
Trauma to teeth and the dentoalveolar process may result in a ridge defect that preclude straightforward implant therapy of the patient. After tooth loss, bone resorption is irreversible, leaving the area without adequate bone volume for successful implant treatment.1 Ridge defects may also present after periodontal or endodontic infection or associated to congenitally missing teeth. Bone grafting is the only solution to reverse dental bone loss and is a well-accepted procedure required in one in every four dental implants. Typically bone and soft tissue augmentation of the area would first be needed to adequately prepare the tissues for the implant and its restoration. Grafting of the site is substantially more difficult in cases where the ridge also lacks adequate height, and techniques to recreate a bony envelope to apply guided bone regeneration may be required. Moreover, defects in the anterior aesthetic zone that require both bone and soft tissue grafting and a restoration that harmonizes the adjacent pink and white aesthetics may be an even more significant challenge to the restorative team. Autogenous material obtained from the same individual is always considered the gold standard because of its high osteogenic, osteoinductive, and osteoconductive potential.
Autogenous grafts, which are derived from the same individual, can retain the viability of cells, mainly the osteoblasts and osteoprogenitor stem cells, and they do not lead to an immunologic response, which is known as the gold standard for bone grafts. Tooth loss is accompanied by a series of adaptive changes, leading to dimensional alterations of the alveolar process. During the first year after tooth extraction, Schropp et al. described 50% bone loss in the buccal-lingual dimension, with 30% of the initial ridge width lost during the first 3 months. In addition, this dimension reduction of the jaws also affects vertically.5 Over time, these resulting ridge deficiencies may limit proper dental implant placement. In every regenerative procedure, it is mandatory to accomplish four major principles that Wang et al. described as PASS and allow a more predictable GBR: primary closure to facilitate a protected environment from microbiota and mechanical forces, angiogenesis to promote de novo bone formation, space to assure the different compartments and avoid the collapse of the biomaterial, and stability of the blood clot. These requirements enable better results and reduce the incidence of possible adverse effects. Within the wide range of different augmentation procedures, guided bone regeneration (GBR) and the use of autogenous bone blocks are the most common interventions in bone augmentation; Khoury et al. described the stabilization of two split autologous bone blocks by microscrews and filling the generated gap with autogenous bone chips. These split bone blocks are obtained, either from the mandibular symphysis or ramus, using piezoelectric surgery or microsaws, obtaining a block that will later be divided into the two final thin laminae.
Among the great variety of different GBR procedures for horizontal bone augmentation, Urban et al. described the utilization of a 1:1 mixture of autogenous and xenogenic graft material, covered by a resorbable collagen membrane that is stabilized by titanium pins. Autogenous bone grafting has several advantages over other augmentation techniques including short healing times, favourable bone quality, lower material costs, no risk of disease transmission or antigenicity, and predictability in the repair of larger defects or greater atrophy. Autogenous bone also is a great solution when guided bone regeneration with the use of particulate bone substitutes such as allograft or xenograft failed to regenerate quality bone. The GBR with bone substitutes such as allogenic or xenogeneic materials and application of biologic barriers such as collagen membranes seem to be the dominant technique for bone regeneration by dentists in North America, however, the pure autogenous bone techniques as described by Khoury seems to receive less advocation. French et al have shown, implants requiring GBR are more likely to fail compared to implants placed in the native bone.10 This is supported by Carcuac et al, which described that the patterns in bone loss around implants placed in pristine or grafted bone are different. In contrast, a meta-analysis by Salvi et al, failed to find sufficient evidence to support the above mentioned reports of increased failure rates of implants placed in augmented sites.
This review illustrates some of the complex clinical cases that I have treated in my practice with pure autogenous bone with application of the Khoury technique.
Case I: Vertical and horizontal bone augmentation with Khoury bone shield technique, one of the most effective techniques in ridge bone augmentation using autogenous bone.
A 27 years old male patient with non contributory medical history was referred to our office to replace missing mandibular incisors due to trauma. As it can be seen significant bone deficiency was noted prior to planning for implant placement. Autogenous bone with harvest from mandibular external oblique ridge was used as a box form to reconstruct the bone contour on both buccal and lingual dimensions. Surgical reentry only 4 months later shows significant high quality bone gain in this area that allowed successful implant placement.
Case I
Fig. 1
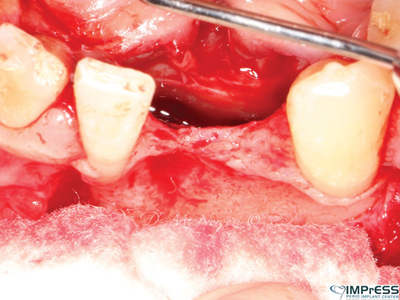
Fig. 2
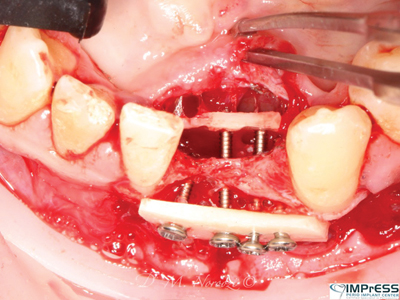
Fig. 3

