Why Do We Have a Problem?
The apparent epidemic of OSA which is occurring in all industrialized countries should not come as a surprise. Many in the sleep community routinely cite the increase in obesity rates over the last three to four decades as the cause of this epidemic. 1-7 There is no question that obesity is a factor. However, focusing on obesity causes us to ignore a more obvious issue that is a real problem. Our change in lifestyle since the advent of agriculture, and, particularly since the industrial revolution has resulted in changes to the human face. Faces no longer grow forward the way they did prior to our adoption of a Western Diet. Mew 8 describes a hypothetical Paleolithic profile and compares it with two commonly used cephalometric norms (Steiner and McNamara). Both these norms have both the upper and lower jaws substantially recessed from the Paleolithic norm. The Steiner norm is perhaps 6-8 mm. recessed in the maxilla alone. The point is that our faces are substantially further back from where they were a few thousand years ago. With the maxilla back, the soft palate which attaches to it is also recessed. With the mandible back, the tongue which attaches to it is also back. The airway in the region of the soft palate and tongue is the most prone to collapse and closure.
Remmers 9 states that, “A structural narrowing of the pharynx plays a critical role in most, if not all, cases of OSA”. Essentially, he is saying that OSA would not exist if both jaws were forward in the face. The narrower the airway, the faster the air has to flow to get the same volume of air into the lungs. This rapid airflow goes over the curved surface of the tongue and/or soft palate producing a negative pressure (Bernoulli Principle). The smaller the airway, the easier it is for this negative pressure to cause the tongue and/or soft palate to close and completely occlude the airway when the muscles are relaxed during certain sleep stages. The size of the airway is not diagnostic of OSA, but the incidence of OSA is much greater with diminished airway size. 10
Facial Changes from Lifestyle Changes of Agriculture and Industrialization
Weston Price toured the world in the 1930’s and noted a dramatic change in dentofacial structures in populations in the space of one generation. 11 He noted the dramatic increase in dental caries, but also reported on the production of malocclusions in children of parents with normal faces, no malocclusions, and low caries rates. The one common factor in all the societies he studied was adoption of a Western diet with refined flour, sugar, and pasteurized milk.
Catlin 12 had observed essentially the same phenomenon as he described differences between Caucasians vs. Native Americans in the 1830’s. He described the open-mouth posture of the Caucasians vs. the lip-together oral posture of the Native Americans and made a passionate plea for people to keep their lips together and breathe through their noses in his book first published in 1860. His illustrations clearly show the facial changes of both jaws falling back in people whose mouths are constantly open at rest. He further observed big differences in childhood mortality and overall disease rates between Caucasians in the Eastern U.S. compared to the Native Americans in the Western U.S. He described the Native Americans as overall much healthier than the Caucasians.
Pottenger 13 experimented with two groups of cats and fed each group the exact same food. The first group was fed raw meat and unpasteurized milk. The second group was fed cooked meat and pasteurized milk. The cats in the second group were smaller skeletally and within three generations many could not reproduce.
Corrucini14 has spent his career investigating the differences in skeletal structures of humans based on differences in their diets. Studying genetically similar populations in India he noted the more rural groups had better teeth and better developed faces than their urban relatives. He felt the differences were likely diet related with the rural group eating more raw food which required more chewing.
Lieberman’s 15 book, The Evolution of the Human Head, outlines how faces in modern society have fallen back dramatically relative to our ancestors. He speculates the reason is our eating softer, more processed foods relative to our ancestors.
Harvold’s 16 monkey studies showed how facial growth is more vertical (less forward) with alteration in the airway. He plugged the noses of normally growing, nasal breathing monkeys making them obligate mouth breathers. He noted vertical growth changes with longer faces and more recessed jaws. It is hard not to draw parallels between what happened to Harvold’s monkeys and what occurs in growing children living today in industrialized countries.
The changes these investigators have noted clearly result in many people today having faces which have not grown as far forward as those of our ancestors. Therefore, airways are smaller as a result, and the OSA epidemic is not surprising.
Example of Face Falling Back with Growth
The patient in Figures 1A, B and C illustrates how the lower face falls back with altered rest oral posture. The cheeks appear flatter as the maxilla drops back in the face and the mandible also drops back. The soft palate is attached to the maxilla and can be expected to fall back along with the maxilla. The tongue is attached to the mandible and will fall back as the mandible fails to grow forward properly. With minor exceptions one can expect that the airway will be reduced as a result of the maxilla and mandible failing to achieve its genetic potential for forward growth.
Figures 1A, B, C
Fig. 1A, 1B, and 1C show the resuIts of poor rest oral posture with the maxilla and mandible both falling back relative to the Bolton norm superimposed on Glabella and Soft Tissue Nasion. Growth patterns like this are, unfortunately, completely normal in all industrialized countries.

The facial changes illustrated by this example are not unique, but have actually become the norm to one degree or another. The changes occur slowly as growth proceeds so that most parents are unaware anything negative is happening. By the time children graduate from high school many have noses which appear large because the maxilla has fallen back and mandibles are recessed massively from where they should have been had growth proceeded according to the genetic plan.
The impact that such falling back of the face has on the size of the airway has not made it into the mainstream growth and development literature. Orthodontists consider themselves the stewards of growth and development, and yet many articles are published in the journals without showing lateral head X-rays or any concern for the airway. Gelb 17 has brought attention to the importance of the airway and has coined the term “Airway Centric™” to bring attention to the importance of airway in diagnosis for all dental patients.
What is Commonly Recommended for OSA in the Orthodontic Literature?
Low rest tongue posture results in the maxilla narrowing. 8 Orthodontists often notice posterior crossbites and/or crowding of the teeth as reasons to expand the maxilla to correct these problems. More recently an awareness of OSA and a possible role for orthodontics in its treatment has emerged. The most common reaction in the orthodontic community is to expand the maxilla (laterally) as a solution for OSA. 18-20 Indeed, this can help by creating more space for the tongue to be properly positioned upwards in the palate at rest. Expansion of the maxilla laterally can be successful, but results are, by no means, a panacea.
Outcomes of such expansion can be dramatically improved if expansion is followed by myofunctional therapy to train the tongue to be firmly against the palate at rest. Combining expansion and myofunctional therapy can be helpful in eliminating OSA. 21,22
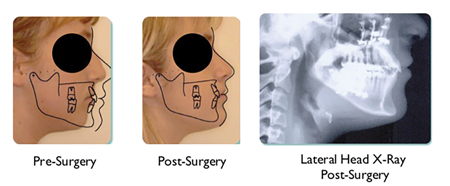
An example of the need for myofunctional therapy is illustrated with the following case. Figures 2A, B and C show the case of male who underwent traditional orthodontics to widen the maxilla as well as maxillomandibular advancement surgery in his mid-teens to open his airway, normalize facial balance, and eliminate his snoring problem. The surgery was a total success. He was told to wear his retainers full time for a year and night time forever. He was also instructed in the importance of adopting proper rest oral posture. Proper rest oral posture means having teeth together lightly, tongue firmly to the palate with the tip at the incisive papilla, and lips together without strain breathing through the nose. This patient did NOT adopt proper rest oral posture and stopped wearing his retainers five years prior to the last picture. The teeth crowded again as the width of the maxilla collapsed dramatically due to his low rest tongue posture. Such a collapse of the maxilla also narrows the nasal airway increasing resistance to airflow affecting his ability to breathe.
Figures 2A, B, C
Fig. 2A: Patient with teeth aligned ready for orthognathic surgery. Fig. 2B: Patient post ortho and orthognathic surgery.
Fig. 2C: Patient after 5 years with no retainer. The maxilla and mandible have narrowed and the incisors are beginning to crowd due to low rest tongue posture.

