Backed by a rapidly growing body of high-quality clinical evidence, Nobel Biocare’s proprietary TiUnite dental implant surface is setting the scientific standard for supporting evidence.
In the 17 years since the launch of TiUnite, the surface has been evaluated in over 465 publications featuring more than 89,500 implants, in over 22,600 patients with a longest mean follow up of 11.2 years.1 The TiUnite surface has been proven to help maintain the implant stability achieved at placement during the critical healing phase2 while enhancing osseointegration3 and anchorage in the surrounding bone compared with machined implants.4,5 TiUnite surface implants can therefore play an important role in helping clinicians meet patient demand for immediate teeth.
Largest ever meta-analysis of a single implant brand
The remarkable efficacy of TiUnite has now been shown in the largest ever meta-analysis assessing a single implant brand. Published in the July/August issue of The International Journal of Oral & Maxillofacial Implants.6 The study by Professor Matthias Karl of Saarland University in Germany and Professor Tomas Albrektsson of the University of Gothenburg in Sweden analyzed results from 106 peer-reviewed publications on prospective clinical studies assessing TiUnite surface implants, featuring 12,804 TiUnite implants and 4,694 patients.
The results confirm that implants with the TiUnite surface have a remarkably low early failure rate and support long-term clinical survival. Early implant- and patient-level survival rates both exceed 99% at one year, and late implant-level survival rate is estimated at 95.1% (91.5% at patient-level) after 10 years.6
Low rates of peri-implantitis, successful soft tissue outcomes with the TiUnite surface
Biological complications were evaluated in 47 of the aforementioned 106 studies. Of these 47 papers, 19 reported cases of peri-implantitis resulting in a prevalence of 5.2% (64/1229 patients). Professors Karl and Albrektsson suggest that, assuming any findings of peri-implantitis in the other examined studies would have been reported by the authors, the actual rate of peri-implantitis among the 4,694 patients in all 106 studies could be as low as 1.36%. This is in line with an earlier report by Albrektsson et al., of 1-2% of well-documented implants at 10 years.7
Successful soft tissue outcomes for TiUnite implants were also reported in a recent study by Drs. Stuart Froum and Ismael Khouly, published in the The International Journal of Periodontics & Restorative Dentistry.8 The results show low rates of peri-implantitis and excellent bone maintenance over 8.5 years for implants featuring the TiUnite surface to the top of the implant, in direct contact with the soft tissue.
The authors observed peri-implantitis only in one case (3.6%) and the reported soft tissue levels—an important factor for implant success—showed a slight gain in interproximal papillae height with no significant changes in probing pocket depth (PPD) or bleeding on probing (BoP) over time. The incidence of mucositis also fell within the range reported by a systematic review of the literature.9 Importantly, the 100% survival rates seen with the TiUnite implants at 1 year were sustained in patients who were available at this 8.5-year follow-up.
TiUnite triggered a reduction in early implant failures
Jemt and colleagues presented an overview of the annual incidence of reported implant failures for patients and operations over a 28-year period at the Brånemark Clinic in Gothenburg, Sweden, between 1986 and 2012.10 During the period 1986–2002, while using machined implants, the authors reported an overall mean incidence of early failures of 11.4% in the maxilla and 4.5% in the mandible. Between 2001 and 2004, the clinic gradually introduced moderately rough surface implants, primarily TiUnite. This coincided with a reduction in the overall mean incidence of early failures to 2.1% for TiUnite and 2.4% for other moderately rough surfaces10 (see Fig.1 below).
Stable marginal bone levels long-term, even in challenging clinical situations
In an investigation by Glauser, 102 TiUnite surface implants were placed predominantly in soft bone and immediately loaded. At 11 years of follow-up, 26 of 38 patients with 66 implants were available for clinical, radiographic and microbiological evaluations.11 The cumulative survival rate was 97.1%, with all three implant failures occurring within the first 6 months. After initial bone remodeling during the first year, the mean marginal bone remodeling up to the 11-year follow-up was −0.47 mm, indicating stable bone levels over 10 years.11
Hans Geiselhöringer, President, Nobel Biocare said: “The importance of the implant surface in achieving excellent treatment outcomes for patients should not be underestimated, as the ever-growing body of high-quality research on the TiUnite surface proves. For clinicians selecting an implant system to treat their patients, surface properties should be a key consideration. When the clinical research is laid out, TiUnite is the choice every time.
“With soft tissue playing a pivotal role in achieving excellent esthetics and long-term treatment success, patients deserve to receive implants that are proven not only to enhance osseointegration, but to support peri-implant health. Both for hard and soft tissue results, the evidence points to TiUnite.”
The full edition of Science First, Volume 4, Issue 2 – TiUnite, setting the scientific standard. Again., will be available at the Nobel Biocare booth (Hall 9, section D3) at the EAO Congress and will be made available for download from nobelbiocare.com/scientific-evidence. Reprints of the meta-analysis by Professors Karl and Albrektsson in The International Journal of Oral & Maxillofacial Implants will also be available from Nobel Biocare at the event. For more information about the TiUnite surface, including clinical cases and scientific studies, visit nobelbiocare.com/TiUnite.