Fig. 4

Fig. 5
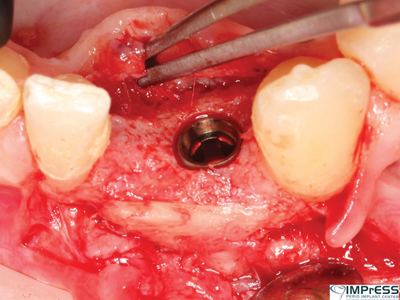
Fig. 6
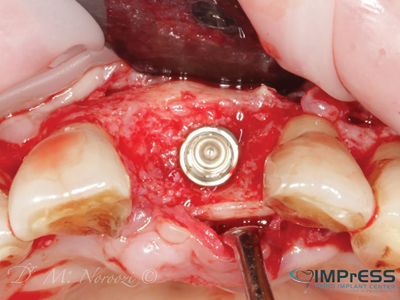
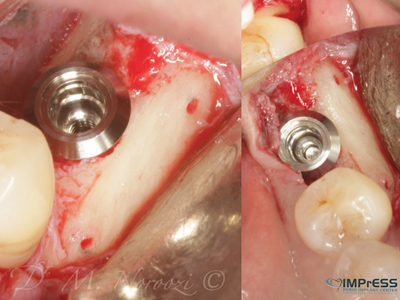
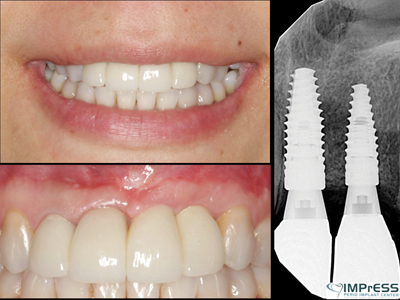
Case II: Significant periodontal infection has led to complete loss of buccal and palatal bone in the area of maxillary central incisor in 45 year old female patient. Autogenous bone from the mandibular ext. oblique ridge was used to reconstruct the horizontal and vertical bone loss for implant therapy. 4 months re-entry shows significant bone gain and successfully integrated implant in the anterior maxilla.
Case II
Fig. 1

Fig. 2
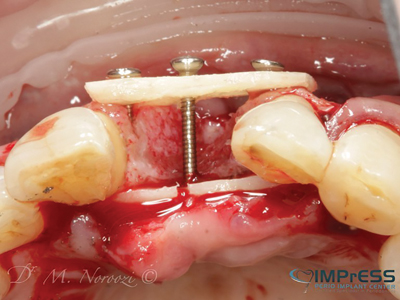
Fig. 3

Fig. 4

Fig. 5

Fig. 6
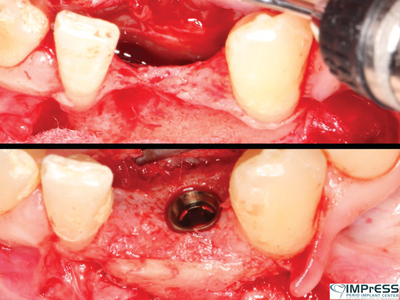
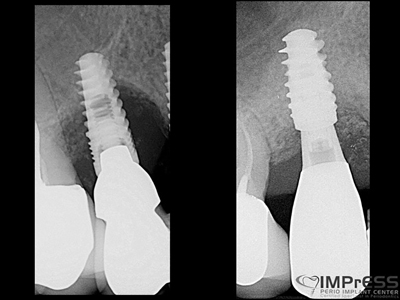
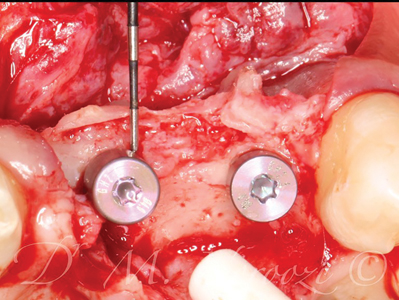
Case III & IV: These cases present the referrals to address implant failures with presence of peri- implant infection, soft tissue defects, severe circumferential bone loss and intrasulcular suppuration.
Implants were removed and the complete loss of the cortical plates was reconstructed with the 3D block graft with Khoury (split bone) technique and autogenous particulates. Five months later, surgical re-entry shows excellent bone quality with complete integration of the cortical bone to the native bone. New implants were surgically placed with excellent primary stability.
Case III
Fig. 1