Lateral expansion of the maxilla even if retained is relatively limited in its ability to solve airway problems since it ignores the fact that both the soft palate and tongue are distalized in the face. Increases in the airway are limited as long as the anteroposterior plane of space is ignored. Lateral expansion should be viewed as a nice start in trying to address the OSA problem.
What Should be the Focus of Orthodontics in Treating the Airway?
Some resolution of sleep apnea may be realized with lateral expansion, but our experience is that much bigger improvements can be achieved working in the anteroposterior plane of space. Remmers9 comments focus on the anteroposterior plane of space. Mew indicates that the very first thing to change in every malocclusion is that the upper anterior teeth fall back from their ideal positions upward and forward. 8 Combining lateral expansion with forward development of the upper and lower jaws appears to give the patient the greatest chance of success in avoiding OSA or eliminating existing OSA.
Orthodontics Traditional Focus on the Anteroposterior Plane of Space
Angle’s classification of malocclusion is focused entirely on the anteroposterior plane of space. One might, therefore, assume that Angle Classification might be very useful in diagnosis and treatment of OSA problems. Nothing could be further from the truth. Reliance on an Angle Classification is to be strongly discouraged. Angle Class I occlusions are supposedly “normal” jaw relationships. Normal, in this case, can often mean “normal” relative to each other, but not to the rest of the face. The teeth can, and often do, fit together nicely with each other, but the teeth exist in a face with both jaws massively recessed to the point that the patient has OSA.
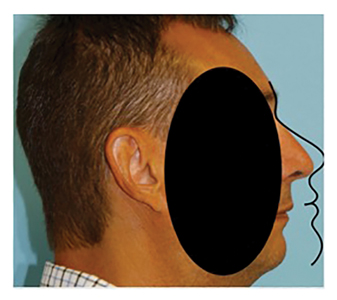
The patient illustrated in Figures 3A, B and C had a perfect Class I occlusion and a very compromised airway. Her chin was forward only because she had a chin implant. Her airway was dramatically reduced with an OSA diagnosis resulting. Her BP (with meds) was 179/121 prior to her undergoing maxilla-mandibular advancement surgery to resolve a severe case of OSA. Her BP 7 weeks after surgery (without meds) was 128/89. She had a Class I occlusion before the surgery and after the surgery. The difference after the surgery was that BOTH JAWS were forward where they were meant to be (and no chin implant was needed).
Figures 3A, B, C
Fig. 3A: Patient with perfect Class I occlusion (with genioplasty) prior to Orthognathic Surgery for OSA Fig. 3B: Post-Orthognathic Surgery for OSA.
Airway in lateral and cross-section view Pre and Post-Orthodontic and Orthognathic Surgery for OSA BP 179/ 121 (with meds) prior to surgery and BP 128/89 (no meds) 7 weeks post surgery.


Angle Class II relationships were studied by McNamara 23 in 1981. The lay public, and most of the dental profession, will view anyone with a Class II malocclusion as having “buck teeth” which essentially implies that the upper teeth protrude in the face. McNamara actually found that the upper teeth in Class II patients were more likely too far back than too far forward. Indeed, he found that maxillary protrusion was relatively rare in Class II patients, and that mandibular retrusion was the most common characteristic. Mew’s 8 assessment, which looks at the lower face in relationship to the nose and/or forehead, actually finds that the maxilla in Class II patients is virtually always too far back. Figures 4A and B show an adolescent male with a Class II Division 1 malocclusion, a very large overjet, and overbite to the palate. The Bolton norm superimposed on Glabella and soft tissue Nasion shows both jaws massively recessed from proper positions in his face. With the maxilla and mandible both recessed in Class II patients it follows that the airway behind both the soft palate and the tongue is reduced in size.
Figures 4A, B
Fig. 4A Adolescent male with Class II deep bite malocclusion and large overjet with both jaws massively recessed from ideal position in face. Fig: 4B Bolton norm superimposed on Glabella and soft tissue Nasion shows maxilla and mandible severely recessed in face. Patients with this degree of lack of forward growth of both jaws is not uncommon in all industrialized societies.

Figures 5A, B and C show a 55-year-old female who had previously undergone surgery to advance only her mandible to correct her Class II malocclusion. Her lateral head X-ray shows an airway with a minimal x-section of 40.8 mm. 2 A PSG confirmed her moderate OSA. The Bolton norm superimposed on Glabella and soft tissue Nasion shows both jaws still substantially recessed from a more ideal position where her airway might naturally be much larger. The point is that her Class II occlusion was treated to a Class I occlusion, but she still suffers from OSA because her mandible was brought forward to meet her recessed maxilla. Had her maxilla and mandible both been advanced her airway would have opened massively increasing the probability of eliminating her OSA. Virtually every Class II patient who undergoes surgery should have both the maxilla and mandible advanced.
Figures 5A, B, C
Patient had previously undergone surgery to advance mandible to correct Class II occlusion. This surgery did not advance the maxilla so the mandible was advanced to a pre-existing recessed maxilla. Fig. 5B: Patient with Bolton norm superimposed on Glabella and soft tissue Nasion shows both maxilla and mandible still severely recessed from ideal positions. Fig. 5C: Airway is completely inadequate (Minimal x-section of 40.8 mm2) and patient still suffers from OSA.

Angle Class III patients are defined as having the lower molars forward of where they would fit with the upper molars with the focus being on the teeth themselves (without reference to the face). Most in dentistry, and even many orthodontists, assume that Class III malocclusions are associated with overgrowth of the mandible. In fact, such is rarely the case. The maxilla is almost always recessed in Class III cases. 24 In addition, even though the mandibular teeth are in front of the maxillary teeth, the mandible is almost always recessed in Class III patients! The airway reduction in such patients can be dramatic. Figure 6 shows a 19-year-old male with a Class III malocclusion with both jaws recessed from an ideal location.
Figure 6
Patient with severe Class Ill malocclusion has both maxilla and mandible massively recessed from Bolton norm superimposed on Glabella and soft tissue Nasion. Class Ill patients rarely have mandibles which protrude in the face. Most Class Ill patients have both jaws recessed from ideal positions.

Figure 7 shows a 56-year-old male who had surgery for a Class III malocclusion approximately 30 years earlier. The surgery performed was a one jaw procedure to set the mandible back. Such treatment was accepted at the time when tongue space and airway were not considered. He came to us because he suffered from OSA. His lateral head X-ray shows his reduced airway which had been made smaller by the previous surgery. He underwent successful double jaw surgery to advance BOTH jaws to eliminate his OSA.
Figure 7
Patient underwent surgery for Class Ill malocclusion to set mandible back 30+ years prior. Lateral head X-ray shows reduced airway as a result of mandibular setback which contributed to OSA.

These examples show that reliance on the Angle Classification of malocclusion is absolutely meaningless and provides us no clue as to what is really happening with either the airway or facial balance. OSA can be present in all Angle Classes and the classification is useless in helping us decide on a treatment regimen to deal with the OSA. Good facial balance is not dependent on any Angle Classification. Treatment must be focused on optimizing both facial balance and the airway no matter the classification. The teeth become secondary in treatment planning.
Tools to Evaluate Jaw Position to Optimize Facial Balance/Airway
Traditional cephalometric analyses have been used in orthodontic diagnosis since the advent of the lateral head X-ray. Virtually all measurements in these analyses focus on hard tissue landmarks of the bony structures and are made on averages of large populations of patients. As such, they are merely describing an average position of jaw structures in patients whose faces have all been adversely affected by growing up in an industrial society as noted above. 11-15 They are absolutely useless in analyzing faces to optimize facial balance since few in our society have optimal facial balance.
There are three simple tools to analyze faces in treatment planning which are useful in achieving better looking faes with larger airways. The first is the Indicator Line as proposed by Mew 8. Figure 8 shows how this is measured. It is a clinical measurement from the tip of the nose to the incisal edge of the upper central incisor. In a growing female, it should ideally be 21 mm plus the patient’s age in years. In a growing male, it should be 23 mm plus the patient’s age in years. In adult patients, the ideal range is 36-40 mm for a female and 38-42 mm for a male.
Figure 8

