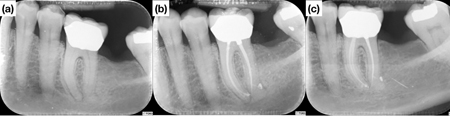
is asymptomatic. 13. Case of Dr. Viraj Vora: (a) Pre-operative radiograph of tooth #2.6. (b) Post-operative radiograph with temporary restoration. (c) 1-year follow-up. (d) Tooth #2.6 has been extracted at the 3-year follow-up.
In vitro and In vivo studies on conservative endodontic treatment
Publications related to conservative endodontics are mainly in vitro experiments which, for the most part, have looked at stress-strain values against volume of dentin loss from access preparations, effect of instrument taper on root dentin removal and canal transportation and length of irrigation exchange to the apical terminus. Such variables are surrogate markers that may correlate to a clinical endpoint (tooth survival or healing) but do not have a guaranteed relationship. As opposed to traditional endodontic cavities (TEC) that include straight line access beyond the canal orifices to the middle third of the root, contracted endodontic cavities (CEC) preserve some of the pulp chamber roof.28,29 In vitro studies using static load to fracture experiments have reported a range of contradicting results with some researchers suggesting that there are no differences in fracture strength of teeth with CECs and TECs.30-37 Since fractures in ETT are a function of time and multiple chewing cycles, static loading experiments arguably may not be appropriate, as opposed to cyclic fatigue testing; however, one must also keep in mind that such experiments cannot translate directly to clinical settings, especially with the presence of non-modifiable tooth factors. Thus, as clinicians, we need to draw careful inferences from the in vitro literature to apply to clinical practice. Other concerns raised with CEC include compromised canal instrumentation, inadequate debridement of the pulp chamber, preservation of original canal anatomy and increased procedural time. It is important to note that these factors are all process-centered outcomes that have not been directly linked to any improvement in patient-centered outcomes to date. Limitations of in vitro studies also include experiments with small sample sizes, lack of optimum standardizations, lack of replication and use of fully intact teeth under tightly controlled environments which may not always represent clinical situations.
There have been very few studies evaluating the size of canal instrumentation and improved radiographic periapical healing. A systematic review examining apical size of instrumentation concluded that in teeth with apical radiolucency, greater apical enlargement may result in greater radiographic healing;38 it is important to note that one of the included studies forming the basis of this conclusion, only looked at mandibular molars, had a short follow-up period (12 months) and that all treated teeth showed improvement regardless of apical instrumentation size.39 Other factors in that study, including the use of inter-appointment medication and placement of immediate permanent restoration, may have also contributed to the healing. Unfortunately, only four studies met the inclusion criteria for this systematic review, of which only one was a randomized controlled trial. Important limitations of the above studies include case heterogeneity, small sample sizes, multiple confounding factors, unknown use of the microscope, treatments performed by undergraduate students, short-term follow-ups and extracted teeth and loss to follow-up that were excluded from final analysis. The careful clinicians appraising these studies may ask themselves: where are these “loss to follow-up” teeth today? With the understanding of these limitations, can we practice endodontics with true certainty based upon these clinical studies? These studies are considered to represent low levels of evidence and, as such, their impact on clinical procedures needs to be considered with great care.
Immediate Placement of Restorations
The restorative phase plays a critical role in long-term survival of ETT.40,41 Indeed, the immediate placement of a permanent restoration following endodontic treatment allows for optimal sealing and a lower likelihood of interim failure (Fig. 13). The survival rate of ETT is increased when the tooth is restored with a permanent restoration (83 per cent to 91.7 per cent) compared with a temporary restoration (34.5 per cent)15 and when the permanent restoration is placed within a short period of time (two weeks).42 The clinician must also select the appropriate restorative material for the area of placement. Due to its high compressive strength and moisture forgiveness, amalgam is the restorative material of choice for restoring endodontically treated molars with extensive amount of coronal tooth structure loss or with deep sub-gingival caries (Fig. 14). Conversely, composite resin materials can be used in esthetically demanding areas where complete moisture control can be achieved and in situations where minimal tooth structure is lost during preparation. There is also increasing evidence that cementing conservatively placed posts in endodontically treated premolars and anterior teeth may provide reinforcement and decrease the likelihood of “snap-off” failures (Figs. 6 & 15), which in turn may translate to improved tooth survival.43,44 Furthermore, reduction and restorative coverage of thin, weak and unsupported tooth structure may decrease the likelihood of coronal structural failure. Considerations for occlusion also play a critical role in long-term retention of ETT. On posterior teeth, eccentric contacts create interferences that can lead to occlusal trauma which is often associated with fractures. Parafunctional habits like clenching and bruxism may also exacerbate occlusal trauma. Notice in Figure 16B how eccentric interferences were pronounced after the initial occlusal adjustment. This is a common observation and highlights the fact that balancing occlusion is a complicated task and often requires multiple rounds of adjustment.