Fig. 2

Fig. 3

Fig. 4
Case IV
Fig. 1

Fig. 2

Fig. 3
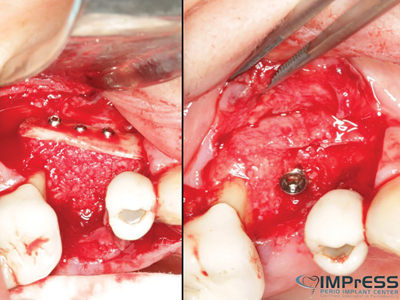
Fig. 4
Case V: 3D bone reconstruction with bone shield technique – Khoury technique with Autograft. A 38 years old male with history of advanced periodontitis was referred to our office to reconstruct the lost alveolar bone in preparation for dental implants in anterior maxilla. Autogenous bone plates harvested from ext oblique ridge was used along with particulate autogenous bone chips from the same site to reconstruct the bone. 5 months re-entry shows complete reconstruction of the bone even the buccal concavity of labial aspect of maxilla.
Case V
Fig. 1

Fig. 2
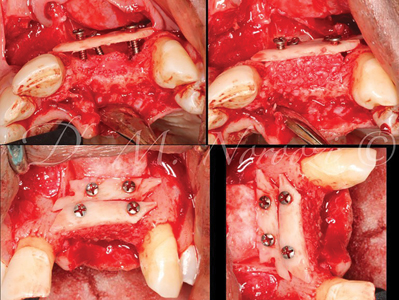
Fig. 3
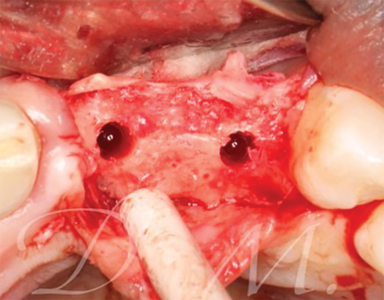
Fig. 4
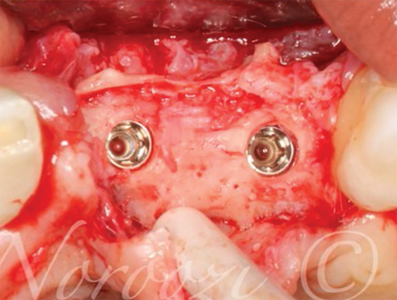
Fig. 5

Fig. 6
Case VI: Pre-orthodontic Bone Augmentation with autogenous bone plates and particulates. This patient was referred to us by our orthodontist to reconstruct the deficiency of bone in the area of congenitally missing second premolars. In order to avoid bone dehiscence, gingival recession and mucogingival defects, adequate bone is preferred so that teeth move within the bone contour. Otherwise there is a high chance of bone loss and gingival recessions once the first premolar and /or molar are moved into the deficient area. CBCT 5 months later showed significant formation of high quality bone with re-establishment of the alveolar bone contour.
Case VI
Fig. 1

Fig. 2

Fig. 3A

Fig. 3B
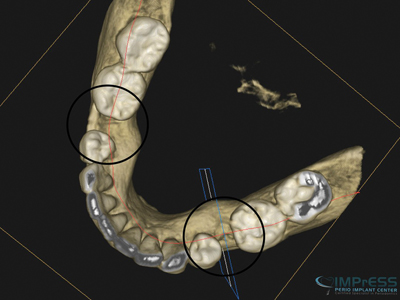
Fig. 3C

Fig. 4

Case VII: Complex 3D bone reconstruction of maxillary anterior region with autogenous bone plates harvested from external oblique ridge of mandible. Bone reconstruction beyond the alveolar bone contour was achieved.
Case VII
Fig. 1
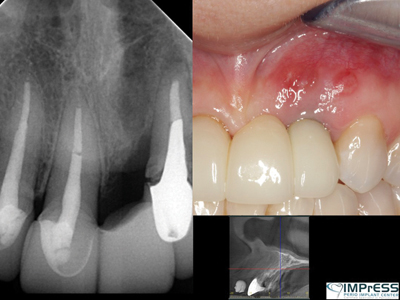
Fig. 2