Figure 9 shows a female with an ideal Indicator Line and a 20 mm airway created by orthognathic surgery. Few people have faces as forward as this patient and 20 mm airways are equally rare.
Mew 8 notes that the very first thing to change in all malocclusions is that the maxillary anterior teeth fall back increasing the Indicator Line measurement. The larger the deviation from the ideal Indicator Line, the less balanced the face and usually the smaller the airway. This is irrespective of classification of malocclusion as noted above. This single measurement can be extremely helpful in screening for possible OSA.
Figure 9
Patient underwent surgery to advance maxilla and mandible. Indicator line measurement ideal for adult female and Bolton norm superimposed on face shows ideal placement of both jaws. Airway is a massive 20 mm.
The second measurement is the Nasolabial Angle illustrated in Figure 10. The range for this number is 90-110 degrees with the ideal being 100 degrees. It is another way to determine the proper position of the maxilla. Faces with Nasolabial Angles larger than 110 degrees become progressively less attractive as the number gets larger. Retractive orthodontics, with or without extractions, can make this number dramatically larger with obvious negative effects on the airway as the number gets larger. Patients with Class II malocclusions and large overjets almost always have Nasolabial Angles on the high side of this range as illustrated by the patient in Figure 11. This is just further evidence that the maxilla in Class II patients is recessed from an ideal position.
Figure 10
 Figure 11
Figure 11
Patient with Class II Division I malocclusion, 10 mm. overjet and 135° Nasolabial Angle showing maxilla severely recessed.

The third measurement tool used in helping us optimize facial balance and airway is the Facial Contour Angle illustrated in Figure 12. The norm is -11 degrees from a straight line. The larger this negative number, the more the mandible is recessed. In general, one can expect that the airway will get progressively smaller as this number gets larger. Figure 13 shows a patient with a facial contour angle of -28o, a small airway, and severe breathing problems.
Figure 12
 Figure 13
Figure 13
Patient has Class II malocclusion with moderate overjet. Facial Contour Angle of -28° indicates severely recessed mandible.

Using the above three guidelines in evaluating faces provides the practitioner easy to use tools to evaluate and plan treatment for optimizing facial balance and airway health. In summary, anything which results in the maxilla and mandible being more forward in the face can be expected to bring both the soft palate (connected to the maxilla) and the tongue (connected to the mandible) forward, thereby, increasing the airway volume and decreasing the probability of collapse during sleep.
Retraction Reducing the Airway
Extraction of teeth with subsequent retraction has been shown to decrease the size of the airway. 25-27 It is critical for dentists to understand the possible effects of ANY form of retraction. The first question we must ask is, “Is it possible to retract enough to produce OSA?” If we accept that it is possible to retract teeth enough to produce OSA logic dictates that we ask the next question which is, “How far can one retract before producing an airway reduction large enough to result in OSA?”
I know of no one who has been able to answer that question. The final question is obvious – “If you do not know where safe retraction becomes unsafe retraction how can you retract at all?” If one accepts the logic of this argument it would seem that traditional orthodontic approaches which retract must be stopped.
Practical Application of Treatment to Optimize Facial Balance and Airway Size in Varying Ages and Situations
It is not the purpose of this article to dictate treatment plans but to outline treatments which have been helpful in optimizing facial balance and airways. An obvious general rule is that treating at the earliest possible time has the best possibility of optimizing facial balance and airway health.
It is also important to remember that nothing which retracts the upper front teeth or restricts the forward growth of the lower face is appropriate at any time. This would include use of headgears which have a goal of restricting maxillary growth. It would also include anything with a headgear effect. All so called “functional appliances” and early treatment preformed appliances can have a headgear effect. 28-30 Class II elastics are routinely used in traditional orthodontics to reduce an overjet in a Class II patient and produce a Class I occlusion. Unfortunately, Class II elastics retract the maxillary anterior teeth and cannot be a part of any treatment concerned with facial balance and airway.
Even closing generalized spacing between the teeth can retract the teeth and reduce the airway. Such space closure must be accomplished in such a way that there is no retraction or reduction in the airway. Figure 14 shows an adolescent where generalized spacing was closed in the anterior but no retraction was done. The generalized spacing was consolidated distal to the second bicuspids where it is not obvious. Such spaces can be left alone or can be closed by over contouring the adjacent teeth with composite resin.
Figure 14
Patient with generalized spacing in upper and lower arches has spacing closed in the anterior without retraction. Spaces have been consolidated between second bicuspid and first molar teeth in all four quadrants. Spaces are large enough to be easily cleaned and are not food traps.

AIRWAY-kening™ Treatment in the Primary Dentition
Gozal 31 indicates that 2-3% of children have OSA, and this number is growing. Harper 32 shows that brain damage can result from even one night of OSA in a young child. Cooper 33 describes the relationship between airway/breathing/OSA issues in African-American children and its impact on many who simply cannot read due to the damage their brains have already endured by the time they enter first grade. Given these facts it is imperative to eliminate the OSA problem as soon as possible. This includes treating patients who have only primary teeth. The patient illustrated in Fig. 15 was five years old and referred to us by a pediatric sleep specialist. The child was diagnosed with Pierre-Robin Sequence, OSA, and Failure to Thrive. We did not promise a result, but outlined Orthotropic® treatment developed by Mew as an effective method of developing both the maxilla and mandible forward.
Figure 15
Patient presents with Pediatric OSA, Pierre-Robin Sequence, and Failure to Thrive.

The maxilla was expanded laterally and anteriorly using a removable appliance (Hang Expancer™). The anterior development was augmented by a reverse pull face mask. The maxillary anterior teeth (as noted by the Indicator Line measurement) were brought forward 7 mm in approximately five months. The mandible was brought forward after the development of the maxilla using a Stage III Biobloc according to the protocol outlined by Mew. 8 Many so called “functional” appliances posture the mandible forward. They also produce a headgear effect which retracts the maxilla because there is nothing to prevent the patient from allowing their mandible to fall back and pull the maxilla back. The Stage III and IV Biobloc appliances used in Orthotropics® as defined by Mew have acrylic extensions to the floor of the mouth which will engage the mandible and make it uncomfortable for the patient to allow the mandible to fall back. Figure 16 shows a Mew Stage III Biobloc appliance. These extensions are adjusted to keep the patient held tightly in an ideal bite position at rest and prevent the patient from putting pressure on the maxilla. By eliminating the headgear effect forward development of both jaws is allowed to occur. Over time the mandible assumes this more forward position and will not fall back. A sleep test done for this patient after the mandible was developed forward showed complete elimination of the OSA problem. The improvement in the airway size is noted in Figure 17.
Figure 16
Mew Stage III Biobloc “postural” appliance with extensions to floor of the mouth. Extensions are adjusted with plastic material to engage the floor of the mouth, prevent the mandible from falling back, and eliminate the “headgear” effect of “functional” appliances.
 Figure 17
Figure 17
Pre and post-treatment airways for patient in Fig. 15. Pre-treatment OSA was eliminated post-Orthotropic® treatment.

