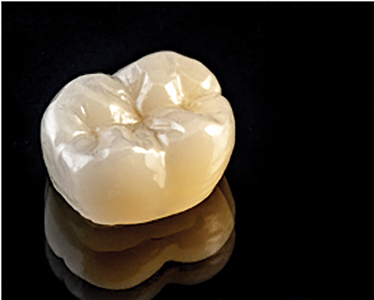
Fixed restorations have come a long way since the early days of cast gold restorations with pyroplast (acrylic) facings. New materials are being developed, techniques simplified, making these advances more economical and user friendly for the dental profession. Beautiful, life-like reproductions of teeth can be created with a variety of different materials such as porcelain fused to metal, lithium disilicate glass-ceramic, polymer glass, porcelain layered onto zirconia, and full contour zirconia (Fig. 1). As well, crowns can be cemented, bonded to natural teeth, and bonded to implant restorations.
Fig. 1

Dental manufacturers have spent millions of dollars in the hopes of persuading you and I that their restorative materials will look and function better than their competitors. There are a number of material options to choose from that will create the right shape, shade and texture and also withstand the stress of the oral environment. Understanding the benefits and limitations to these materials will ensure the correct material is prescribed for each patient’s unique clinical situation.
Porcelain Fused to Metal
Porcelain fused to metal (PFM) restorations has long been the standard in fixed crown and bridge restorations (Fig. 2). Abraham Weinstein developed PFMs in the 1950s as a replacement for high gold alloys with acrylic facings. These newer materials, fraught with design and thermal expansion challenges, were prone to chipping and cracking. The firing of the metal substructure produces the dark oxides integral to bonding porcelain to metal. The necessity to opaque out these dark oxides resulted in PFMs lacking the deep translucency found in most natural teeth.1
Fig. 2

Over several decades, these materials improved immensely. Smaller glass particle sizes in newer porcelains gave it a smoother finish, which proved less abrasive to the opposing dentition. The range of shades widened for improved aesthetics. Finally, our ability to reliably bond porcelain to a greater variety of dental alloy combinations was instrumental in PFM becoming the standard for all other materials to meet and exceed.
Lithium Disilicate Glass-Ceramic
High leucite-containing ceramics commercially known as Empress 1 (Ivoclar Vivadent AG) were introduced in the late 1980s and were the first pressable ceramic materials. Building on its success, the latest version of these lithium disilicate glass-ceramic materials is familiarly known as IPS e.Max (Fig. 3). These restorations are first formed in wax and a heated lithium disilicate glass-ceramic ingot is pressed into the mould using a specially designed pressing furnace. Today these materials are also available in versions for milled applications. IPS e.Max Press provides the fit, form, and function of a pressed ceramic with maximum aesthetic characteristics, and exceptional flexural strength at over 400 MPa. Due to their high strength, these restorations can be conventionally cemented if the preparation is greater than or equal to 4 mm in height. Alternatively, due to their glass content, they can be adhesively bonded after etching their internal surfaces with hydrofluoric acid gel. This provides maximum flexibility to address individual clinical requirements.2
Fig. 3

Ceramic Restoration.
IPS e.Max Press ingots are available in varying degrees of translucency for maximum versatility (Fig. 4). Ingots come in the High Translucency (HT), created for inlays, onlays and veneers; Low Translucency (LT), which is ideal for creating one-step fully anatomical restorations; Medium Opacity (MO), intended for devitalized, slightly discolored preparations; and High Opacity (HO), for preparations that are non-vital and severely discolored. The LT ingots are available in the nine most popular Vita A-D shades as well as four contemporary bleach shades.2
Fig. 4

IPS e.Max restorations are available in two forms. One can choose full contour that provides high strength and beautiful aesthetics as an alternative to zirconia and porcelain fused to precious metal restorations. For more demanding cases, restorations can be fabricated utilizing the cut-back and build-up technique. Final veneering with IPS e.Max Ceram (Ivoclar Vivadent AG), a proprietary nano-fluorapatite layering ceramic, offers more translucency for greater aesthetics.2 As this layering porcelain fuses to the lithium disilicate core when fired, the chances of separation due to parafunction are limited. Aesthetics, high flexural strength, tremendous reduction in wear to the opposing dentition that’s even kinder than that to natural enamel, and over 15 years of clinical data, make lithium disilicate glass-ceramic restorations a very reliable addition to our restorative dentistry arsenal.3
Polymer Reinforced Glass
Polymer Glass Restorative materials, although not as popular today, are still a material available for fixed restorations. These hybrid materials are a combination of glass particles (78% porcelain filler) suspended in a composite matrix. Originally introduced as belleGlass HP and later rebranded as Premise Indirect (KavoKerr Corporation–USA), it is a laboratory-processed composite restorative material that closely resembles tooth structure in wear and thermal conductivity (Fig. 5).
Fig. 5

