First published in ZMK 2022;38: 183-185
 Worldwide survey on the preferred method of prevention
Worldwide survey on the preferred method of prevention
A clean mouth is not only important for oral health, but also for health in general. With Guided Biofilm Therapy (GBT), EMS has developed a systematic, modular, scientifically proven protocol for oral prophylaxis together with universities, clinicians and the Swiss Dental Academy (SDA). Of the more than 76,000 patients surveyed worldwide, more than 92% are enthusiastic about the GBT method and will recommend it to family and friends.
Due to the high burden of disease, the WHO (World Health Organization) has declared oral diseases, including caries and periodontitis, as a key health problem [1,2]. The World Dental Federation (FDI) also highlights the importance of a healthy mouth for general and systemic health in its „Vision 2030“ [3]. In addition to a healthy lifestyle, the microbial dental plaque (biofilm) must be removed effectively by daily oral hygiene and through regular professional mechanical plaque removal (PMPR) [4,5]. To achieve an effective and gentle PMPR, the dental team should apply modern methods, instruments, and materials [6,7]. Prevention-oriented practices therefore surveyed more than 76,000 patients worldwide through questionnaires to determine the preferred method for professional prophylaxis.
Comparison of methods
Guided Biofilm Therapy (GBT) is based on the classic long-term recall of the Swedish dentist Dr. Per Axelsson [8]. As early as the 1970s, he and his team were able to demonstrate in a large group of patients that no teeth are lost to caries or periodontitis if preventive care is consistently performed well into old age. GBT is a further development of this standardized and systematic concept, using new findings and technologies. The protocol can be adapted to all patient groups and clinical findings according to risk [9,10]. The methods involved in GBT have been documented in numerous scientific studies [11-17]. After mandatory disclosure, the objective of GBT is to achieve the most complete and minimally invasive removal of biofilm possible from all oral surfaces [18]. Disclosure is intended for individual patient motivation and the targeted professional removal of biofilm. The biofilm is removed supra- and subgingivally with AIRFLOW® PLUS Powder (based on erythritol) in a minimally invasive manner using AIR-FLOWING® and PERIOFLOW®. [19]. If necessary, a practically painless piezoceramic ultrasonic instrument (PIEZON® PS NO PAIN Instrument) is used for any residual hard deposits (calculus). In contrast, the „conventional PMPR procedure“ focuses on the removal of hard depo- sits, very often with invasive sonic or hand instruments [19,20]. Subsequently, the tooth surfaces are treated with rotating brushes or silicone cups using abrasive polishing pastes. This polishing abrades superficial tooth substance and leaves polishing paste on the surface [21]. The conventional method does not involve applying a system. The biofilm is usually not disclosed before treatment [22] as removal of the disclosed bio- film would require significantly more time (Chéserex, Switzerland, 2018).
Analysis of the questionnaires
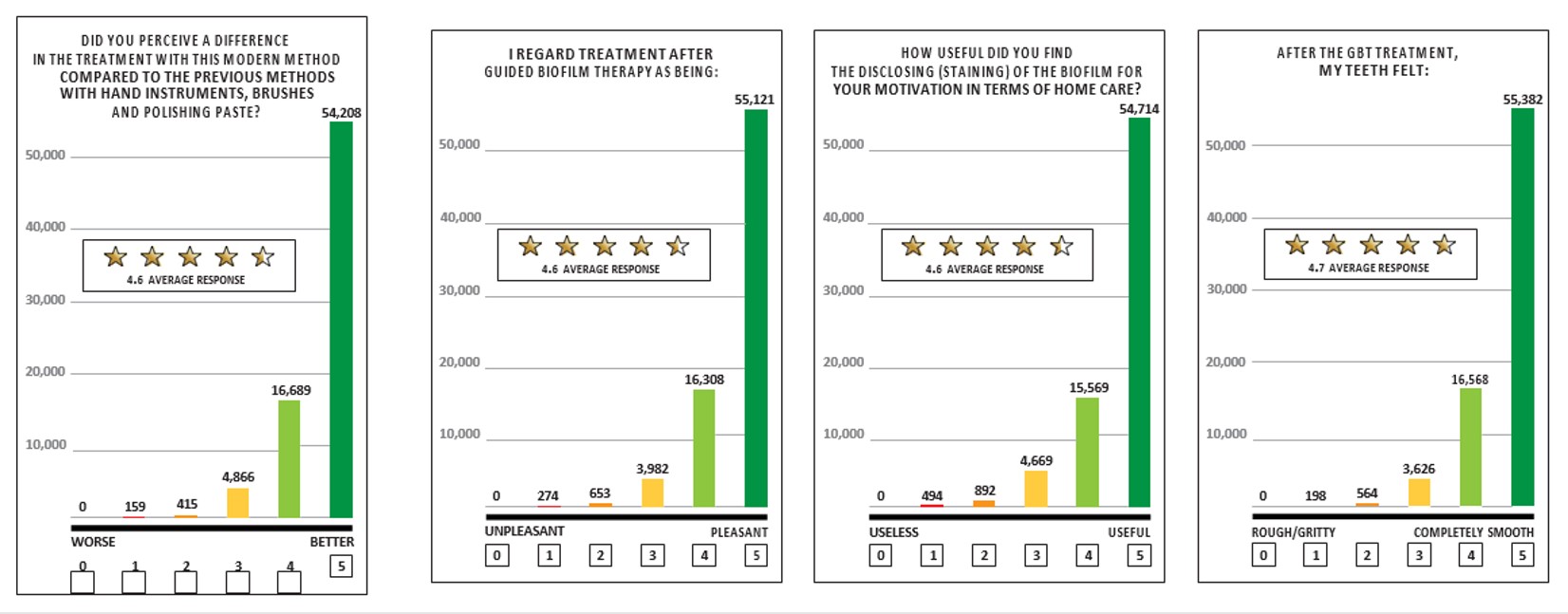
The questionnaires answered by patients (n = 76,338) consisted of 8 questions, including the overall assessment of GBT, the surface smoothness achieved, the usefulness of disclosure before starting the treatment and a direct comparison with the conventional method (diagrams). The anonymized questionnaires were provided to EMS by prevention- oriented practices and clinics. GBT achieved very good results in all the questions illustrated, scoring 4.6 or 4.7 out of a possible 5 points in each case. For the questions about the duration of the treatment and its recommendation, which are not illustrated, the average score was 4.7 out of 5 points.