The results of a study 34 of consecutively treated Orthotropics® patients has confirmed excellent airway improvements are achievable with both lateral and anteroposterior forward development of both arches. Indeed, a 31% airway increase was noted at the level of the palate, a 23% increase at the base of the tongue, and a 9% increase in the area of the laryngopharynx.
Treatment in the primary dentition has not been commonly done because historically the focus of orthodontics has been on straightening teeth. The focus on teeth must be be changed to a focus on optimizing facial balance and airway development. The teeth must be viewed as a convenient handle to the cranial bones which make up the face. The earlier we treat the better – even in the primary dentition.
AIRWAY-kening™ Treatment in the Early Mixed Dentition
The patient in Figures 18A, B and C began treatment at 8 years of age, when the four permanent maxillary anterior teeth were erupted into the mouth (standard time for Orthotropics®). Her maxillary anterior teeth were advanced 8 mm, while the width of her maxillary arch was dramatically increased to over 40 mm (at the first molars) from a number in the low 30’s. Her mandible was then brought forward with an ADAPT-LGR™ (similar to a Stage IV Biobloc) which has extensions to the floor of the mouth and no headgear effect. By first advancing the maxilla and then advancing the mandible the entire lower face can be brought forward. This enhances both facial balance and optimizes airway development as the soft palate and tongue move forward with the maxilla and mandible. The airway improvement in this case is dramatic as shown in Figure 19. This child’s mother reported that she has more energy, is more outgoing, and is now two grades ahead of her classmates in most subjects. Her mother attributes a good portion of this change to the dramatically improved airway and better sleeping pattern.
Figures 18A, B, C
8y 3m old with deep bite and end-to-end Class II occlusion, maxillary anterior teeth 8 mm. too far down and back in face.
 8y 7m old in middle of Orthotropic® treatment with massive lateral expansion of maxilla, 8 mm. upward and forward advancement of six maxillary anteriors, and lower arch leveled to a near flat occlusal plane as per Orthotropic® protocol.
8y 7m old in middle of Orthotropic® treatment with massive lateral expansion of maxilla, 8 mm. upward and forward advancement of six maxillary anteriors, and lower arch leveled to a near flat occlusal plane as per Orthotropic® protocol.
 10y 3m old patient after Orthotropic® treatment with ADAPT-LGR™ appliance to develop mandible forward and correct poor rest oral posture.
10y 3m old patient after Orthotropic® treatment with ADAPT-LGR™ appliance to develop mandible forward and correct poor rest oral posture.
 Figure 19
Figure 19
Note dramatic profile and airway improvements for patient in Fig. 18A, B, C.
13.1 mm2 minimal X-section (high risk for OSA) becomes 186.1 mm2 minimal X-section (low risk for OSA) after Orthotropics®.

AIRWAY-kening™ Treatment in the Permanent Dentition
The traditional time for wearing braces is generally in the very early teenage years when all the permanent teeth have erupted and can be aligned easily. Unfortunately, the grand majority of facial growth has already occurred and trying to get both the maxilla and mandible to develop further forward is nearly impossible. Johnston 35 compared traditional orthodontics with headgear and braces with “functional” appliances which purported to “grow the mandible” in the 1980’s and concluded that both groups had a “moderate mid-facial dentoalveolar retrusion”. No mention was made in this article that the resulting lack of forward growth of the lower face might impact health through reduced airway increasing the chances of OSA, UARS, or any other airway related problem. Current evidence suggests that there is cause for concern.
Many efforts have been made to develop the mandible forward in children who are still growing and are of the traditional age to wear braces. The Herbst appliance was developed in Germany in the early 1900’s and enjoyed a surge of interest in the U.S. in the early 1980’s. The literature is pretty clear that there is very little forward development of the mandible and a pronounced headgear effect. 28 Many other approaches have been proposed such as the MARA appliance, Forsus, Twin Force Bite Corrector, Jasper Jumper, etc. All can be effective in correcting a Class II malocclusion to a Class I occlusion. However, there does not appear to be dramatic improvement in achieving forward growth of the maxilla and mandible resulting in airway increases.
In a Class II situation involving a teen or adult the treating doctor who wants to optimize facial balance must consider a surgical approach to advance both jaws to more ideal positions in the face. When the discrepancy is severe and OSA is already present this may well be the only effective approach. For many reasons, most orthodontists will try to do anything to avoid subjecting the patient to surgery. The traditional orthodontic approach to avoid surgery is to remove the maxillary right and left first bicuspid teeth and retract the anterior teeth to produce Class I cuspids and ideal incisal guidance. Unfortunately, this treatment approach can have negative consequences on both facial balance and the airway.
There may be an alternative treatment approach for the Class II patient who is not severely retrognathic. The overjet can be reduced by advancing the lower anterior teeth and creating space between the bicuspid teeth (or elsewhere in the lower arch) using a removable appliance. Once the lower anterior teeth are advanced, the posterior teeth can be brought forward and the space closed by using TAD’s as anchorage. The case shown in Figures 20A, B, C and D illustrates this treatment. This patient started treatment at 12 years, 10 months with a sagittal appliance to advance the lower anterior teeth. After approximately seven months of appliance wear the lower anterior teeth were sufficiently anteriorized to reduce the overjet and open the bite. Braces were placed on the teeth for alignment. TAD’s were placed after approximately two years of treatment. Alastic chains from the TAD’s to the molars brought the molars forward. Another 14 months of treatment were required to completely close the spaces. Effectively this treatment brought the entire lower dentition forward on the mandible without changing the position of the mandible itself. The airway improvement resulting from this treatment as well as substantial bone on the labial aspect of the teeth is shown in Figure 21.
Figure 20A, B
Patient in Fig. 20A, B, C, D had 60.2 mm2 minimal X-section (moderate risk for OSA) which became 150.4 mm2 minimal X-section (low risk for OSA) Post Treatment. Note substantial bone on labial aspect of lower incisors Post-Treatment. Incisor advancement did not cause bone loss or recession as orthodontists are taught.
Male patient (13y 5m) in midst of treatment with lower sagittal appliance opening spaces between permanent bicuspid teeth to advance lower anterior teeth.


Male patient (14y 10m) in full braces with TAD’s placed between lower cuspids and first bicuspid teeth. Alastic chains from TAD’s to first molars bring molars forward to close the spaces created by the sagittal appliance.
Male patient (17y 8m) more than a year post-treatment. Entire lower dentition has been moved forward to eliminate overjet. Note no gingival recession.


Figure 21
Patient in Fig. 20A, B, C, D had 60.2 mm2 minimal X-section (moderate risk for OSA) which became 150.4 mm2 minimal X-section (low risk for OSA) Post Treatment. Note substantial bone on labial aspect of lower incisors Post-Treatment. Incisor advancement did not cause bone loss or recession as orthodontists are taught.

Advancing lower anterior teeth in this fashion is NOT considered the Standard of Care in the Community and is generally thought to risk recession and possible loss of lower anterior teeth. This general feeling still is pervasive in the orthodontic community despite a complete absence of published reports of such treatment ever causing problems. It also ignores the refereed literature which confirms that it is NOT a problem to substantially advance lower anterior teeth. 36-42 This treatment approach should be considered as an excellent way to resolve an overjet without retracting the upper anterior teeth when it is too late to develop the entire lower face forward with Orthotropics® or not to be considered because of expected poor patient compliance. This treatment should not be done for patients who have significantly recessed chins.
AIRWAY-kening™ Treatment for Missing Lateral Incisor Teeth in Adolescents
Congenital absence of lateral incisor teeth is certainly not uncommon. Its treatment has been the subject of much controversy for many years. Prior to the advent of implants the focus was largely on closing the missing lateral incisor spaces to avoid preparing virgin teeth for a bridge. Implants changed that discussion when the adjacent teeth no longer needed to be prepared for bridges. There is still a lot of controversy in treating this problem with many still happy to remove the other lateral incisor which often is a peg lateral, and close both spaces. The intimation is that the “cuspid teeth will be brought forward in the face”. Anchorage considerations of the roots of all the teeth involved render that statement almost preposterous. The result of such space closure is almost always significant retraction of the two central incisor teeth with a very unaesthetic increase in the nasolabial angle. The patient in Figure 22 (shown here as an adult) was missing an upper lateral incisor, and had a peg lateral incisor on the contralateral side as an adolescent. The peg lateral incisor was removed as well as the lower second bicuspid teeth and all spaces were closed with retraction. Her Nasolabial Angle is approximately 140 degrees when a number of 100 is considered ideal. It has been shown that such retraction can also change the direction of growth of the lower face in a formerly forward growing face. 43
Figure 22
This patient exhibits severe flattening of the entire maxilla and a very recessed mandible. The Naso labial Angle is 140° ( 100° ideal).