Fig.1
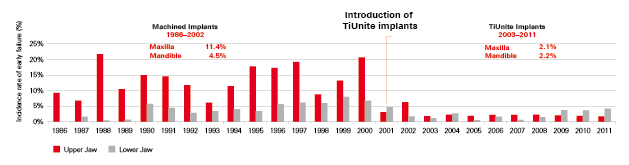
Lower incidence of early failures upon the introduction of moderately rough surfaces, primarily TiUnite surface implants, was significant in both jaws (p<0.05).
Fig. 2
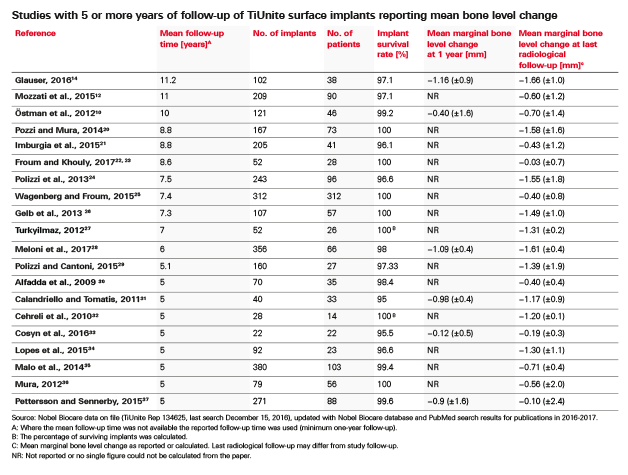
Studies with 5 or more years of follow-up of TiUnite surface implants reporting mean bone level change.
References
- TiUnite literature search, Nobel Biocare Services AG, July 2017
- Glauser R, Portmann M, Ruhstaller P, et al. Stability measurements of immediately loaded machined and oxidized implants in the posterior maxilla. A comparative clinical study using resonance frequency analysis. Appl Osseointegrat Res 2001;2:27–29.
- Ivanoff CJ, Widmark G, Johansson C, Wennerberg A. Histologic evaluation of bone response to oxidized and turned titanium micro-implants in human jawbone. Int J Oral Maxillofac Implants 2003; 18:341-8
- Albrektsson T, Johansson C, Lundgren A-K, et al. Experimental studies on oxidized implants. A histomorphometrical and biomechanical analysis. Appl Osseointegrat Research 2000;1(1):21–24.
- Omar OM, Lenneras ME, Suska F, et al. The correlation between gene expression of proinflammatory markers and bone formation during osseointegration with titanium implants. Biomaterials 2011;32(2):374–386.
- Karl M and Albrektsson T. Clinical performance of dental implants with a moderately rough (TiUnite) surface: A meta-analysis of prospective clinical studies, Int J Oral Maxillofac Implants. 2017;32(4):717-734.
- Albrektsson T, Canullo L, Cochran D, De Bruyn H. “Peri-Implantitis”: a Complication of a foreign body or a man-made “disease”. Facts and fiction. Clin Implant Dent Relat Res. 2016;18(4):840-849.
- Froum SJ, Khouly I. Survival rates and bone and soft tissue level changes around one-piece dental implants placed with a flapless or flap protocol: 8.5-year results. Int J Periodontics Restorative Dent. 2017;37:326–337.
- Tomasi C, Derks J. Clinical research of peri-implant diseases – quality of reporting, case definitions and methods to study incidence, prevalence and risk factors of peri-implant diseases. J Periodontol 2012;39(Suppl 12):207-223.
- Jemt T, Olsson M, Franke Stenport V. Incidence of first implant failure: a retroprospective study of 27 years of implant operations at one specialist clinic. Clin Implant Dent Relat Res 2015;17(Suppl 2):e501–e510.
- Glauser R. Implants with an oxidized surface placed predominately in soft bone quality and subjected to immediate occlusal loading: results from an 11-year clinical follow-up. Clin Implant Dent Relat Res 2016;18(3):429–438.
Nobel Biocare
Nobel Biocare is a world leader in the field of innovative implant-based dental restorations. The company’s portfolio offers solutions from single tooth to fully edentulous indications with dental implant systems (including key brands NobelActive®, NobelParallel®, Brånemark System® and NobelReplace®), a comprehensive range of high-precision individualized prosthetics and CAD/CAM systems (NobelProcera®), treatment planning and guided surgery solutions (NobelClinician® and NobelGuide®) and biomaterials (creos™). Nobel Biocare supports its customers through all phases of professional development, offering world-class training and education along with practice support and patient information materials. The company is headquartered in Zurich, Switzerland. Production takes place at five sites located in the United States, Sweden, Japan and Israel. Products and services are available in over 80 countries through subsidiaries and distributors.