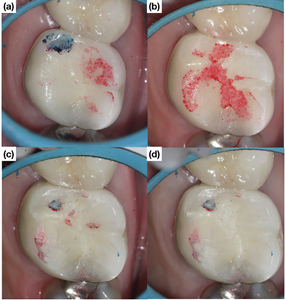
Fig. 13
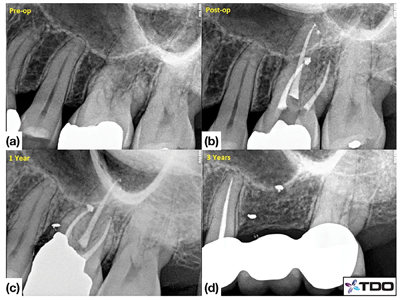
Fig. 14


(d) Matrix band adaptation. (e) Access cavity restored with amalgam. (f-g) A gingival flap is raised in order to restore the deepsub-gingival buccal caries. (h) Post-operative radiograph. (i-j) 1-year follow-up shows healthy gingival contour and radiographic healing.
Fig. 15
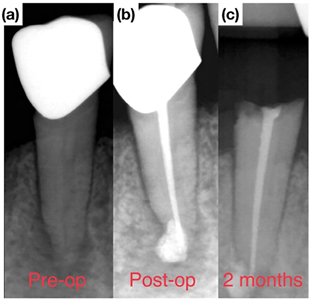
Fig. 16
Conclusion
Contemporary approaches to endodontic treatment are evolving towards improved patient centered-outcomes. Patients demand long-term tooth survival and when coupled with cost vs. effectiveness decisions, the average root canal treatment should at least rival or surpass the supposed long-term survivability of dental implants. Inherently there are many unmodifiable factors that present to a dentist performing endodontic treatment, which make it difficult to make direct comparisons to dental implants. However, the modifiable factors could be considered fully controllable and may play a key role for post-endodontic tooth survivability. No clinician can suddenly adapt to a new method of practice as it disrupts the current clinical workflow, requires tremendous mental debiasing and diligent patience to observe small progression under a cloud of uncertainty. However, arguably, the preservation of residual tooth structure is of paramount importance whether the procedure is basic operative dentistry, endodontic therapy or full-coverage restorations. As clinicians we should also make careful inferences from the literature and realize the inherent flaws especially when translating findings from bench top research to clinical settings.
In conclusion, treatment modalities to maximize longevity of ETT include well-planned conservative access cavities that leverage caries and restorations, conservative root canal preparations and placement of immediate coronal restorations, which include the placement of conservative full coverage restorations when indicated. The adaptation of new concepts and technologies in endodontics including Image Guided Access and Dynamically Guided Access has begun and appears very promising in improving patient-centered outcomes.
Oral Health welcomes this original article.
References
- Sedgley C, Messer H. Are endodontically treated teeth more brittle? J Endod [Internet]. 1992;18(7):332–5. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=1402595.
- Ørstavik D, Pitt Ford TR. Epidemiology of apical periodontitis. In: Essential endodontology : prevention and treatment of apical periodontitis. 1998.
- de Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S, et al. Treatment Outcome in Endodontics: The Toronto Study-Phase 4: Initial Treatment. J Endod. 2008.
- Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health. Int Endod J. 2011.
- Mohamed A, Steier L. Uncertain Decision-Making in Primary Root Canal Treatment. J Evid Based Dent Pract. 2017;17(3):205–15.
- Khatami S, Mac Entee, Michael I; Pratt DCJ. Evolution of clinical reasoning in dental education. J Dent Educ. 2011.
- Higgs J, Jones M, Loftus S, Christensen N. Clinical reasoning in the health professions. Elsevier Health Sciences. 2008.
- Apelian N, Vergnes J-N, Bedos C. Humanizing clinical dentistry through a person-centred model. Int J Whole Pers Care. 2014.
- Newsome PRH, Wright GH. Patient Management: A review of patient satisfaction: 2. Dental patient satisfaction: an appraisal of recent literature. Br Dent J. 1999.