Over 98% of patients reported experiencing no unpleasant pain during treatment or that the pain was less than with conventional treatment (overall average 4.6).
Discussion and Conclusions
More than 92% of respondents prefer Guided Biofilm Therapy compared to the old method (score 4 or 5 points). This is con- sistent with previously published studies from practice and aca- demia on patient acceptance and satisfaction [6,7,23]. GBT is suitable for both primary preventive PMPR as well as secondary preventive periodontitis and peri-implantitis therapy, depending on the risk and need. Due to its unique scientific documentation and clinical suitability compared to other methods, the concept is recommended by numerous renowned experts [24-26].
The results of the extensive patient survey presented here speak very clearly in favor of Guided Biofilm Therapy compared to con- ventional treatment. To date, no data of this magnitude have been published. Analyses of other surveys conducted among smaller groups of respondents show the same trend as the global survey presented here [7,23].
And finally, it should be noted that the benefits of GBT are not limited to achievable patient satisfaction and the associated high recall adherence rate. As demonstrated in high-level studies, GBT is ergonomically optimized, significantly more effective, at the same time more time-saving and more economical compared to conventional methods [19,27,28,29,30]. It can therefore be implemented particularly efficiently and successfully by the dental prophylaxis team.
Oral Science, your EMS Guided Biofilm Therapy Integration Specialist!
Oral Science is the leading partner for progressive dental professionals who are striving to increase profitability by ensuring superior clinical outcomes and patient experience. It excels in supporting the integration of treatments and technologies that will result in consistent optimal clinical outcomes. Oral Science’s team of Preventive Dental Care Partners and Registered Dental Hygienists is looking forward to supporting your integration of Guided Biofilm Therapy using the AIRFLOW® Prophylaxis Master.
Literature
- Blas E, Kurup Introduction and methods of work. In: World Health Organization: Equity, social determinants and public health programmes. In: World Health Organization (ed). Equity, social determinants and public health programmes, 2010:3-10.
- World Health Political declaration of the third high-level meeting of the General Assembly on the prevention and control of noncommunicable diseases. Report by the Director-General. EXECUTIVE BOARD EB150/7, 150th session 11 January 2022, Provisional agenda item 7. 2022.
- FDI World Dental Vision 2030: Delivering Optimal Oral Health for All. Available from: https://www.fdiworlddental.org/vision2030. 2021.
- Tonetti MS, Chapple ILC, Jepsen S, Sanz Primary and secondary prevention of periodontal and peri-implant diseases. Journal of Clinical Periodontology 2015;42:S1-S4.
- Axelsson P, Nystrom B, Lindhe The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. Journal of clinical periodontology 2004;31:749-757.
- Furrer C, Battig R, Votta I, Bastendorf KD, Schmidlin PR. [Patient acceptance of Guided Biofilm Therapy]. Swiss Dent J 2021;131:229-234.
- Furrer C, Battig R, Votta I, Bastendorf KD, Schmidlin Patientenakzeptanz nach Umstellung auf Guided Biofilm Therapy. Swiss Dent J 2021;131:229-234.
- Axelsson P. [Effect of mechanical control of dental plaque on the development of dental caries, gingivitis and periodontitis. The Karlstad study]. Tandlakartidningen 1976;68:1080-1085.