It is particularly tempting for orthodontists to close missing lateral incisor spaces when the patient is Class II. A very common treatment approach for Class II patients with all their permanent teeth is to remove the upper first bicuspids and retract the six anterior teeth to produce Class I cuspids. It is an easy transition from this thinking process to close the missing lateral incisor spaces and retract the centrals. The goal for the orthodontist is to reduce the overjet. Almost always this will be done at the expense of the face and the airway. Figure 23 shows a 55-year-old male whose missing lateral incisor spaces were closed by “canine substitution” when he was an adolescent. The retraction of his teeth resulted in a severe lack of forward development of his entire lower face. The Bolton norm superimposed on his face in Figure 24 illustrates just how far back both jaws are from the norm. He unconsciously tips his forehead back which positions his lower face forward to open his airway. He has OSA and suffered a stroke in his early 50s. Since 65-80% of all stroke patients suffer from OSA, 44 it seems likely that the retraction of his face which occurred with the space closure contributed to his OSA and his stroke.
Figure 23
55y 2m old male treated as child for missing lateral incisors with “canine substitution”.
 Figure 24
Figure 24
Patient in Fig. 23 with Bolton norm superimposed on Glabella and Soft Tissue Nasion. Maxilla and mandible are severely recessed. 35° backward tilt of forehead from vertical (should be vertical) keeps chin forward and maintains airway.
The following case illustrates an alternative to closing the spaces. This 10-year, nine-month old male in Figure 25A and B had a missing upper left lateral and a peg right lateral. He had received another orthodontic opinion to have the peg lateral removed and both lateral spaces closed orthodontically. His Class II bite relationship would have been perfect for that treatment plan if the face and airway were not considerations! One might suggest that the only way to correct the Class II relationship without retracting the upper teeth in some fashion would be surgery to advance the mandible. Certainly, that would have been an option but his chin prominence made this seem very unnecessary. Instead, we advanced his lower anterior teeth dramatically to reduce the overjet using a removable appliance. We opened space between the lower second bicuspid teeth and first permanent molars bilaterally. This space is large enough for an implant. We could have placed TAD’s and brought the molars forward, but it would have added significant treatment time in a case where the patient had very poor oral hygiene. The goal of the treatment was to reduce the overjet by advancing the lower anterior teeth forward rather than by retracting the upper anteriors. The prevailing wisdom in the orthodontic profession is that such an advancement of the teeth would cause recession and possible tooth loss of the lower anterior teeth. We have been advancing lower anterior teeth in this fashion for over thirty years and have not experienced this problem even once. The refereed literature clearly supports such treatment with confirmation that such advancement is not a threat to periodontal health. 36-42
Figure 25A, B
10y 9m old male with missing upper left lateral incisor, undersized maxillary right lateral incisor, and Class II malocclusion with moderate to large overjet. Patient received orthodontic opinion to have maxillary right lateral incisor removed and both lateral incisor spaces closed by retraction of the central incisors (“canine substitution”).
 Orthodontic treatment opened space for the missing upper left lateral incisor and spaced the right lateral incisor for veneering. A temporary bonded bridge replaces the missing lateral incisor until growth is complete and implant placement is accomplished. Massive advancement of ten lower anterior teeth reduced the overjet. Spaces large enough for an extra bicuspid were created between second bicuspids and first molars. Note absolutely no recession on lower anterior teeth despite what orthodontists are taught.
Orthodontic treatment opened space for the missing upper left lateral incisor and spaced the right lateral incisor for veneering. A temporary bonded bridge replaces the missing lateral incisor until growth is complete and implant placement is accomplished. Massive advancement of ten lower anterior teeth reduced the overjet. Spaces large enough for an extra bicuspid were created between second bicuspids and first molars. Note absolutely no recession on lower anterior teeth despite what orthodontists are taught.

The retraction of the central incisors in missing lateral incisor cases cannot be justified for facial esthetic reasons or for the possible airway reduction which may accompany this treatment. Instead, space must be opened whenever there is a missing lateral incisor so that a suitable replacement can be placed.
AIRWAY-kening™ Treatment for Adult Class II –Nonsurgical Correction
Figures 26A, B and C show a 38-year-old male who had undergone four years of retractive orthodontics in which minor lower anterior spacing and been closed and spacing had been left in the maxilla for replacement of missing teeth. The restorative dentist was unhappy with the way the teeth fit and referred the patient for further treatment. At this point, the patient was a snorer and suffered from OSA. A surgical approach to advance both jaws was considered but rejected by the patient. A compromise treatment to advance the entire lower anterior segment of teeth was selected. First, ideal spacing of the upper anterior teeth for implants created an overjet. The overjet was corrected by advancing the lower anterior teeth with a sagittal appliance. Within a few weeks of wearing the sagittal appliance the patient’s wife reported his snoring had ceased completely. The final advancement of the lower anterior teeth resulted in enough space for an extra bicuspid tooth on each side of the lower arch.
Figures 26A, B, C
38m yo male underwent orthodontics which closed lower anterior spacing in preparation for replacing missing maxillary teeth. He snored and suffered from OSA.
 Revisionary orthodontic treatment reopened lower incisor spacing. Maxillary spaces were better idealized for restorative. Spaces for “extra” bicuspid teeth implants were created between lower cuspids and first bicuspids reducing the Class II overjet. Snoring and apparent OSA eliminated.
Revisionary orthodontic treatment reopened lower incisor spacing. Maxillary spaces were better idealized for restorative. Spaces for “extra” bicuspid teeth implants were created between lower cuspids and first bicuspids reducing the Class II overjet. Snoring and apparent OSA eliminated.
 Despite massive advancement of lower anteriors for patient in Fig. 26A, B there is no recession.
Despite massive advancement of lower anteriors for patient in Fig. 26A, B there is no recession.

Despite the generally held warning in the orthodontic profession that such advancement of lower anterior teeth might cause recession and ultimate tooth loss there is no hint of loss of attachment of the tissue as noted in Figure 26C.
AIRWAY-kening™ Treatment by Adding Extra Bicuspid Teeth
Adding teeth where none are missing may seem a radical thing to do. The patient shown in Figures 27A-E suffered several migraines per week and reportedly lost two to three weekends a month being incapacitated with migraines. Nothing she had done to address this nearly 20-year problem had been successful. We noted her tender TMJ’s, tender facial and cervical muscles, etc., and also recognized that her upper and lower teeth appeared tipped back in her face. Without promising her resolution of any symptoms, we suggested that we open spaces in both arches to give her more tongue space. As the treatment progressed she became happier and happier with the cessation of symptoms and the esthetic appearance of a fuller profile. Her migraine pattern was entirely eliminated and has not returned. We created enough space so that an extra bicuspid tooth in each quadrant was added. Implants were placed in the sites and ultimately restored with porcelain crowns. She states that she sleeps well and awakes well rested since the treatment. Her headache pattern was completely eliminated as her tongue space/airway was increased. Her broader smile with no gumminess was a nice side benefit of the elimination of her pain pattern.
Figures 27A, B, C, D, E
Migraine suffering patient who never had orthodontic treatment.
 Patient after orthodontic treatment to open space for “extra” bicuspid teeth between upper bicuspids and between lower cuspids and first bicuspids. Substantial lateral expansion of both arches was also accomplished. Migraine pattern was completely eliminated.
Patient after orthodontic treatment to open space for “extra” bicuspid teeth between upper bicuspids and between lower cuspids and first bicuspids. Substantial lateral expansion of both arches was also accomplished. Migraine pattern was completely eliminated.
 Patient after restoration of “extra” bicuspid teeth in each quadrant.
Patient after restoration of “extra” bicuspid teeth in each quadrant.
 No recession in lower anterior despite massive advancement of anterior teeth.
No recession in lower anterior despite massive advancement of anterior teeth.
 Pre and Post-Treatment smiles.
Pre and Post-Treatment smiles.