- Bardes CL. Defining “Patient-Centered Medicine.” N Engl J Med. 2012.
- Azarpazhooh A, Dao T, Ungar WJ, Da Costa J, Figueiredo R, Krahn M, et al. Patients’ values related to treatment options for teeth with apical periodontitis. J Endod. 2016.
- Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: Part 2: Tooth survival. Int Endod J. 2011.
- Landys Borén D, Jonasson P, Kvist T. Long-term survival of endodontically treated teeth at a public dental specialist clinic. J Endod. 2015;41(2):176–81.
- Stavropoulou AF, Koidis PT. A systematic review of single crowns on endodontically treated teeth. Journal of Dentistry. 2007.
- Lynch CD, Burke FM, Ní Ríordáin R, Hannigan A. The influence of coronal restoration type on the survival of endodontically treated teeth. Eur J Prosthodont Restor Dent. 2004.
- Petersson K, Fransson H, Wolf E, Håkansson J. Twenty-year follow-up of root filled teeth in a Swedish population receiving high-cost dental care. Int Endod J. 2016.
- Vire D. Failure of endodontically treated teeth: classification and evaluation. J Endod. 1991.
- Prati C, Pirani C, Zamparini F, Gatto MR, Gandolfi MG. A 20-year historical prospective cohort study of root canal treatments. A Multi-
level analysis. International Endodontic Journal. 2018. - Yu VSH, Messer HH, Yee R, Shen L. Incidence and Impact of Painful Exacerbations in a Cohort with Post-treatment Persistent Endodontic Lesions. J Endod. 2012.
- Carr GB. Microscopes in endodontics. J Calif Dent Assoc. 1992.
- Clark D, Khademi J. Modern Molar Endodontic Access and Directed Dentin Conservation. Dental Clinics of North America. 2010.
- Clark D, Khademi J, Herbranson E. The new science of strong endo teeth. Dent Today. 2013.
- Brief J, Edinger D, Hassfeld S, Eggers G. Accuracy of image-guided implantology. Clin Oral Implants Res. 2005.
- Buchanan LS. Dynamic CT-Guided Endodontic Access Procedures. 2018;(January).
- Anderson J, Wealleans J, Ray J. Endodontic applications of 3D printing. International Endodontic Journal. 2018.
- Schilder H. Cleaning and Shaping the Root Canal. Dent Clin North Am. 1974.
- Tang W, Wu Y, Smales RJ. Identifying and Reducing Risks for Potential Fractures in Endodontically Treated Teeth. Journal of Endodontics. 2010.
- Krishan R, Paqué F, Ossareh A, Kishen A, Dao T, Friedman S. Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars. J Endod. 2014.
- Moore B, Verdelis K, Kishen A, Dao T, Friedman S. Impacts of Contracted Endodontic Cavities on Instrumentation Efficacy and Biomechanical Responses in Maxillary Molars. J Endod [Internet]. 2016;42(12):1779–83. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0099239916305817
- Rover G, Belladonna FG, Bortoluzzi EA, De-Deus G, Silva EJNL, Teixeira CS. Influence of Access Cavity Design on Root Canal Detection, Instrumentation Efficacy, and Fracture Resistance Assessed in Maxillary Molars. J Endod. 2017.
- Plotino G, Grande NM, Isufi A, Ioppolo P, Pedullà E, Bedini R, et al. Fracture Strength of Endodontically Treated Teeth with Different Access Cavity Designs. J Endod. 2017.
- Özyürek T, Ülker Ö, Demiryürek EÖ, Yılmaz F. The Effects of Endodontic Access Cavity Preparation Design on the Fracture Strength of Endodontically Treated Teeth: Traditional Versus Conservative Preparation. J Endod. 2018.
- Ivanoff CS, Marchesan MA, Andonov B, Hottel TL, Dandarov Y, Mandova S, et al. Fracture resistance of mandibular premolars with contracted or traditional endodontic access cavities and class II temporary composite restorations. ENDO-ENDODONTIC Pract TODAY. 2017.
- Chlup Z, Žižka R, Kania J, Pˇr ibyl M. Fracture behaviour of teeth with conventional and mini-invasive access cavity designs. J Eur Ceram Soc. 2017.
- Silva EJNL, Rover G, Belladonna FG, De-Deus G, da Silveira Teixeira C, da Silva Fidalgo TK. Impact of contracted endodontic cavities on fracture resistance of endodontically treated teeth: a systematic review of in vitro studies. Clinical Oral Investigations. 2018.
