Exposure to ionizing radiation and its potential risks are often major concerns of our patients. Ambiguity and confusion exist among the general public, mainly due to the risks discussed in the media and from spurious online information. This leads to confusion, fear, and avoidance by the patient. Therefore, this review aims to attenuate the ambiguity and to provide a clear and evidence-based summary of the current knowledge base for the reader.
As dental professionals, we are aware of the benefits of dental radiography in diagnosis and treatment planning. Therefore, this article aims to arm treatment providers with a thorough understanding of the associated risks and benefits of dental radiography, specifically in regard to an imaging technology that has disrupted dental imaging; 3-dimensional cone beam computed tomography (CBCT).
Radiation 101
Radiation exists in many forms, not all of which are ionizing, the form that poses a risk to human health. Radiation is defined in part by its wavelength. Low frequency radiation, such as radio waves, thermal/microwaves, infrared, and visible light waves are of too low penetrating power to produce changes to the electron balance of atoms and molecules, therefore, classifying these radiation types as non-ionizing. However, higher frequency radiation such as ultraviolet, X-ray, and gamma-rays are able to displace electrons from their orbit around an atom, and therefore have the capacity to cause cellular damage and pose a risk to humans due to their ionizing potential.
Sources of Ionizing Radiation Exposure
We are constantly exposed to radiation in the environment as well as through man-made sources (Table 1). Continuous and ubiquitous exposure to natural background ionizing radiation contributes to roughly half of the annual effective dose in most people. Both cosmic and terrestrial sources contribute to the background radiation experienced. Generally, the other half of ionizing radiation experienced by people per year is by medical imaging, of which dental imaging contributes only a minute percentage of the total exposure from medical imaging. Most medical X-ray exposure derives from computed tomography (CT) scanning of the chest and abdomen. However, it is important to distinguish that although background radiation exposure affects the population relatively uniformly, medical radiation exposure is generally skewed to individuals who are relatively old and/or sick. This should always be considered when discussing sources of ionizing radiation with patients and when weighing the risks and benefits to prescribing dental radiography.
Table 1