AIRWAY-kening™ Treatment by Reopening Extraction Spaces
The patient shown in Figures 28A and B suffered from severe TMJ/Pain and had undergone arthroscopic surgery to the TMJ’s more than a decade before we examined her. The pain pattern was not a current problem but she suffered from moderate OSA and typically slept about two hours a night. Tomograms confirmed both TMJ’s were undergoing severe degenerative changes, but were asymptomatic at the time. Since both jaws were massively recessed, orthognathic surgery was the obvious treatment of choice.
Figures 28A, B
44 yo female patient suffering from Moderate OSA subsequent to adolescent retractive orthodontic treatment with removal of four bicuspid teeth. Bicuspid spaces reopened completely in maxilla and partially in mandible completely eliminating OSA.

She had a history of previous orthodontic treatment as an adolescent with four bicuspid teeth having been removed as part of the treatment. We are strong advocates of reopening extraction spaces as part of the treatment so that the patient has a better chance of having their tongue properly positioned to the palate at rest. Without promising her that even one symptom would be relieved, we started her on a protocol we have developed to reopen the extraction spaces in the maxilla, but not in the mandible. She agreed that orthognathic surgery should be part of the treatment plan from the beginning. By not opening bicuspid spaces in the mandibular arch we kept the lower incisors more retruded, which would allow for a larger surgical advancement of the mandible. A larger mandibular advancement would produce a greater increase in the Posterior Airway Space (distance between back of tongue and back of throat). She agreed to the treatment approach.
During the treatment, she obtained several surgical opinions since all the surgeons she saw diagnosed her with severe degenerative joint disease and recommended total joint replacement. She didn’t want to undergo surgery, but continued the treatment plan hoping for some miracle. In the midst of our reopening the extraction spaces only in the maxillary arch she started to sleep better. Without consulting us, she decided to have another sleep test done and found that she was completely free of OSA. A portion of the sleep report signed by the M.D. sleep physician follows:
“(Patient name) had mild obstructive sleep apnea-hypopnea syndrome with an REM dominant component. Her sleep apnea has completely resolved with orthodontic therapy – despite the 10+ pounds of interim body weight gain. It is quite remarkable how much improvement she has had in her apnea severity despite the presence of a large tongue and crowded oropharynx.”
Having completely eliminated her OSA problem, the patient wanted to terminate the treatment even though she had a poor bite relationship. We were able to convince her to allow us to open some space in the lower arch to reduce her overjet. After a very short time she terminated the treatment. The door was left open for her to do orthognathic surgery in the future if she changed her mind.
The significance of this case is that by merely opening a 7 mm space in each upper buccal segment for placement of an implant, her tongue gained enough space to be positioned upward and forward so that she was declared free of OSA by her sleep physician. She had undergone no myofunctional therapy, which might have had an additional benefit in helping her have proper rest position of the tongue to the palate. Her tongue had spontaneously found enough space in the palate to move upward and forward to eliminate her OSA. It is clear that we simply do not know where the threshold exists for OSA.
AIRWAY-kening™ Class II Camouflage Treatment
Camouflage treatment of Class II cases has long been a part of traditional orthodontic treatment. Such treatment involves retracting the upper anterior teeth after the removal of the upper first bicuspid teeth. More recently temporary anchorage devices (TAD’s) have been used to retract the maxillary anterior teeth and extraction of the first bicuspid teeth is avoided. This approach takes an already deficient maxilla and makes it more deficient. It damages the face and decreases the airway. In no way can it still be justified.
Figures 29A, B and C is the case of a 40-year-old female who merely wanted her teeth straightened. She sought the services of a local orthodontist in her area who recognized that she had a Class II malocclusion with little or no lower crowding. He did NOT offer her the option of surgery to advance the mandible. Instead he offered her the camouflage treatment of removing her upper right and left first bicuspid teeth to allow him to retract her six anterior teeth and reduce the overjet. The goal was no overjet with proper cuspid and incisal guidance long advocated by the profession.
Figures 29A, B, C
40 yo female patient had maxillary right and left first bicuspid teeth extracted and her overjet completely eliminated by retraction when she presented for a second opinion. She had developed severe pain in the TMJ’s, an inabiity to breathe, and OSA Patient reported, “I thought I was going to die”. Fig. 29B shows result of approximately 3 months of upper sagittal appliance wear to
re-advance the six maxillary anterior teeth and produce a slight overjet. The pain, breathing, and OSA problems were eliminated. Fig. 29C shows her ready to have braces removed having received approval from an implant surgeon and restorative dentist.

During the treatment she began to experience severe symptoms. She had trouble breathing and sleeping. She developed a severe pain pattern in the muscles of her face and around her TMJ’s. She would awaken in the night in a sweat with panic attacks thinking that she was going to die. She brought this problem to the attention of her orthodontist but he said the problem was unrelated to what he was doing and she would get used to it. She consulted with pain specialists in a large city near her home and was told there was no physical problem that could be identified. Deep inside she suspected that the retraction of her front teeth was causing the sleep and pain problem. She convinced her orthodontist to remove the upper arch wire which was continuing to retract her teeth. He reluctantly did so because she insisted. Within two hours she found her pain pattern subsiding, but the sleep problem persisted.
She presented to us in a panic mode thinking that she was going to die. We found all of the muscles of her face and neck to be extremely tender to palpation. There was no clicking in her joints, but her maxillary anterior teeth had been retracted so much that they were hitting traumatically with the lower incisors and causing distal pressure into the TMJ’s. Her clenching pattern was an unconscious effort to push the anterior teeth forward and free her mandible from being trapped by the maxillary anterior teeth. We did not promise reduction or elimination of even one symptom, but did promise to do our best. A maxillary sagittal appliance was used to reopen her extraction spaces. She wore it and activated it as instructed. The spaces opened as predicted. She returned to our office in four months with the extraction spaces more than halfway reopened. Her symptom pattern had been completely eliminated. The pain was gone and she was sleeping like she did before her retractive treatment. The final gallery shows treatment complete but with braces still in place.
Some may argue that this is a single example of one case and does not occur all that often. The fact is that it is NOT an uncommon occurrence with this treatment approach. Unfortunately, both the orthodontic profession and the public are largely unaware of a connection between retraction and symptom patterns. With the internet, many more patients are realizing the connection and that treatment to resolve the problem may be available. Some orthodontists are beginning to understand this connection and no longer feel comfortable doing this retractive treatment. Ideally this process would happen much faster so fewer will suffer.
AIRWAY-kening™ Surgical Correction of OSA with Double Jaw Advancement Surgery
When more conservative measures are ineffective, the ultimate correction for OSA is surgery. When the word “surgery” is used in most sleep clinic settings it refers to UPPP 45,32 (Uvulopalatopharyngeoplasty), which does not enjoy a great track record of success and isn’t without serious negative consequences. Other surgical procedures to the nasal or pharyngeal airway itself can be considered but none have a great chance of success. Such procedures as straightening a deviated septum, reducing turbinates, removing nasal polyps, etc., can improve the nasal airway. Whereas they may benefit the nasal airway, they do nothing to open the airway in the soft palate or base of the tongue areas where occlusion of the airway in OSA is often the critical issue.
The greatest chance of success in eliminating OSA surgically comes from surgery to advance both the maxilla and the mandible. It must be done with careful preparation for the outcome to be ideal. Orthodontic preparation of the arches is of paramount importance. Orthodontics should be part of the treatment in every case. The lower arch must be developed laterally in all cases so that the maxillary arch can be expanded to maximum dimension. Mew 8 indicates that an intermolar width of 42 mm between the maxillary molars is necessary for the tongue to be permanently postured to the palate at rest. Getting the patient to adopt such proper rest oral posture is critical for optimizing success in treating OSA. Figure 30 shows a 55-year-old male who had undergone double jaw advancement surgery without orthodontics in an effort to resolve his OSA. His intermolar width was about 30 mm. A PSG done months after the surgery showed that he still suffered from OSA. Had the patient undergone orthodontics to widen the mandibular arch and ultimately have the maxillary arch surgically expanded to the expanded lower arch the OSA might well have been eliminated.
Figure 30
Patient had undergone double jaw surgery to advance maxilla and mandible to eliminate OSA without any orthodontic preparation. OSA persisted. Had orthodontics been done pre-surgically to expand the mandibular arch, the maxilla could have been expanded surgically improving the likelihood of eliminating OSA.