- Corsentino G, Pedullà E, Castelli L, Liguori M, Spicciarelli V, Martignoni M, et al. Influence of Access Cavity Preparation and Remaining Tooth Substance on Fracture Strength of Endodontically Treated Teeth. Journal of Endodontics. 2018.
- Sabeti M, Kazem M, Dianat O, Bahrololumi N, Beglou A, Rahimipour K, et al. Impact of Access Cavity Design and Root Canal Taper on Fracture Resistance of Endodontically Treated Teeth: An Ex Vivo Investigation. J Endod [Internet]. 2018;44(9):1402–6. Available from: https://doi.org/10.1016/j.joen.2018.05.006
- Aminoshariae A, Kulild J. Master apical file size–smaller or larger: A systematic review of microbial reduction. International Endodontic Journal. 2015.
- Saini HR, Tewari S, Sangwan P, Duhan J, Gupta A. Effect of different apical preparation sizes on outcome of primary endodontic treatment: A randomized controlled trial. J Endod. 2012.
- Aquilino SA, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent. 2002.
- Olcay K, Ataoglu H, Belli S. Evaluation of Related Factors in the Failure of Endodontically Treated Teeth: A Cross-sectional Study. J Endod. 2018.
- Willershausen B, Tekyatan H, Krummenauer F, Briseño Marroquin B. Survival rate of endodontically treated teeth in relation to conservative vs post insertion techniques — a retrospective study. Eur J Med Res. 2005.
- Ferrari M, Vichi A, Fadda GM, Cagidiaco MC, Tay FR, Breschi L, et al. A Randomized Controlled Trial of Endodontically Treated and Restored Premolars. J Dent Res. 2012.
- Ferrari M, Cagidiaco MC, Grandini S, De Sanctis M, Goracci C. Post placement affects survival of endodontically treated premolars.
J Dent Res. 2007. - “Best practices in endodontics: A desk reference” Journal of Conservative Dentistry : JCD vol. 18,6 (2015): 507.
About The Author
 Dr. Nadeau graduated with a DDS degree from Dalhousie University. After practicing as a general dentist in Newfoundland for one year, he enrolled in the 3-year Graduate Endodontics Program at the University of Toronto in 2016. Dr. Nadeau may be contacted at: bobby.nadeau@mail.utoronto.ca.
Dr. Nadeau graduated with a DDS degree from Dalhousie University. After practicing as a general dentist in Newfoundland for one year, he enrolled in the 3-year Graduate Endodontics Program at the University of Toronto in 2016. Dr. Nadeau may be contacted at: bobby.nadeau@mail.utoronto.ca.
 Dr. Dale Jung was raised in Orange County, California. He attended Pomona College in Claremont, California and graduated with a degree in Biology. Following college, Dr. Jung spent two years at the National Institute of Dental and Craniofacial Research in Bethesda, Maryland where he studied human salivary gland development and authored or co-authored a few papers. Dr. Jung then moved back to California to attend UCLA School of Dentistry to pursue a career in dentistry. During his time in dental school, Dr. Jung became interested in the field of endodontics and following dental school, he pursued his interests at New York University College of Dentistry in New York City, New York where he earned his certification in Endodontics.
Dr. Dale Jung was raised in Orange County, California. He attended Pomona College in Claremont, California and graduated with a degree in Biology. Following college, Dr. Jung spent two years at the National Institute of Dental and Craniofacial Research in Bethesda, Maryland where he studied human salivary gland development and authored or co-authored a few papers. Dr. Jung then moved back to California to attend UCLA School of Dentistry to pursue a career in dentistry. During his time in dental school, Dr. Jung became interested in the field of endodontics and following dental school, he pursued his interests at New York University College of Dentistry in New York City, New York where he earned his certification in Endodontics.
 Dr. Viraj Vora graduated from the University of Western Ontario with a DDS and a Master of Science and a Certificate of Specialty in Endodontics from the University of Michigan. Dr. Vora is in full time private practice in Vaughan, ON, limited to microscopic conservative endodontics and restorative dentistry. He may be contacted at viraj@endodonticcentre.ca.
Dr. Viraj Vora graduated from the University of Western Ontario with a DDS and a Master of Science and a Certificate of Specialty in Endodontics from the University of Michigan. Dr. Vora is in full time private practice in Vaughan, ON, limited to microscopic conservative endodontics and restorative dentistry. He may be contacted at viraj@endodonticcentre.ca.
RELATED ARTICLE: Dynamic Navigation For Orthograde And Retrograde Endodontics