Fig. 3
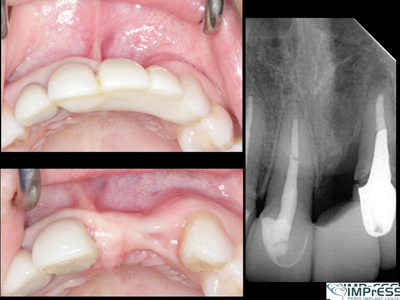
Fig. 4
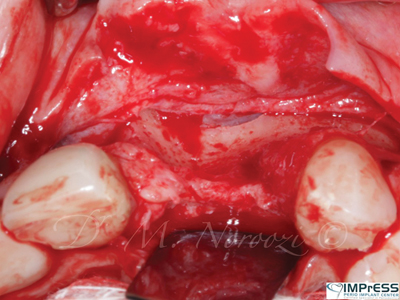
Fig. 5
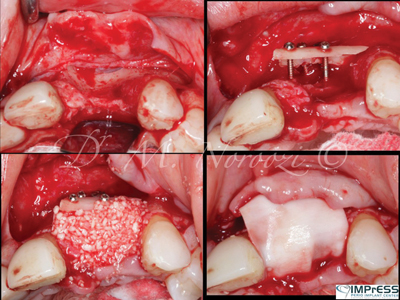
Fig. 6
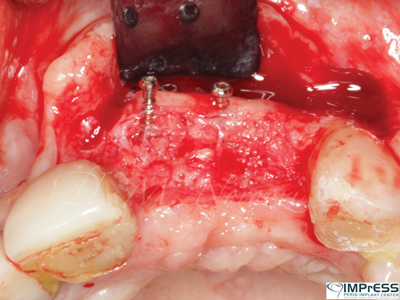
Fig. 7
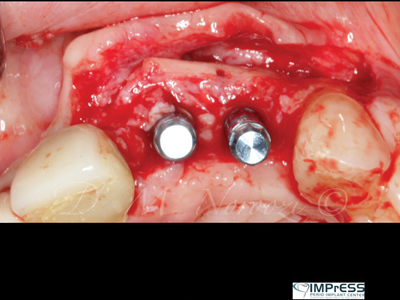
Fig. 8
Oral Health welcomes this original article.
References
- Cawood J.I., Howell R.A. A classification of the edentulous jaws. Int. J. Oral Maxillofac. Surg. 1988;17:232–236. doi: 10.1016/S0901-5027(88)80047-X.
- Tan W.L., Wong T.L., Wong M.C., Lang N.P. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin. Oral Implants Res. 2012;23(Suppl. 5):1–21. doi: 10.1111/j.1600-0501.2011.02375.x.
- Buser D., Sennerby L., De Bruyn H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontology 2000. 2017;73:7–21. doi: 10.1111/prd.12185.
- Liu J., Kerns D.G. Mechanisms of guided bone regeneration: A review. Open Dent. J. 2014;8:56–65. doi: 10.2174/1874210601408010056.
- Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. The International journal of periodontics & restorative dentistry. 08/01/2003;23(4):313-323.
- Wang H.L., Boyapati L. “PASS” principles for predictable bone regeneration. Implant Dent. 2006;15:8–17. doi: 10.1097/01.id.0000204762.39826.0f.
- Khoury F., Hanser T. Mandibular bone block harvesting from the retromolar region: A 10-year prospective clinical study. Int. J. Oral Maxillofac. Implants. 2015;30:688–697. doi: 10.11607/jomi.4117.
- Urban I.A., Lozada J.L., Jovanovic S.A., Nagy K. Horizontal guided bone regeneration in the posterior maxilla using recombinant human platelet-derived growth factor: A case report. Int. J. Periodontics Restor. Dent. 2013;33:421–425. doi: 10.11607/prd.1408.
- Urban I.A., Nagursky H., Lozada J.L., Nagy K. Horizontal ridge augmentation with a collagen membrane and a combination of particulated autogenous bone and anorganic bovine bone-derived mineral: A prospective case series in 25 patients. Int. J. Periodontics Restor. Dent. 2013;33:299–307. doi: 10.11607/prd.1407.
- French D, Ofec R, Levin L. Long term clinical performance of 10 871 dental implants with up to 22 years of follow-up: Acohort study in 4247 patients March 2021Clinical Implant Dentistry and Related Research 23(1) DOI:10.1111/cid.12994 License CC BY 4.0.
- Carcuac O, Abrahamsson I, Derks J, Petzold M, Berglundh T. Spontaneous progression of experimantal peri-implantitits in augmented and pristine bone: A pre-clinical in vivo study. Clin Oral Impl Res. 2020; 31: 192-200. https://doi.org/10.1111/clr.13564
- Salvi GE, Monje A, Tomasi C. Long-term biological complications of dental implants placed either in pristine or in augmented sites, A systematic review and meta-analysis. Clin Oral Impl Res. 2018;29(Suppl. 16):294-310. https://doi.org/10.1111/clr.13123
About the Author

Dr. Mehdi Noroozi is a board-certified periodontist who provides the full scope of surgical periodontal and dental implant therapy.Dr. Noroozi has a special interest in esthetic and reconstructive periodontics and implantology. In addition to private practice, He is a clinical assistant professor in the Department of Periodontics at the University of British Columbia where he is involved in didactic and clinical teaching of periodontics at post-graduate level. Mehdi Noroozi has lectured nationally and internationally and published on various topics related to periodontics and implantology. He can be reached at info@implantperiospecialist.com Private practice, Vancouver, British Columbia.