Radiation Dose Limits
The Canadian Nuclear Safety Commission (CNSC) is the federal regulator of nuclear facilities and materials in Canada. The CNSC is responsible for setting radiation dose limits in order to protect workers, such as nuclear power workers and medical personnel who work with sources of ionizing radiation from overexposure to those sources. Current Canadian dose limits for exposure to radiation are 50 mSv/year and 1 mSv/year for radiation works and for the general public, respectively. 1 These limits are in line with the guidelines set out by the International Commission on Radiological Protection, 2007.
Dentists, dental hygienists and assistants are considered to be occupationally exposed radiation workers, while other dental office staff (i.e., treatment coordinators) are considered to be members of the public. Recent study of dosimetry records of radiology staff over three years shows received doses of no greater than 1.5 mSv per year. 2 Therefore, with continuous reduction of dental imaging radiation emission and improved best practices, these values are likely even lower in dental workers exposed to radiation today.
There is however, no defined limit to the amount of radiation a patient is able to experience. This is because it is assumed that all ionizing radiation by a medical source is done to directly benefit the patient (i.e., diagnostic imaging, radiation therapy) and the ALARA guideline, supplying As Low As Reasonably Achievable radiation dose is followed. When describing the level of radiation exposure and its anticipated risk to patients, appropriate language should be used and clearly defined in an effort to explain the risk. It is also imperative to obtain informed consent from the patient prior to any exposure to ionizing radiation in a dental setting.
Absorbed dose is the measure of the total kinetic energy released in matter by any type of ionizing radiation (i.e., ultraviolet, X-ray, gamma-ray, etc.). Absorbed dose varies depending on the type and energy of the radiation and the type of matter with which it interacts.
Equivalent dose is a term used to compare the biological effects of the different types of radiation on a tissue/organ. To allow for comparisons among types of radiation, equivalent dose is measured in Sieverts (Sv).
Progressing further, each tissue/organ of the body presents a different sensitivity to radiation and its energy. Therefore, for comparison among tissue types effective dose is used to quantify actual risk to humans. Effective dose considers the biological effects of both different types of radiation as well as different radio-sensitivities of tissue types. Radiosensitive tissues are generally fast-reproducing cells. Some of the most radiosensitive tissue types are blood cells, young cells of the bone marrow, immature reproductive cells, and cells of the intestinal mucosa. Tissues with low radio-sensitivity (i.e, more highly resistant to changes induced by ionizing radiation) include muscle, nerve, mature bone, and the salivary gland, among others.
Mechanism of Action
Ionizing radiation of any kind cause chemical changes to cells that result in biological damage. There are two mechanisms of action that radiation can cause such damage:
Ionization
As an X-ray photon passes through matter, its energy may directly hit and dislodge an electron from its stable orbital position within an atom. This disruption of the atom from its neutral state (creating a positive atom and a negative electron) can cause it to interact with other atoms causing further ionization, excitation or breaking of chemical or molecular bonds. The actual outcome of ionization of an atom by an X-ray photon depends on the molecules it has its effect on (i.e., non-significant cellular structures vs. DNA).
Free Radical Formation
Alternatively, an X-ray photon can have its deleterious effects by interacting with a water molecule to create a free radical/reactive oxygen species (ROS). When an X-ray photon ionizes H2O, breaking it apart into highly unstable and reactive free radicals, the free radicals recombine to cause changes that are capable of widespread cellular effects.
The effects of radiation damage, although additive, are followed closely by cellular repair. While complex, cells have remarkable mechanisms in place to either repair the damage caused by radiation or to undergo apoptosis, programmed cell death, if damage has occurred that is beyond repair.
Several factors influence the likelihood of radiation damage including:
a. Total absorbed dose
b. Dose rate – as mentioned above, radiation damage is additive. Therefore, a greater dose applied over a shorter period of time may increase the likelihood of experiencing radiation damage
c. Amount of tissue irradiated – as discussed below, the smallest field of view (FOV) should always be imaged so as to limit the amount and type of tissue irradiated
d. Cell sensitivity – determination of the FOV and positioning of the patient should always consider the anatomical location of tissues that have high radio-sensitivity, whenever possible
e. Age – younger individuals with immature, developing tissues are at a great risk for radiation damage while older or diseased individuals may have a diminished ability to undergo cellular repair.
Estimating Risk
The primary risk from dental radiography and the overwhelming concern of patients is the chance of developing radiation damage-induced cancer. While the mechanism of action by which the risk of cancer formation is clear, very few studies have been conducted to assess a causal relationship from low-dose diagnostic procedures (i.e., dental radiography). This literature is limited, as the only ethical answer to this question would come from epidemiological data which, would require sample sizes so large that they are impractical. Also, to definitively test this research question, accurate measurements of effective dose would be required, of which there are limited readily available, easy-to-use, or reliable cost-effective methods.
Risk from radiation at low-doses has been estimated with the development of the linear non-threshold (LNT) hypothesis.1 This hypothesis was generated and extrapolated based on data from human epidemiological studies of those exposed to very high levels of radiation (>100 mSv) (i.e., survivors of Hiroshima and Nagasaki atomic bombs, astronauts, and radiation-therapy patients). These observational studies demonstrate a linear response of radiation dose to the probability of developing cancer (Fig. 1). The LNT hypothesis suggests that there is a linear relationship between radiation dose and the risk of spontaneous formation of a new cancer. As this is a linear relationship, this hypothesis suggests that there is no “safe dose” of radiation, below which there is no risk. Rather, it suggests that as exposure increases, so does the likelihood of developing cancer.
Fig. 1