Surgery to advance the mandible almost always needs to be done with a counterclockwise rotation of the occlusal plane. Such a rotation brings the mandible forward maximally with the projection of the bony chin optimized. Because the genioglossus muscle is attached to the lingual aspect of the mandible at the bony chin, the tongue advancement is optimized when surgery is done in this fashion. Most surgeons doing mandibular advancement surgery today are not doing this. Figures 31A and B show a 62-year-old male who had pre-surgical orthodontics to broaden the lower arch and underwent surgery to expand the maxilla to the widened mandibular arch and advance both jaws with a counterclockwise rotation. After years of suffering fatigue from untreated OSA, having both jaws advanced surgically has allowed him to go on to lead a normal life with renewed interest in skiing and other outdoor sports. The airway improvement produced with proper advancement of both jaws is dramatic. His sleep physician performed a PSG to confirm that he no longer suffers from OSA and commented that, “You have an airway like a wind tunnel”.
Figures 31A, B
62 yo male patient presented with severe fatigue and OSA. Pre-surgical orthodontics broadened the lower arch allowing the maxilla to be expanded at the time of surgery. Both jaws were advanced massively with a counterclockwise rotation of the occlusal plane to maximally advance the genioglossus muscle. The improvement in the airway eliminated his OSA and caused the sleep physician to remark, “You have an airway like a wind tunnel!”.

Orthognathic surgery to advance both jaws can be a very successful approach to treating OSA sufferers if it is planned properly, prepared for properly orthodontically, and executed properly by a surgeon who understands how to advance the jaws for optimal esthetics and airway. Patients who finally are free of OSA often awake in recovery and say, “I can breathe!” like they had never taken a breath before in their life. Many also indicate dramatically improved brain function when they are finally sleeping normally and are getting proper oxygenation.
Palliative Solutions
Managing patients airway problems with oral appliances can be very helpful and is now becoming a focus of many dentists. Unfortunately, such treatment is more of a “Band Aid” solution. It is not a permanent “fix” of the problem. Mandibular Advancement Devices (MAD’s) which posture the mandible forward can open the airway enough to reduce the AHI in many mild or moderate OSA sufferers. Unfortunately, over time all have a headgear effect of retracting the maxilla and ultimately will become less effective. Figure 32 shows an OSA sufferer who had a normal occlusion before wearing a MAD for many years. The headgear effect of that appliance produced the end-to-end incisor relationship and open-bite. Patients need to be warned of such bite changes and reduced effectiveness over time.
Figure 32
This patient wore a MAD (Mandibular Advancement Device) for OSA for several years causing the maxilla to be retracted with a “headgear effect” and producing an open-bite. The appliance became less effective in reducing the OSA.

CPAP is the gold standard of OSA treatment. CPAP is the treatment of choice in cases of mild to severe OSA when a MAD is not effective. Sadly, CPAP does not enjoy a high rate of compliance long term. It can also have a headgear effect of driving the maxilla distally. Figure 33A shows a male prior to his wearing a CPAP for about 10 years. He began with a perfect Class I occlusion but the headgear effect retracted the maxilla to the illustrated bite relationship in Figure 33B. The CPAP became largely ineffective after this occurred. Maxillomandibular advancement surgery was the only solution to his problem.
Figures 33A, B
47 yo male with normal bite relationship prior to CPAP treatment. Fig. 33B After approximately 10 years of CPAP therapy an anterior crossbite was produced and CPAP was no longer effective. Maxilla-mandibular advancement surgery was recommended to treat his OSA.