Polymer reinforced glass is a mixture of aliphatic and urethane dimethacrylate resins with the smallest, most uniform glass crystals whose particle size averages between 3 to 4 microns. It is the only polymer glass material that is processed in a high heat environment (about 293 degrees Fahrenheit) that releases more free radicals, resulting in a more complete cure (approximately 98% compared to 60%-70% from light curing alone). Processing under high pressure (2 atm or 28 psi) eliminates voids in the material, while processing in a nitrogen dry atmosphere eliminates the oxygen-inhibited layer. Together, the result is a complete conversion of the surface area. Cooling to room temperature results in a much harder, stronger, and durable dental restoration with a higher compressive strength, when compared to typical chair-side, light-cured composites. With a coefficient of thermal expansion closely resembling that of natural teeth, this material is less prone to marginal leakage.4
The advantages of this lab-processed micro-hybrid include excellent surface finish longevity, high strength, low water absorption, excellent colour stability, and very low wear (in-vivo) less then 10 microns per year (an annual wear rate equal or slightly less than natural enamel). Some of the advantages over ceramic restorations are simpler fabrication techniques, margins when finished are impeccable, restorations may be adjusted, modified, refinished, and repaired chair side, restorations and luting cements are the same type of material, and, in addition, this type of restoration is kinder to opposing teeth.
For additional strength, these restorations can be reinforced with Construct Fibers (KavoKerr Corp–USA). This ultra-high strength (tensile strength-3,000MPa, modulus-172GPa), braided weave (two over/two under 50*50 picks/in), polyethylene fiber is cold-gas plasma treated, and is near invisible when embedded in the resin material (Fig. 6).
Fig. 6

Zirconia
For decades, PFM has set the standard for strength, durability, and marginal fit. With the introduction of milled Zirconia, enhanced aesthetics is now an inherent feature.
Zirconia is the dioxide form of the metallic element Zirconium, a member of the titanium family. Zirconia comes in pre-sintered form. Using Computer Aided Design (CAD), we can now virtually design copings, bridge frameworks, and full anatomical crowns. Then, using Computer Aided Milling (CAM), we can mill the pre-sintered zirconia into the shapes of crowns and/or bridges at 125% size. Once sintered in a furnace, Zirconia shrinks to the exact 100% size.5
Zirconia can be used in two different ways: It can be made more aesthetically pleasing by bonding porcelain to the Zirconia, or it can be used in its monolithic form as a Full Contour Zirconia, which is stronger and less likely to chip or fracture.6
Porcelain Layered onto Zirconia
Porcelain layered onto milled zirconia crowns are suitable for both anterior and posterior applications (Fig. 7). In the beginning, like any new material, there were obstacles to overcome. In the early 2000s, in 8% of the cases, the layering porcelain debonded or chipped. That was an unacceptably high percentage. However, with improved control of heating and cooling cycles, stronger adherence to correct framework design for porcelain support, and an improved ceramic layering system, chipping and debonding issues have been reduced to almost the same percentage as that of other materials, including PFM.7
Fig. 7

The milled Zirconia copings are tinted to match the shade of the final restoration. As well, the frames are thin and translucent which ensure a natural appearance. They can also be milled using a more opaque Zirconia material. This opacity is most beneficial in masking out dark colours, such as metal posts, roots that darkened after endodontic therapy, or tetracycline stains. Even though Zirconia is metal based, it is white in colour, and as such it delivers a better aesthetic outcome around tissue areas, compared to PFM.
Some of the advantages of Zirconia restorations are excellent aesthetics and translucency, superior strength, high fracture resistance making it ideal for 4-6 unit bridges, outstanding marginal fit, sixteen shades that match the Vita shade system, and a preparation that is similar to PFM.
One must keep in mind that Zirconia is still a metal, so patients with significant metal allergies should consider getting tested prior to using Zirconia. In addition, when layering Zirconia with porcelain, a more aggressive tooth preparation is required to achieve a satisfactory aesthetic result.
Full Contour Zirconia
The other option for Zirconia is in the form of full contour restorations. The original full contour Zirconia materials were extremely hard and opaque, making it difficult to match the shade and translucency of natural teeth (Fig. 8). However, full Zirconia materials are extremely durable, especially when fabricated to their minimal recommended thicknesses.
Fig. 8

The solution to the limitations of the original Zirconia material was a newer generation product known as Multi-Layered Full Contour Zirconia materials. Multi-layered Zirconia brings beautiful aesthetics to the strength of full contour Zirconia crowns (Fig. 9).
Fig. 9
Adding other elements such as Yttria to the Zirconium
alters the strength and translucency of the restorative material. Zirconia has a strength range of 800-1200 MPA (2-3 times stronger than e.Max). The addition of the Yttria diminishes the strength of the material, but it adds to its translucency.5,8
There are many advantages to Multi-Layered Full Contour Zirconia restorations, other than decreased wear of the opposing dentition and greater translucency compared to traditional Zirconia. Pre-shaded material eliminates white spots typical after clinical adjustments. This material is extremely strong and resistant to fracture and chipping if not reduced past its minimal recommended thicknesses of 0.5mm and feather-edge margin preparations.
It’s important to keep in mind that Zirconia’s physical properties make its surface harder than other materials, and as such will wear the opposing dentition.9 Also, care must be taken not to thin them down below their manufacturer’s recommendations, as this will diminish their strength and result in total fracture failure of the restoration. Another concern with these types of restoration is adhesion, as the internal surfaces are smoother than other materials, not easily roughened with micro-etching, and cannot be chemically etched with hydrofluoric acid, because they are not a glass-based material.
Methods to Improve the Retention of Zirconia-Based Crowns
Zirconia based restorations cannot be acid-etched due to the absence of silica and glass, which makes micro-etching (sandblasting) the preferred surface-roughening method. Although Zirconia restorations can be affixed to tooth structure using resin modified glass ionomer cement, conventional cements, or resin cement, it is very important that the clinician appreciate that clinical success with fixed ceramic restorations is strongly influenced by preparation height, your choice of cementation/bonding system, and the material to which it is bonded to, such as tooth or implant. Dual-cure resin cements are the preferred choice because they have the advantages of marginal seal, good retention, and ideal film thickness, resulting in improved fracture resistance.
Here are some suggested methods to increase the retention of the intaglio surface of Zirconia-based restorations for bonding (Figs. 10A&B).10
Fig. 10A
Fig. 10B