CBCT 101
CBCT has relatively recently been introduced in dental radiography as an adjunct to conventional dental radiography. CBCT provides high spatial resolution and diagnostic reliability often greater than standard 2-dimensional imaging methods. The CBCT does not replace conventional radiography such as a full mouth series for caries and periodontal evaluation. The CBCT is an additional diagnostic tool one can use to gain more information, avoid exploratory surgery (for example in the diagnosis of a cracked root), and it allows you to perform a virtual surgery in some cases increasing patient safety and reducing the risk of complications and ultimately reducing cost for the patient.
CBCT technology works by three basic steps: Acquisition, Reconstruction, and Analysis.
Acquisition
All CBCTs models, regardless of their make, consist of an x-ray source and a detector connected to a gantry which rotates in either 180° or 360° (Fig. 2) around the region of interest (ROI). CBCT technology utilizes the same basic concepts of 2-dimensional radiography, by which the X-ray source produces bursts of photon energies as X-ray beams. As the X-ray beam passes through matter (i.e., human maxillofacial ROI), lower energy X-rays are attenuated while higher energy X-rays pass through to the detector, recording raw 2-dimensional images. One 2-dimensional raw image is captured with every photon burst, creating hundreds to thousands of individual images. These 2-dimensional images are made up of a series of pixels, each of which has its own grayscale value, dependent on the number of photons that reach the detector. Each of the thousands of raw, planar images acquired in sequence appear very similar to individual 2-dimensional cephalometric radiographs.
The acquisition settings of CBCT images can be adjusted to produce optimal quality images for the protocol with the least amount of radiation exposure to the patient possible. Most commercially available CBCT units have specific imaging protocols created and tested by the manufacturer, with the option to adjust at the discretion of the operator. Some exposure settings that can be adjusted to alter the resulting image include: voltage, amperage, resolution, exposure time, rotation step, and FOV size (Table 2). While these settings can be adjusted to improve image quality, they often come at the expense of a higher radiation exposure to the patient. A balance must be struck between acquiring an image of high enough quality for diagnostic purposes and reducing the radiation exposure to the patient. The entire acquisition process takes roughly 15-20 seconds in most commercially available CBCT models.
Even under optimal acquisition setting conditions, image artifacts can still impair CBCT image quality (Fig. 3). An image artifact is any distortion in the image. Image artifacts can be caused by movement of the patient, beam hardening, or X-ray scatter from existing restorations in the FOV. Beam hardening involves a change in the energy of the photon beam as X-rays pass through matter. Low energy X-rays are absorbed first, ultimately decreasing the overall beam energy, but increasing the average energy of the beam as it passes through the FOV. Radiation scatter involves photons being severely defracted from their original path after interaction with very dense matter or material (i.e., dental implants, metallic restorations, etc.).
Table 2

Fig. 2

Fig. 3

To eliminate or reduce image artifacts, it is important to consider:
1. The position of the patient to avoid misalignment of the X-ray source with the ROI
2. Restraint of the head and clear and concise instruction to the patient, including the time for which they are expected to remain completely still. To reduce movement artifacts, some patients may require being set-up for scanning in a seated position, rather than conventional standing position.
3. The size of the FOV, reduced to as small as feasibly possible and adjusted to exclude previously restored areas.
4. Removal of any external metallic objects (i.e., jewellery).
Reconstruction
Following CBCT raw image acquisition, sophisticated software algorithms are applied to the raw data to reconstruct the images along three planes (transverse, sagittal, and coronal) to re-create the 3-dimensional volume (Fig. 4). The spatial resolution of the 3-dimensional image is measured in voxels (3-dimensional pixels).
Analysis and Interpretation
The final step in the method of CBCT imaging involves the analysis and interpretation of the images captured. A great benefit to CBCT imaging is the ability to manipulate, maneuver and reorient the resultant volumetric data set in order to scroll through the “stack” of images created. This drastically improves the ability of dental health professionals to diagnose and in the treatment planning of their patients.
Fig. 4

Responsible Radiation Prescription
While the images acquired through CBCT imaging are powerful, consideration must always be made in regard to the radiation exposure to patients. In accordance with the ALARA concept, there should always be justification for the acquisition of a CBCT image over a standard 2-dimensional radiograph. Generally, CBCT should only be used as an adjunct to periapical and panoramic imaging for diagnosis and treatment planning, and not as a screening tool as there are several advantages and disadvantages to the method itself (Table 3).
Several dosimetry studies have been conducted to examine the effective dose of CBCT technologies in comparison to other CT scanners and to 2-dimensional radiography techniques. In general, the radiation dose to a patient with CBCT is markedly lower than that of multi-slice CT scanners.3-6 A review of the literature revealed an average effective dose of 2.7-24.3 µSv for periapical images, 43.2-200 µSv for digital full-mouth series, and 13-560 µSv for medium sized FOV CBCT.5-8 As described above, several factors including the make and model of the CBCT machine impact the effective radiation dose to the patient. Therefore, only a generalized series of “low-to-high” radiation dose technologies can be described.
Table 3