Alternatives to Palliative Treatment
There will always be a place for palliative treatment of OSA. Many health care issues do not have “solutions” and the best option is some form of palliative treatment. However, the prevention of the problem is the option that really makes sense. Myofunctional therapy to teach children to have their tongue to the palate, teeth touching lightly and lips together breathing through the nose would ideally become the standard and would eliminate many of the orthodontic and breathing issues children present with today. Optimizing forward facial development as early as possible in growing children has been shown to improve the airway short term. 34 Surely optimizing the forward facial development and keeping that development will have long term benefits. This is a great subject for future research.
Dentistry…the Gateway to the Airway
Dentists have been given a gift and responsibility to manage the airway. Most are completely unaware that the decisions made regarding treatment for malocclusions can have a positive or negative effect on the airway. We need to become aware of this critical role we have been given and shoulder the responsibility of addressing these problems in a way that reflects the life and death importance of optimizing airways.
As with any problem, it is obvious that the earlier the treatment is done the easier it is and the better the outcome. Nevertheless, the profession needs to be ready to effectively help patients of any age with treatment modalities which are predictable and have a high chance of success in resolving the problems related to airway inadequacy. Exciting times lie ahead for the profession, but dramatic changes must be made. Retraction in any form must end. This requires a complete change in the orthodontic profession because many (if not most) treatment plans are retractive in nature. A complete discussion of these treatment plan changes is in an article by Hang and Gelb. 47 Orthodontic research to find better ways to help patients develop their faces forward must replace research on how to straighten teeth more efficiently and effectively to the “Gold Standard” Class I occlusion, without regard to the position of the jaws in the face or to the airway. Orthodontists must embrace the goal of optimizing airway for all if the profession is to escape the often-cited image of being “oral cosmetology”, and take its rightful place in the health care profession with AIRWAY-kening™ treatments. OH
Oral Health welcomes this original article.
References
- Schwartz, AR, Patil SP, Laffan AM, Polotsky V, Schneider H, and Smith PL Obesity and Obstructive Sleep Apnea Pathogenic Mechanisms and Therapeutic Approaches. Proceedings of the American Thoracic Society. 2008; Vol. 5, No. 2.
- Romero-Corral A, Caples, S M, Lopez-Jiminez, F, Somers V K Interactions Between Obesity and Obstructive Sleep Apnea. Chest. 2010 Mar; 137(3) 711-719.
- Durán J, Esnaola S, Rubio R, Iztueta A Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001 Mar; 163(3 Pt 1):685-9.
- Resta O, Foschino-Barbaro MP, Legari G, Talamo S, Bonfitto P, Palumbo A, Minenna A, Giorgino R, De Pergola G Sleep-related breathing disorders, loud snoring and excessive daytime sleepiness in obese subjects. Int J Obes Relat Metab Disord. 2001 May; 25(5):669-75.
- Fritscher LG, Mottin CC, Canani S, Chatkin JM Obesity and obstructive sleep apnea-hypopnea syndrome: the impact of bariatric surgery. Obes Surg. 2007 Jan; 17(1):95-9.
- Wolk R, Somers VK Obesity-related cardiovascular disease: implications of obstructive sleep apnea. Diabetes Obes Metab. 2006 May; 8(3):250-60.
- Peppard PE, Young T, Palta M, Dempsey J, Skatrud J 7 Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000 Dec 20; 284(23):3015-21.
- Mew J. The cause and cure of malocclusion. Heath eld: John Mew; 2013.
- Remmers, J Personal Communication, Canadian AACP meeting, Vancouver, B.C. November 2016.
- Hatcher DC Cone Beam Computed Tomography: Craniofacial and Airway Analysis. Sleep Medicine Clinics, Vol. 5 Number 1, 3010.
- Price W A Nutrition and Physical Degeneration. Price Pottenger Nutrition Foundation 1-28-2008 Eighth Edition.
- Catlin G Shut Your Mouth and Save Your LIfe. London: Trubner & Co., 57&59 Ludgate Hill, 1882.
- Pottenger FM Pottenger’s Cats: A Study in Nutrition. Price-Pottenger Nutrition Foundation 1983.
- Corruccini RS. How Anthropology Informs the Orthodontic Diagnosis of Malocclusion’s Causes. Lewiston, NY: The Edwin Mellen Press; 1999.
- Lieberman D. The evolution of the human head. Cambridge: Belknap Press of Harvard University Press; 2011.
- Harvold, EP, Tomer BS, Vargervik K, Chierici, G. Primate experiments of oral respiration. AJO. 1981;79: 359-372.
- Gelb M. Airway centric TMJ philosophy. CDA J. 2014;42:551–562.
- Cistulli PA, Palmisano RG, Poole MD Treatment of obstrutive sleep apnea syndrome by rapid maxillary expansion. Sleep. 1998 Dec 15 (8): 831-5.
- Tsuiki S, Maeda K, Inoue Y, Rapid maxillary expansion for Obstructive Sleep Apnea: A lemon for lemonade? J Clin Sleep Med. 2014 Feb 15; 10(2): 233.
- Pirelli P, saponara M, Guilleminault C. Rapid maxillary expansion (RME) for pediatric obstructive sleep apnea: a 12-year follow-up. Sleep Medicine August 2015 Vol. 16, Issue 8: 933-931.
- Guilleminault C, Sullivan S. Towards restoration of continuous nasal breathing as the ultimate treatment goal in pediatric obstructive sleep apnea. Enliven: Pediatr Neonatol Biol. 2014;1(1):1–5.
- Guilleminault C, Huang YS, Monteyrol PJ, Sato R, Quo S, Lin CH. Critical role of myofascial reeducation in pediatric sleep disordered breathing. Sleep Med. 2013 Jun;14:518–525.
- McNamara JA Jr. Components of class II malocclusion in children 8–10 years of age. Angle Orthod. 1981;51:177–202.
- Primozic J, Farcnik F, Perinetti G, Richmond S, Ovsenik M. The association of tongue posture with the dentoalveolar maxillary and mandibular morphology in Class III malocclusion: a controlled study. Eur J Orthod (2013) 35 (3): 388-393.
- Ang Q, Jia P, Anderson N, Wang L, Lin J. Changes of pharyngeal airway size and hyoid bone position following orthodontic treatment of Class I bimaxillary protrusion. Angle Orthod. 2012;82:115–121.
- Chen Y, Hong L, Wang C, Zhang S, Cao C, Wei F, LV T,Zhang F, Liu D Effect of large incisor retraction on upper airway morphology in adult bimaxillary protrusion patients. Three-dimensional multislice computed tomography registration evaluation. Angle Orthod, 2012 Vol 82, No 6.
- Germec-Cakan D, Taner T, Akan S. Uvulo-glossopharyngeal dimensions in non-extraction, extraction with minimum anchorage, and extraction with maximum anchorage. European Journal of Orthodontics Nov 2010: 33(2011) 515-520.
- Pancherz H, Ruf S. The Herbst appliance: research-based clinical management. Chicago, IL: Quintessence Pub ; 2008.
- Berkman ME, Haerian A, McNamara JA Jr Interarch Maxillary Molar Distalization Appliances for Class II Correction. J Clin Orthod. 2008;42:35-42.
- Ishaq RAR, AlHammadi MS, Fayed MMS, El-Ezz AA, Mostafa Y. Fixed funtional appliances with multi bracket appliances have no skeletal effect on the mandible: A systematic review and meta-analysis. Am J Orthod Dentofacial Ortho 2016; 149:612-624.
- Gozal, D Lecture to American Academy of Craniofacial Pain.
- Harper R, Kumar R, Ogren JA, Macey PM. Sleep-disordered breathing: Effects on brain structure and function. Respir. Physical.Neurobiol 2013.
- Cooper PW Jr. Why? African American Children Can Not Read 2009i Universe, Inc Bloomington, NY.
- Singh GD, Medina LE, Hang WM. Soft tissue facial changes using biobloc appliances: geometric morphometrics. Int J of Orthod. 2009;20:29–34.
- Johnston LE. Growing jaws for fun and profit. What doesn’t and why. In: McNamara, (ed.) Craniofacial growth series 35. Center for Human Growth and Development. Ann Arbor: University of Michigan; 1999.
- Artun J, Grobety D. Periodontal status of mandibular incisors after pronounced orthodontic advancement during adolescence: a follow-up evaluation. AJO-DO. 2001;119:2–10.
- Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: a retrospective study of adult orthodontic patients. AJO-DO. 2005;127:552–561.
- Azia T, Flores-Mir C. A systematic review of the association between appliance-induced labial movement of mandibular incisors and gingival recession. Just Orthod J. 2011;May:27(1):33-9.
- Kasha A. Gingival recession and labial movement of lower incisors. Enid Based Dent 2013 Mar;14(1):21-2.
- Renkema AM, Navratilova Z, Mazurka K, Katsaros C, Fudalej PS. Gingival labial recessions and the post-treatment proclamation of mandibular incisors. Our J Orthod. 2015 Oct;37(5):508-13.
- Ruf S, Hansen K, Panthers H. Does orthodontic proclination of lower incisors in children and adolescents cause gingival recession? Am J Orthod Ortho. 1998 Jul;114(1):100-6.
- Morris JW, Campbell PM, Tadlock LP, Boley J, Buschang PK. Prevalence of gingival recession after orthodontic tooth movements Am J Orthod Ortho. 2017 May;151(5):851-859.
- Biggerstaff RH The orthodontic management of congenitally absent maxillary later incisors and second premolars: A case report. Am J Orthod Ortho. 1992 Dec;102 (6):537-545.
- Remmers J. J Personal Communication, Canadian AACP meeting, Vancouver, B.C. November 2016.
- Braga A, Grechi TH, Eckeli A, et al. Predictors of uvulopalatopharyngoplasty success in the treatment of obstructive sleep apnea syndrome. Sleep Medicine. 2013 Dec;14(12):1266-71.
- Caples SM, Rowley JA, Prinsell JR, Pallanch JF, Elamin MB, Katz SG, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010 Oct;33(10):1396-407.
- Hang W, Gelb M. Airway Centric® TMJ philosophy/Airway Centric® orthodontics ushers in the post-retraction world of orthodontics. Cranio. 2017 March; Vol. 35(2) 68-78.
About the Author
 Early in his career Dr Hang saw serious limitations in esthetics and function with traditional orthodontics. He learned and developed innovative techniques to protect and enhance the airway while enhancing ethetics and function. He treats all ages including children beginning at age 3, adults who have had teeth extracted for orthodontics and suffer from E.R.R.S.™ (Extraction Retraction Regret Syndrome™), and OSA patients. Dr. Hang has spoken on orthodontics, facial esthetics and airway locally, nationally, and internationally. He was awarded the AAPMD Lifetime Achievement Award in 2016 for his contribution to the field of airway orthodontics.
Early in his career Dr Hang saw serious limitations in esthetics and function with traditional orthodontics. He learned and developed innovative techniques to protect and enhance the airway while enhancing ethetics and function. He treats all ages including children beginning at age 3, adults who have had teeth extracted for orthodontics and suffer from E.R.R.S.™ (Extraction Retraction Regret Syndrome™), and OSA patients. Dr. Hang has spoken on orthodontics, facial esthetics and airway locally, nationally, and internationally. He was awarded the AAPMD Lifetime Achievement Award in 2016 for his contribution to the field of airway orthodontics.
RELATED ARTICLE: Tips for Discussing Orthodontic Treatment with Patients
Follow the Oral Health Group on Facebook, Instagram, Twitter and LinkedIn for the latest updates on news, clinical articles, practice management and more!