With so many options available to us in fixed restorative materials, it is imperative that the clinician be aware of both the benefits and the drawbacks of each material. Clinicians with an understanding of resin adhesive chemistry, dental material science, biomechanics, preparation design, and occlusion will be able to deliver a restoration that will last for years to come.
Oral Health welcomes this original article.
Disclosure: The author wishes to express that he has no financial interest in any of the products mentioned in this article.
Acknowledgement: The author wishes to gratefully acknowledge the help, support, and guidance of Dr. Stephen Abrams in the writing of this article. He has been inspirational as a mentor in the continued pursuit of excellence in dentistry. The author would like to thank Dr. Paul Alter for his review and suggestions in the editing of this article, as well as Dr. Ron Goodlin for his help with the photography.
References
- Culha, O., Zor, M., Gungor, M.A., Arman, Y., & Toparli, M. (2009). Evaluating the bond strength of opaque material on porcelain fused to metal restorations (PFM) alloys by scratch test method. Materials & Design, 30(8), 3225-3228. http://doi.org/10.1016/j.matdes.2008.12.018.
- Helvey, G. (2010). A History of Dental Ceramics. Compendium, 31(4).
- Alarwali, A.M., Kutty, M.G., Al-Haddad, A.Y., & Gonzalez, M.A.G. (2018). Fracture Resistance of Three Different All-Ceramic Crowns: In Vitro Study. Am J Dent, 31(1), 39-44. PMID: 29630804.
- Kakaboura, A., Rahiotis, C., Zinelis, S., Al-Dhamadi, Y.A., Silikas, N., & Watts, D.C. (2003). In vitro characterization of two laboratory-processed resin composites. Dental Materials, 19(5), 393-398. https://doi.org/10.1016/50109-5641(02)00082-9.
- Braeside Dental. (2017). Zirconia (full Zirconia and porcelain fused to Zirconia). Dental Services. Braeside Dental Centre.
- Preis, V., et al. (2012). In vitro failure and fracture resistance of veneered and full-contour zirconia restorations. Journal of Dentistry, 40(11), 921-928. https://doi.org/10.1016/j.dent.2012.07.010.
- Baldassarri, M., Stappert, C.F.J., Wolff, S., Thompson, V.P., & Zhang, Y. (2012). Residual stresses in porcelain-veneered zirconia prostheses. Dental Materials, 28(8), 873-879. http://doi.org/10.1016/j.denta.2012.04.019.
- Johnasson, C., Kmet, G., Rivera, J., Larsson, C., & Von Steyern, P.V. (2013). Fracture strength of monolithic all-ceramic crowns made of high translucent ytrrium oxide-stabilized zirconium dioxide compared to porcelain-veneered crowns and lithium disilicate crowns. Acta Odontologica Scandinavica, 72(2), 145-153. http://doi.org/10.3109/00016357.2013.822098.
- Miyazaki, T., Nakamura, T., Matsumura, H., Ban, S., & Kobayashi, T. (2013). Current Status of Zirconia Restoration. J Prosthodont Res, 57(4), 236-261. https://doi.org/10.1016/j.jpor.2013.09.001.
- Tanis, M.C., Akay, C., & Karakis, D. (2015). Resin cementation of zirconia ceramics with different bonding agents. Biotechnology, Biotechnological Equipment 29(2), 363-367. https://doi.org/10.1080/13102818.2014.996606.
About the Author
 Ronald Klausz, is the owner of Klausz Dental Laboratories, located in Toronto, Ontario. He has written numerous articles on restorative and implant dentistry, and has lectured in both Canada and the United States. He upholds his family’s traditions of producing advanced, high quality restorations and appliances, while providing unique client relationships and patient care services.
Ronald Klausz, is the owner of Klausz Dental Laboratories, located in Toronto, Ontario. He has written numerous articles on restorative and implant dentistry, and has lectured in both Canada and the United States. He upholds his family’s traditions of producing advanced, high quality restorations and appliances, while providing unique client relationships and patient care services.
RELATED ARTICLE: Marginal Gaps of Porcelain Crowns by Manufacturing Technique: A Literature Survey