Common Concerns Surrounding CBCT Technology
A very commonly asked question surrounding CBCT scanning that dental professionals must be ready to educate their patients around is “How much radiation is this going to expose me too?”
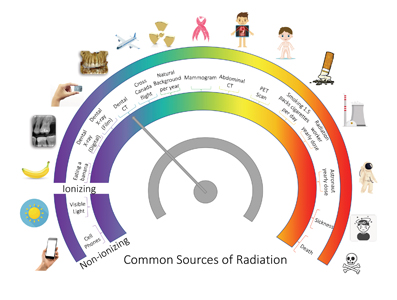
To simplify this highly complex topic and to provide a visual for patients, the simple infographic below can be used as a comparative teaching tool (Fig. 5). When describing effective radiation dose to patients, it is important to underscore the number of nuances that can impact their exposure.
Fig. 5
Similarly, the precautions and considerations taken when deciding to prescribe a CBCT to a patient should be clearly described. Considerations include the justification for requiring the 3-dimensional scan and the risk-to-benefit analysis done in preparation of every scan. Precautions taken that should be described to the patient include: the adjustment of exposure settings, the collimated X-ray beam technology, the size of the FOV acquired, and the external precautions including the use of a lead apron and thyroid collar.
It is also imperative that dental professionals stay up-to-date with recent media releases and publications on the topic of dental imaging and radiation exposure. Patients are exposed to a myriad of complex and ambiguous information sources every day. They rely on dental health professionals to provide them with a clear bottom line when it comes to risks to their health.
Finally, do not dismiss patient concerns around radiation exposure and their perceived risk. Validate their concerns with empathy and understanding. Education of your patients can go a very long way in shifting their perspective on the topic and their acceptance of your offer to do your best work to help them. OH
Oral Health welcomes this original article.
References
- Wrixon AD. New ICRP Recommendations. J Radiol Prot. 2008; 28: 161-168.
- Reddy SS, Rakesh N, Chauhan P, Clint JB, Sharma S. Is dosimetry still a necessity in current dental practice? J Radiol Prot. 2015; 35(4): 911-916.
- Silva MAG, Wolf, U, Heinicke F, Bumann A, Visser H, Hirsch E. Cone-beam computed tomography for routine orthodontic treatment planning: A radiation dose evaluation. Am J Ortho Dentofac Orthop. 2007; 133(5): 640e1-640e5.
- Carrafiello G, Dizonna M, Colli V, Strocchi S, Pozzi Taubert S, Leonardi A, Giorgianni A, Barresi M, Macchi A, Bracchi E, et al. Comparative study of jaws with multislice computed tomography and cone-beam computed tomography. Radiol med. 2010; 115(4): 600-611.
- Loubele M, Bogaerts R, Van Dijck E, Pauwels R, Vanheusden S, Suetens P, Marchal G, Sanderink G, Jacobs R. Comparison between effective radiaiton dose of CBCT and MSCT scanners for dentomaxillofacial applications. European journal of radiology. 2009; 71(3): 461-468.
- Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology. 2008; 106(1): 106-114.
- Lorenzoni DC, Bolognese AM, Garib DG, Guedes FR, Sant’Anna EF. Cone-beam computed tomography and radiographs in dentistry: aspects related to radiation dose. International journal of dentistry. 2012; 2012.
- Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, Cockmartin L, Bosmans H, Jacobs R,
- Bogaerts R, et al. Effective dose range for dental cone bean computed tomography scanners. European journal of radiology. 2010; 81(2): 267-271.
About the Author
 Amanda Longo is the Chief Innovation Officer and Director of Strategy of a world-class periodontal practice in Fonthill, ON. Her role involves strategic innovation of the practice and of the profession itself to ensure the specialty of periodontology is positioned for the patient of today and of tomorrow. Dr. Longo’s doctoral thesis examined the use and safety of micro-computed tomography as a method to quantify the microarchitecture of bone. She investigated the effect of intermittent radiation exposure throughout the lifespan on the quality of bone health.
Amanda Longo is the Chief Innovation Officer and Director of Strategy of a world-class periodontal practice in Fonthill, ON. Her role involves strategic innovation of the practice and of the profession itself to ensure the specialty of periodontology is positioned for the patient of today and of tomorrow. Dr. Longo’s doctoral thesis examined the use and safety of micro-computed tomography as a method to quantify the microarchitecture of bone. She investigated the effect of intermittent radiation exposure throughout the lifespan on the quality of bone health.
 Dr. Fritz is a full-time periodontist in Fonthill, ON and is on a mission to redefine the way people think about periodontal and implant wellness. He leads an extraordinary, collaborative, empowered team of clinicians, makers, scientists and artists who are all working together to innovate the dental specialty of periodontics and redefine the patient experience.
Dr. Fritz is a full-time periodontist in Fonthill, ON and is on a mission to redefine the way people think about periodontal and implant wellness. He leads an extraordinary, collaborative, empowered team of clinicians, makers, scientists and artists who are all working together to innovate the dental specialty of periodontics and redefine the patient experience.
RELATED ARTICLE: When to Take a CBCT Scan for Implant Placement
Follow the Oral Health Group on Facebook, Instagram, Twitter and LinkedIn for the latest updates on news, clinical articles, practice management and more!