- Bastendorf K, Strafela-Bastendorf Auf das klinische Protokoll kommt es an – PZR, UPT und GBT. Quintessenz 2020;71:1380-1389.
- Shrivastava D, Natoli V, Srivastava KC, Alzoubi IA, Nagy AI, Hamza MO, et al. Novel Approach to Dental Biofilm Management through Guided Biofilm Therapy (GBT): A Review. Microorganisms 2021;9.
- Vouros I, Antonoglou GN, Anoixiadou S, Kalfas A novel biofilm removal approach (Guided Biofilm Therapy) utilizing erythritol air-polishing and ultrasonic piezo instrumentation: A randomized controlled trial. International journal of dental hygiene 2021;n/a.
- Nascimento GG, Leite FRM, Pennisi PRC, López R, Paranhos Use of air polishing for supra- and subgingival biofilm removal for treatment of residual periodontal pockets and supportive periodontal care: a systematic review. Clinical Oral Investigations 2021;25:779-795.
- Schwarz F, Becker K, Renvert Efficacy of air polishing for the non-surgical treatment of peri-implant diseases: a systematic review. Journal of clinical periodontology 2015;42:951-959.
- Buhler J, Amato M, Weiger R, Walter A systematic review on the patient perception of periodontal treatment using air polishing devices. International journal of dental hygiene 2016;14:4-14.
- Buhler J, Amato M, Weiger R, Walter A systematic review on the effects of air polishing devices on oral tissues. International journal of dental hygiene 2016;14:15-28.
- Barnes CM, Covey D, Watanabe H, Simetich B, Schulte JR, Chen An in vitro comparison of the effects of various air polishing powders on enamel and selected esthetic restorative materials. The Journal of clinical dentistry 2014;25:76-87.
- Petersilka G, Koch R, Vomhof A, Joda T, Harks I, Arweiler N, et al. Retrospective analysis of the long-term effect of subgingival air polishing in supportive periodontal therapy. Journal of Clinical Periodontology 2021;48:263-271.
- Mensi M, Scotti E, Sordillo A, Agosti R, Calza Plaque disclosing agent as a guide for professional biofilm removal: A randomized controlled clinical trial. International journal of dental hygiene 2020;18:285-294.
- Fu JH, Wong LB, Tong HJ, Sim Conventional versus comprehensive dental prophylaxis: comparing the clinical outcomes between rubber cup and air polishing and the importance of plaque disclosure. Quintessence Int 2021;0:0.
- Wennstrom JL, Tomasi C, Bertelle A, Dellasega Full-mouth ultrasonic debridement versus quadrant scaling and root planing as an initial approach in the treatment of chronic periodontitis. Journal of clinical periodontology 2005;32:851-859.
- Arefnia B, Koller M, Wimmer G, Lussi A, Haas M. In Vitro Study of Surface Changes Induced on Enamel and Cementum by Different Scaling and Polishing Techniques. Oral health & preventive dentistry 2021;19:85-92.
- Stiftung Weit aufmachen, bitte. Stiftung Warentest: Professionelle Zahnreinigung. Test 2015:86-90.
- Strafela-Bastendorf N, B. Die Patientenzufriedenheit in der Prophylaxe. Plaque ‚N Care 2020;36:452-456.
- Lang N, A. L, KD. B. Wissenschaftlicher Konsensus Guided Biofilm Therapy-Protokoll. Ein neues Konzept für die primäre und sekundäre Prävention. 2019.
- Sculean A, Bastendorf KD, Becker C, Bush B, Einwag J, Lanoway C, et al. A paradigm shift in mechanical biofilm management? Subgingival air polishing: a new way to improve mechanical biofilm management in the dental Quintessence Int 2013;44:475-477.
- Schwarz F, Becker K, Bastendorf KD, Cardaropoli D, Chatfield C, Dunn I, et Recommendations on the clinical application of air polishing for the management of peri-implant mucositis and peri-implantitis. Quintessence Int 2016;47:293-296.
- Mensi M, Scotti E, Sordillo A, Dale M, Calza S. Clinical evaluation of air polishing with erythritol powder followed by ultrasonic calculus removal versus conventional ultrasonic debridement and rubber cup polishing for the treatment of gingivitis: A split-mouth randomized controlled clinical trial. Inter- national journal of dental hygiene 2021;n/a.
- Park BY, Kim M, Park J, Jeong JH, Noh Research on dental plaque removal methods for efficient oral prophylaxis: With a focus on air polishing and rubber cup polishing. International journal of dental hygiene 2021;19:255-261.
- Donnet M, Fournier M, Schmidlin PR and Lussi A Novel Method to Measure the Powder Con- sumption of Dental Air-Polishing Devices. Appl. Sci. 2021, 11(3), 1101
- Bischoff J „Nebenbei-Prophylaxe“ kann nur der Anfang sein. ZWP 2018; 24:20-22.